Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Dec 21, 2013; 19(47): 9084-9091
Published online Dec 21, 2013. doi: 10.3748/wjg.v19.i47.9084
Published online Dec 21, 2013. doi: 10.3748/wjg.v19.i47.9084
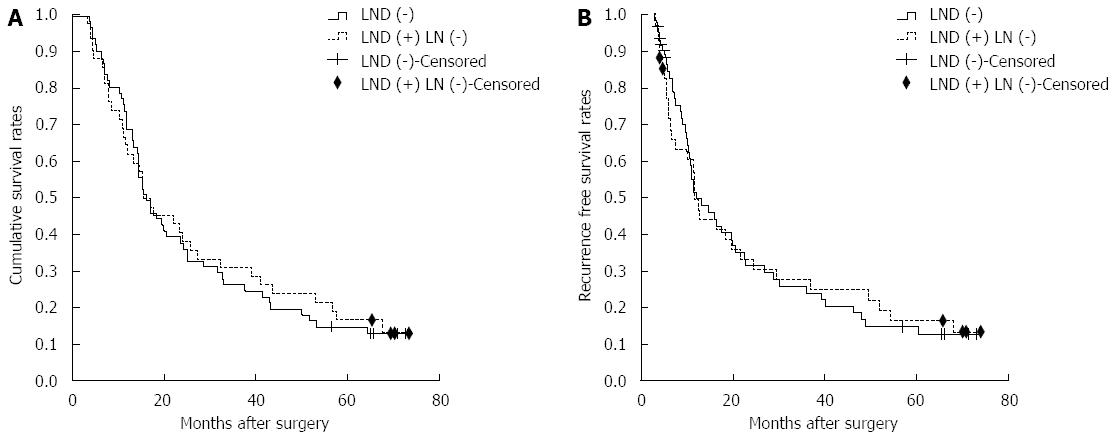
Figure 1 Overall survival and recurrence-free survival curves of intrahepatic cholangiocarcinoma patients without lymph node involvement.
A: Survival curves of patients in the lymph node dissection (LND) (-) and LND (+) LN (-) groups. There is no significant survival difference between the two groups (P = 0.822). The censored represented the cases who were still alive at the endpoint; B: Recurrence-free survival curve of patients in LND (-) and LND (+) LN (-) groups. There is no significant survival difference between the two groups (P = 0.970). The censored represented the cases who were still alive at the endpoint or died for other reasons instead of tumor recurrence.
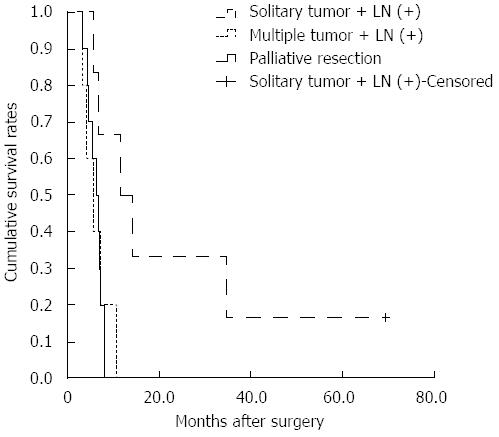
Figure 2 Survival curves of patients in the palliative resection and lymph node dissection (+) lymph node (+) groups.
There are significant differences between the palliative resection group and patients with lymph node (LN) involvement and a solitary tumor (P = 0.013). There are no significant differences between the palliative resection group and patients with LN involvement and multiple tumors (P = 0.744).
- Citation: Li DY, Zhang HB, Yang N, Quan Y, Yang GS. Routine lymph node dissection may be not suitable for all intrahepatic cholangiocarcinoma patients: Results of a monocentric series. World J Gastroenterol 2013; 19(47): 9084-9091
- URL: https://www.wjgnet.com/1007-9327/full/v19/i47/9084.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i47.9084