Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 14, 2013; 19(42): 7231-7240
Published online Nov 14, 2013. doi: 10.3748/wjg.v19.i42.7231
Published online Nov 14, 2013. doi: 10.3748/wjg.v19.i42.7231
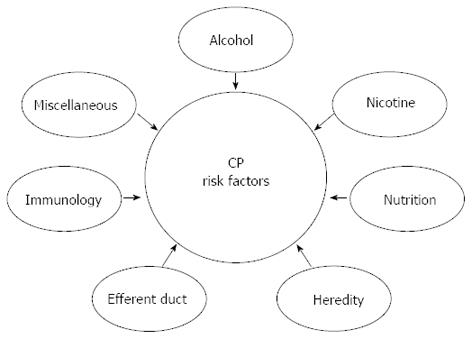
Figure 1 The etiological risk-factors associated with chronic pancreatitis are multiple and involve both genetic and environmental factors.
According to the M-ANNHEIM classification system, different synergistic risk factors are known such as: alcohol-consumption, nicotine-consumption, nutritional factors, hereditary factors, efferent duct factors, immunological factors and miscellaneous and rare metabolic factors. CP: Chronic pancreatitis.
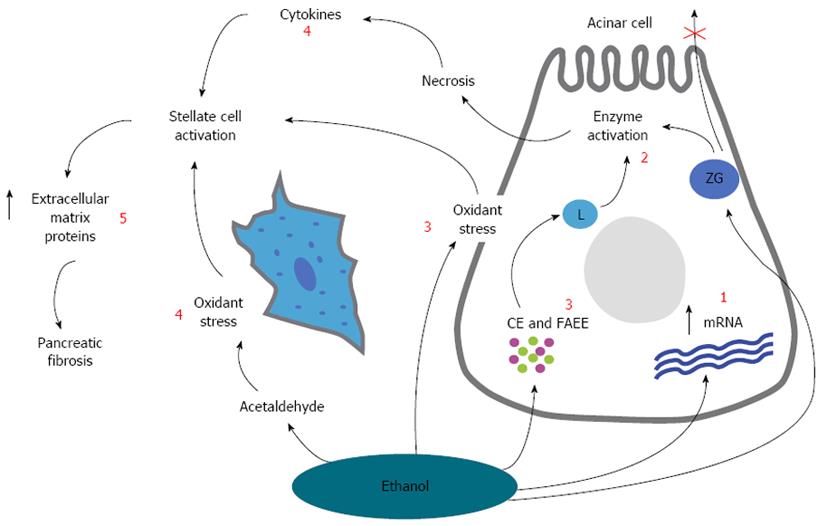
Figure 2 A schematic overview showing the overall hypothesis for the pathogenesis of alcoholic chronic pancreatitis.
The effect of ethanol and its metabolites on the subcellular organelles include increased digestive and lysosomal enzyme content [due to increased synthesis (increased mRNA) and impaired secretion (1)] and destabilization of lysosomes (L) (2) and zymogen granules (ZG) [mediated by oxidant stress, cholesteryl esters (CE) and fatty acid ethyl esters (FAEE) (3)]. These changes will make the cell more sensitive to trigger factors and in the presence of appropriate trigger factors, overt acinar cell injury is initiated (alcoholic acute pancreatitis). Pancreatic stellate cells are activated by cytokines during alcohol-induced necroinflammation, or directly by ethanol via its metabolism to acetaldehyde and the subsequent generation of oxidant stress (4). Activated pancreatic stellate cell then increases the synthesis of extracellular matrix proteins leading to pancreatic fibrosis. Modified from Vonlaufen et al[84] (5).
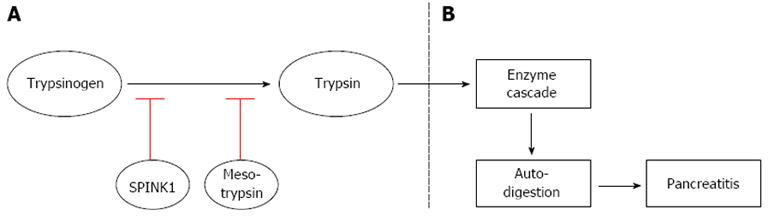
Figure 3 A scheme representing the role of digestive enzymes in normal pancreatic tissue and in the case of pancreatitis.
A: In a normal pancreas, SPINK1 (first line of defense) and mesotrypsin (second line of defense) inhibit the generation of trypsin resulting from auto-activation of trypsinogen. These defense mechanisms prevent the pancreas from activating the pancreatic enzyme cascade and auto-digestion; B: If mutations are present in the SPINK1 and/or in the mesotrypsin gene, they losses their ability to inhibit the generation of trypsin resulting in activation of enzyme cascade and subsequent pancreatic auto-digestion leading to pancreatitis. SPINK1: Serine protease inhibitor, kazal type 1, gene (encodes for pancreatic secretory trypsin inhibitor).
- Citation: Brock C, Nielsen LM, Lelic D, Drewes AM. Pathophysiology of chronic pancreatitis. World J Gastroenterol 2013; 19(42): 7231-7240
- URL: https://www.wjgnet.com/1007-9327/full/v19/i42/7231.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i42.7231