Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 28, 2013; 19(4): 528-535
Published online Jan 28, 2013. doi: 10.3748/wjg.v19.i4.528
Published online Jan 28, 2013. doi: 10.3748/wjg.v19.i4.528
Figure 1 Endoscopic treatment room (A) and treatment procedures (B) of the Shirakawa Clinic.
The treatment team included two doctors [one operator (1) and one doctor to administer propofol sedation (2)], two nurses who care for the patients (3) and two endoscopical technicians (not in photo). 4: Vital sign monitor.
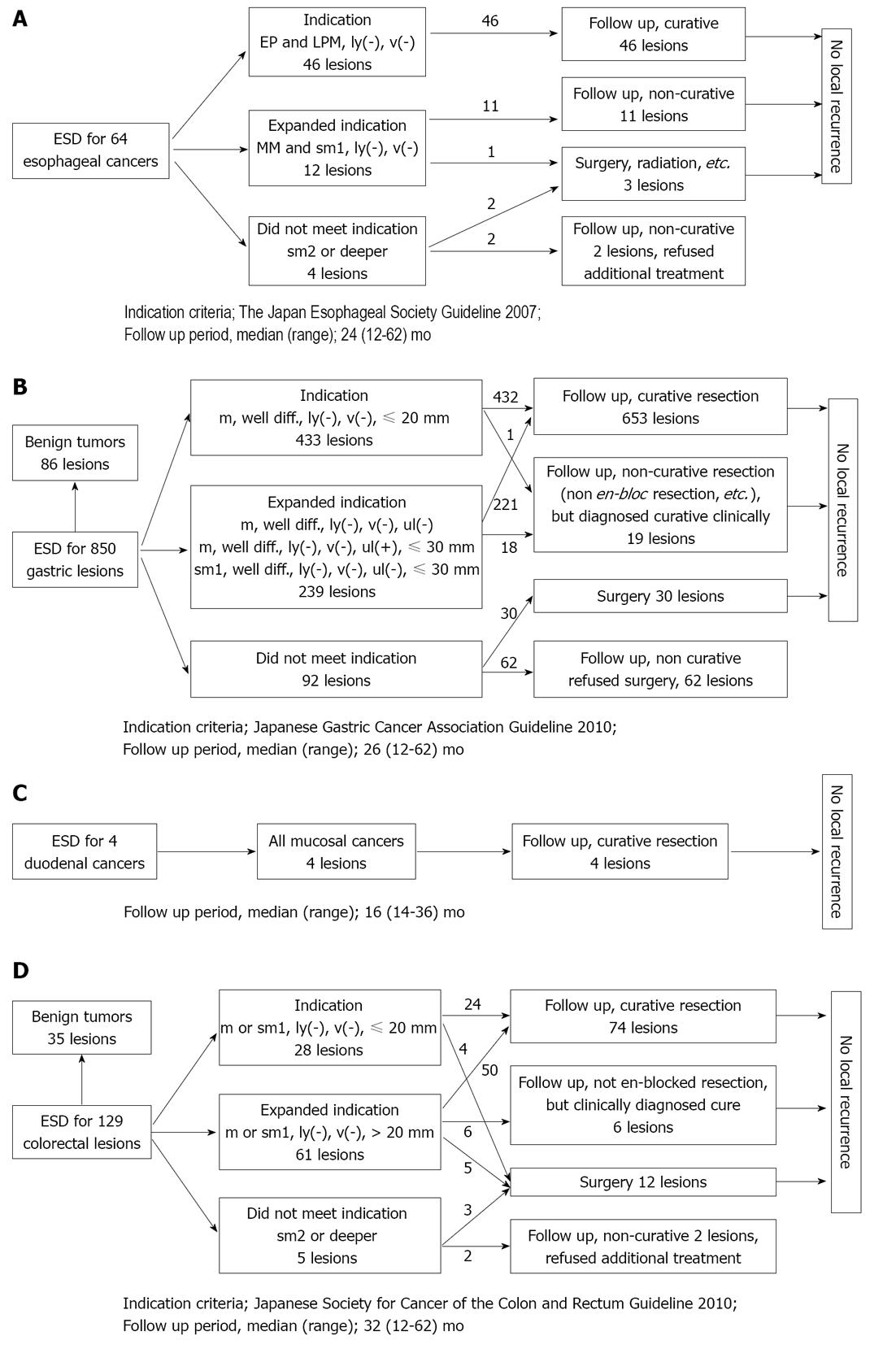
Figure 2 The clinical courses after the endoscopic submucosal dissection of esophageal cancers (A), gastric lesions (B), duodenal cancers (C) and colorectal lesions (D).
ESD: Endoscopic submucosal dissection; EP: Epithelium; MM: Muscularis mucosae; LPM: Lamina propria mucosae; Well diff.: Well differentiated adenocarcinoma.
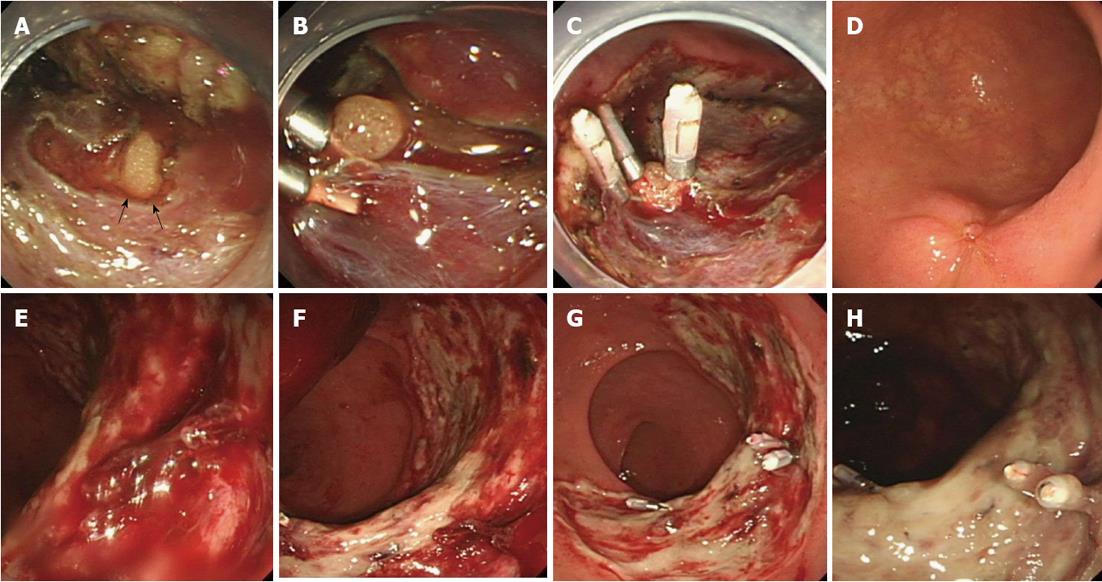
Figure 3 Representative cases of perforation and bleeding treated endoscopically.
A: A perforation was detected (arrows); B: When the omentum became visible through the perforation hole, we attempted to aspirate the omentum through the perforation hole, then clipped the gastric wall and omentum together; C: Several clips were used to seal the hole completely; D: The appearance three months after clipping; E: Bleeding from a post-endoscopic submucosal dissection ulcer was detected; F: After removing the coagulation, the bleeding point was detected; G: Clips were used to achieve hemostasis endoscopically; H: The appearance 1 wk after clipping.
- Citation: Sohara N, Hagiwara S, Arai R, Iizuka H, Onozato Y, Kakizaki S. Can endoscopic submucosal dissection be safely performed in a smaller specialized clinic? World J Gastroenterol 2013; 19(4): 528-535
- URL: https://www.wjgnet.com/1007-9327/full/v19/i4/528.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i4.528