Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Jul 7, 2013; 19(25): 4031-4038
Published online Jul 7, 2013. doi: 10.3748/wjg.v19.i25.4031
Published online Jul 7, 2013. doi: 10.3748/wjg.v19.i25.4031
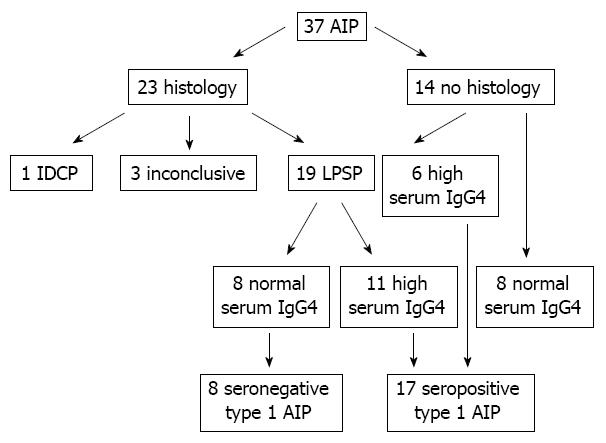
Figure 1 Enrolled patients and classification of autoimmune pancreatitis.
Among 37 patients with autoimmune pancreatitis (AIP), one case was type 2 AIP and 19 patients were type 1 AIP by histology. The pathological diagnosis was inconclusive in three cases among 23 tissue samples. Among 14 patients without histology, eight patients were excluded because of normal serum immunoglobulin G4 (IgG4) levels. Ultimately, 25 patients with definite type 1 AIP (19 histologically and six serologically diagnosed cases) were enrolled in this study. LPSP: Lymphoplasmacytic sclerosing pancreatitis; IDCP: Idiopathic duct-centric chronic pancreatitis.
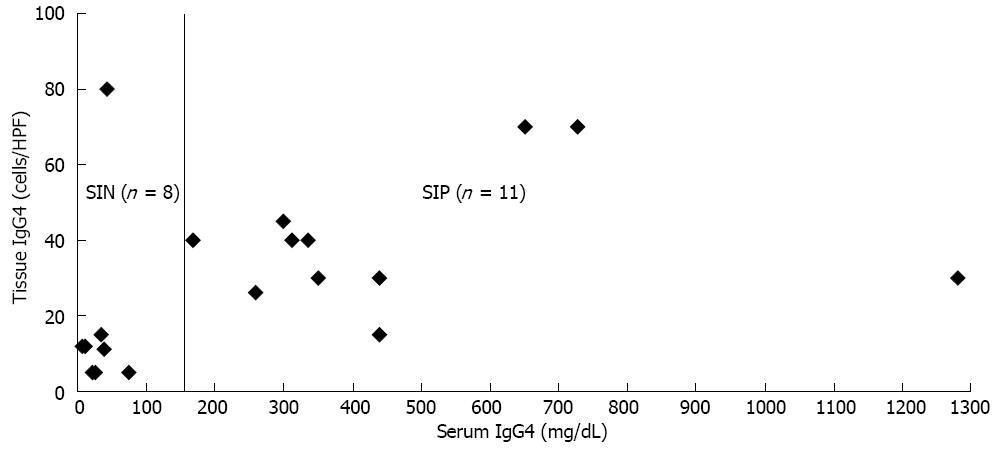
Figure 2 Correlation between serum and tissue immunoglobulin G4 concentrations.
Among eight serum immunoglobulin G4 (IgG4)-negative (SIN) patients, the tissue IgG4 concentrations were less than 15 cells per high power filed (HPF) in most of cases, except one. Among 11 serum IgG4-positive (SIP) patients, the tissue IgG4 concentrations were more than 25 cells per HPF, except one case (15 cells per HPF). There was no linear correlation between serum and tissue IgG4 concentration among the 11 SIP patients.
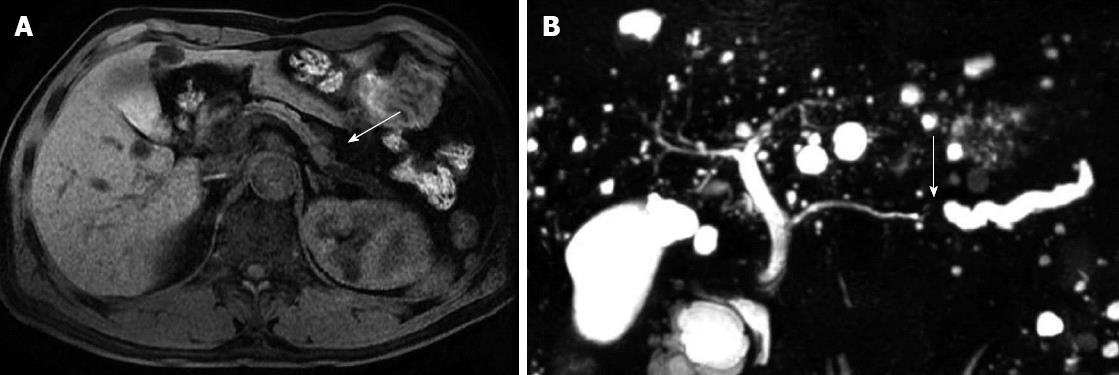
Figure 3 Magnetic resonance image of 61-year-old male patient with normal serum immunoglobulin G4.
A: Magnetic resonance image shows slightly exophytic mass of iso-attenuation at the body of pancreas; B: Distal parenchymal atrophy and abrupt cutting of pancreatic duct with upstream ductal dilatation.
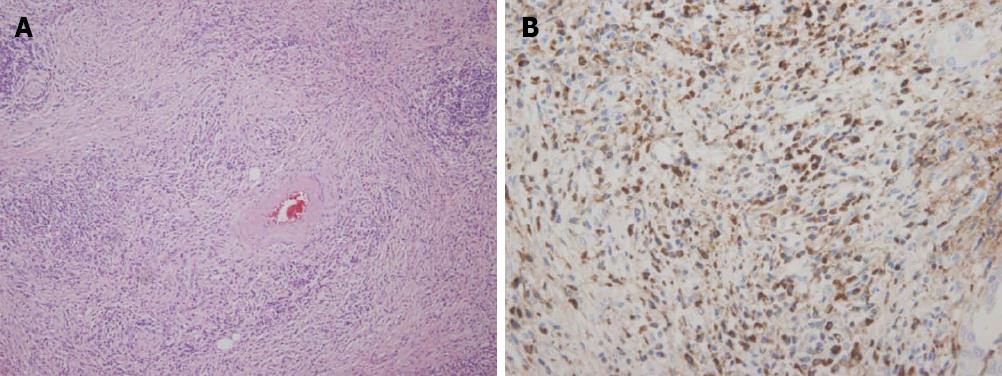
Figure 4 Histology and immunoglobulin G4 immunohistochemical staining.
A: Hematoxylin and eosin staining shows typical finding of lymphoplasmacytic sclerosing pancreatitis (× 200); B: Immunoglobulin G4 (IgG4) staining shows dense infiltration of IgG4 positive cells (× 400).
- Citation: Paik WH, Ryu JK, Park JM, Song BJ, Park JK, Kim YT, Lee K. Clinical and pathological differences between serum immunoglobulin G4-positive and -negative type 1 autoimmune pancreatitis. World J Gastroenterol 2013; 19(25): 4031-4038
- URL: https://www.wjgnet.com/1007-9327/full/v19/i25/4031.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i25.4031