Copyright
©2013 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 14, 2013; 19(2): 209-218
Published online Jan 14, 2013. doi: 10.3748/wjg.v19.i2.209
Published online Jan 14, 2013. doi: 10.3748/wjg.v19.i2.209
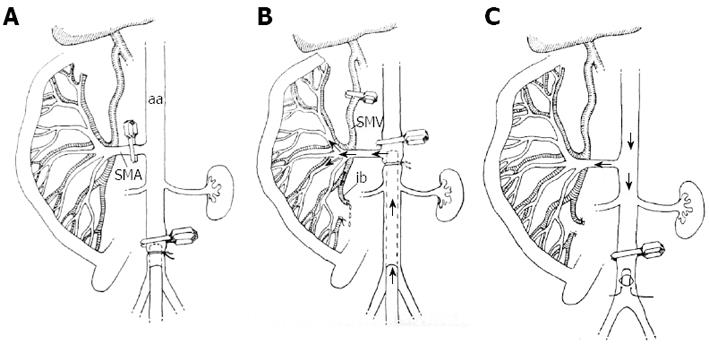
Figure 1 The sequential steps of the intestinal perfusion in vivo.
A: The abdominal aorta (aa) is occluded by a clip, followed by cannulation of the vessel; the superior mesenteric artery (SMA) is clipped; B: The aortic clip is positioned above the SMA; the cannula is positioned at the level of SMA to allow its perfusion with hypertonic saline; the perfusate outflow is secured through the opened ileocecal branch (ib) of the superior mesenteric vein (SMV); the main trunk of SMV is clipped; C: The cannula is removed to allow blood flow through the SMA to resume simultaneously with the following procedures: the aortic clip is positioned as in Figure 1A; the clip occluding the SMV is removed, and bleeding from the ileocecal branch of the SMV is prevented by ligation.
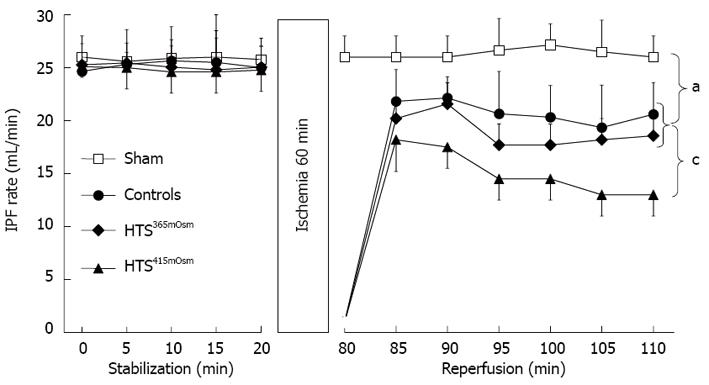
Figure 2 Intestinal perfusate flow rate in the ex vivo rat experiments with 60-min ischemia followed by varying conditions of reperfusion.
The groups tested were: sham-operated (no ischemia at all, n = 6); controls (30 min reperfusion with normotonic buffer, n = 5); 2 groups with either HTS365mOsm (n = 5) or HTS415mOsm (n = 5), both subjected to 5-min reperfusion with the respective hypertonic solution followed by 25 min reperfusion with normotonic buffer. The pre-ischemic values of Intestinal perfusate flow (IPF) rate were similar in all groups. No changes were apparent in the shams over the whole period, whereas IPF values were lower in all the ischemia-reperfusion groups, although the groups showed different patterns. HTS415mOsm resulted in the most prominent decrease in the IPF rate, with a further progressive fall to the end of the experiment. In contrast, IPF rate was less affected in the control and HTS365mOsm groups, to a similar degree in both, while an appreciable degree of stabilization took place towards the end of the postischemic period. Postischemic IPF rate recovery did not differ between the controls and the HTS365mOsm group, whereas postischemic IPF rate values were significantly lower in the HTS415mOsm group, compared to both the controls and the HTS365mOsm group. Data are mean ± SD. aP < 0.05 vs sham; cP < 0.05 vs controls.
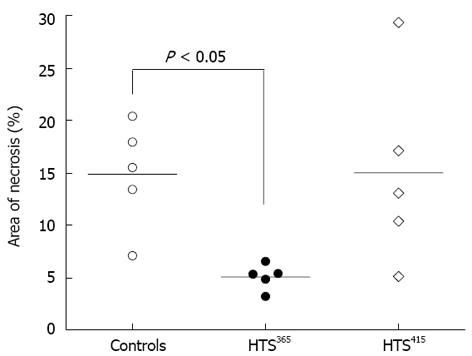
Figure 3 Area of necrosis within the isolated rat intestine after 60-min ischemia followed by the varying conditions of reperfusion.
The area of necrosis (AN) is defined as the percentage of 2.3.5-triphenyltetrazolium chloride-negative in relation to the total intestinal tissue volume. Controls (reperfusion with normotonic saline) and the HTS415mOsm group did not differ statistically regarding AN volume, whereas HTS365mOsm administration resulted in a significantly lower value of AN. In both hypertonic saline (HTS) groups, the 5-min reperfusion with the appropriate hyperosmotic saline was followed by 25-min normotonic reperfusion. The data are presented as dot plots with median values.
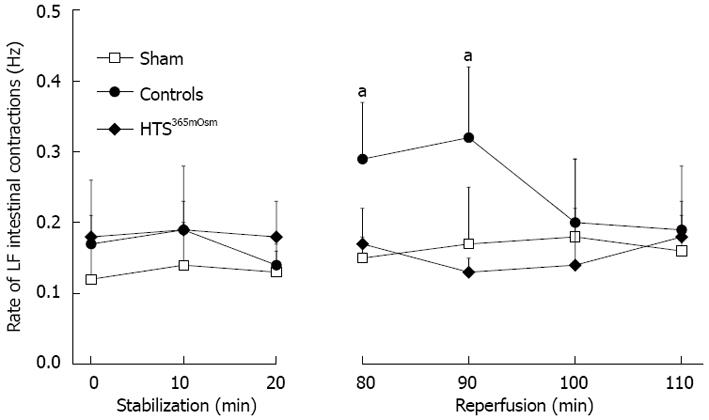
Figure 4 The rate of low frequency intestinal contractions in the ex vivo experiments.
In shams, the intestine was continuously perfused for 110 min. In controls (60-min ischemia followed by 30-min reperfusion), intestinal contraction rate was significantly higher over the initial 10 min of reperfusion in comparison with the shams. Intestinal reperfusion with hyperosmotic saline in the HTS365mOsm group prevented the increase in postischemic intestinal contraction rate. Data are mean ± SD. aP < 0.05 vs sham. LF: Low frequency.
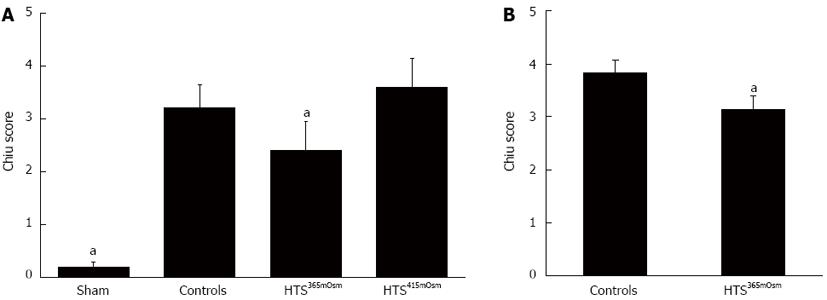
Figure 5 Histologically defined scores in the ex vivo (A) and in vivo (B) experiments.
A, B: In the sham group (no ischemia at all, A) slight injury only is evident, probably due to the prolonged perfusion in the extracorporeal environment. Sixty-minute ischemia followed by 30-min normotonic reperfusion (controls) resulted in a significant injurious effect, which, however, was substantially less expressed in the HTS365mOsm but not in the HTS415mOsm group. The analogous difference between the controls and the HTS365mOsm group is apparent in the in vivo experiments (B). The data are expressed as mean ± SD; aP < 0.05 vs controls.
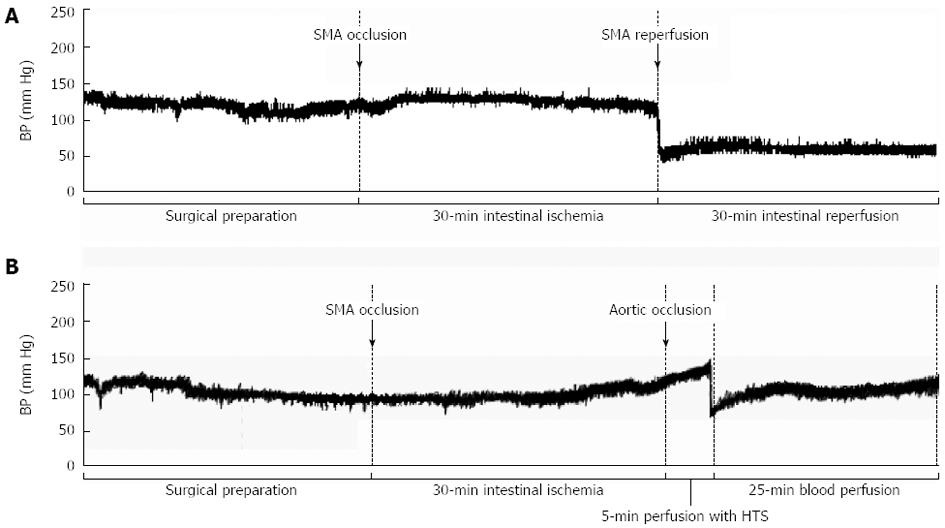
Figure 6 Representative samples of arterial blood pressure recordings in anesthetized rats subjected to intestinal ischemia-reperfusion in vivo.
A: Thirty-minute superior mesenteric artery (SMA) occlusion followed by 30-min reperfusion (controls) resulted in a persistent blood pressure (BP) decrease over the entire reperfusion period; B: Thirty-minute SMA occlusion finalized by aortic clamping followed immediately by 5-min SMA perfusion with hypertonic saline (365 mOsm/L), with a subsequent 25-min reperfusion with blood, resulted in a transient drop with a rapid restoration of BP up to the initial values. HTS: Hypertonic saline.
- Citation: Kornyushin O, Galagudza M, Kotslova A, Nutfullina G, Shved N, Nevorotin A, Sedov V, Vlasov T. Intestinal injury can be reduced by intra-arterial postischemic perfusion with hypertonic saline. World J Gastroenterol 2013; 19(2): 209-218
- URL: https://www.wjgnet.com/1007-9327/full/v19/i2/209.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i2.209