Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Dec 14, 2012; 18(46): 6720-6728
Published online Dec 14, 2012. doi: 10.3748/wjg.v18.i46.6720
Published online Dec 14, 2012. doi: 10.3748/wjg.v18.i46.6720
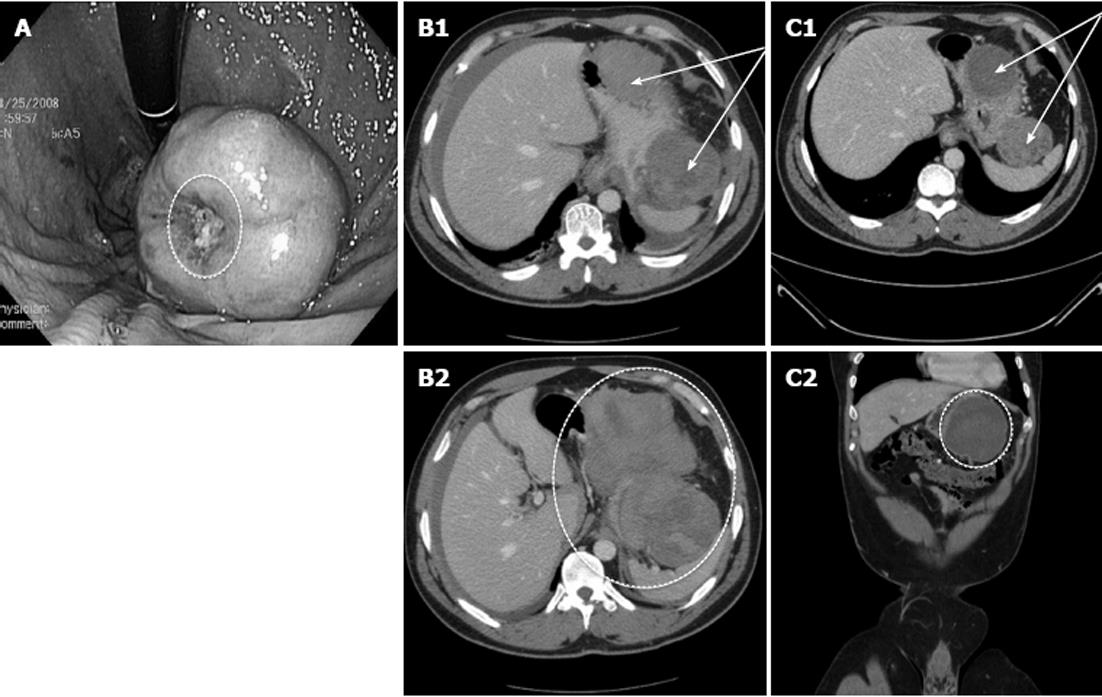
Figure 1 Clinical images of complicated gastrointestinal stromal tumors.
A: Large intraluminal gastric gastrointestinal stromal tumors (GIST) with punctate central ulceration. The bleeding ulcer was treated endoscopically with sclerotherapy and electrocautery (cauterized tissue; white oval). The patient had an interval resection electively without additional hemorrhage from the tumor; B: Acute presentation of a patient with a ruptured gastric GIST with hemoperitoneum. These images represent contrast-enhanced computed tomography (CT) scan from a patient with a large extraluminal gastric GIST along the greater curvature of the stomach. B1 demonstrates axial CT images of the bi-lobed tumor with irregular borders (arrows); B2 shows additional axial images at the caudal extent of gastric tumor with layering of blood in the splenic recess (oval). He was diagnosed with hemoperitoneum and was resuscitated with packed red blood cells, fresh frozen plasma, and platelets; the patient was on antiplatelet therapy at the time of admission. He stabilized and had an upper endoscopy/ultrasonography for tissue diagnosis and to plan definitive treatment; C: Ruptured gastric GIST following conservative management. Contrast-enhanced CT images following a six-week period of conservative management of the patient with ruptured gastric GIST. C1 demonstrates the more organized bi-lobed tumor with distinct borders (arrows); C2 shows coronal images of the organized hemorrhagic component within the splenic recess after a period of observation (oval). Ultimately this patient had an interval open subtotal gastrectomy for a high-grade GIST.
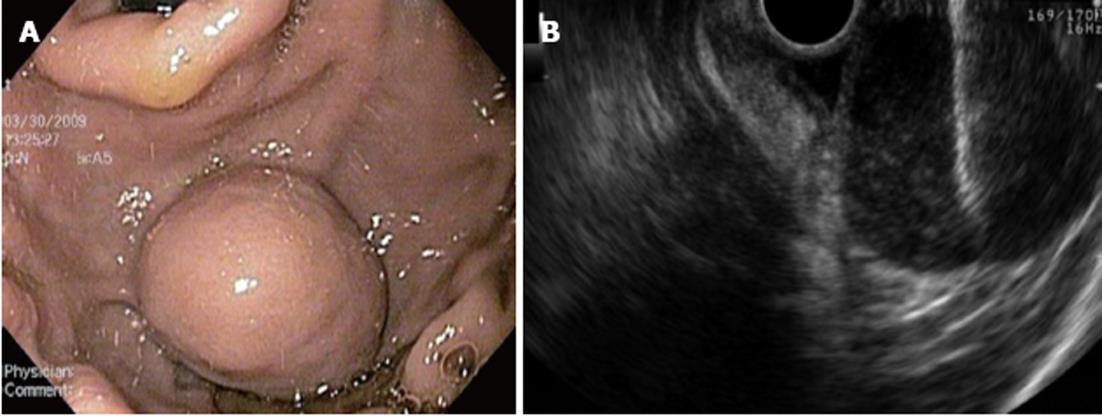
Figure 2 Endoscopy ultrasound images with fine needle aspiration biopsy.
A: A 3 cm × 3 cm submucosal intraluminal mass within the gastric cardia; B: This Endoscopy ultrasound image shows the fine needle aspiration biopsy needle (horizontal white line in upper right corner of image) puncturing the submucosal gastric gastrointestinal stromal tumors.
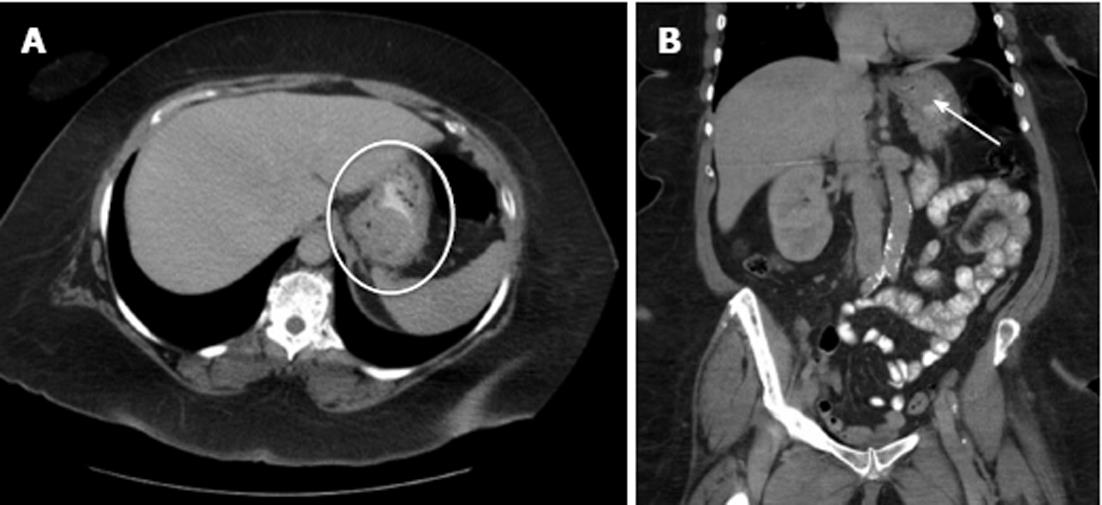
Figure 3 Gastroesophageal junction gastrointestinal stromal tumors.
A: An axial computed tomography image of a gastric gastrointestinal stromal tumor (white oval) located along the posterior wall of the gastroesophageal junction (GEJ); B: Coronal images of the tumor (white arrow) show its proximity to the GEJ.
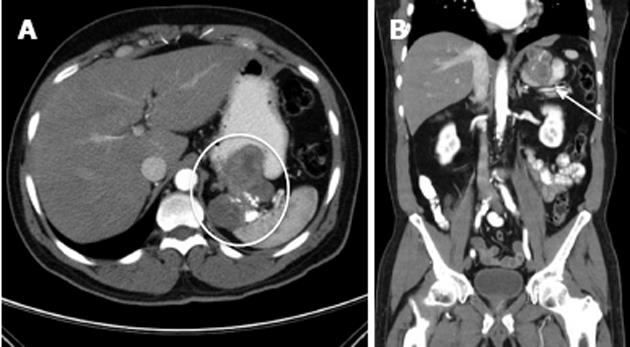
Figure 4 Locally-advanced gastric gastrointestinal stromal tumors.
A: Representative contrast-enhanced computed tomography images show a large, proximal gastric gastrointestinal stromal tumors that invades into the splenic hilum (oval); B: On the coronal images the arrow indicates a heterogeneous mass invading into the spleen with areas of viable tumor and necrotic areas represented by calcifications.
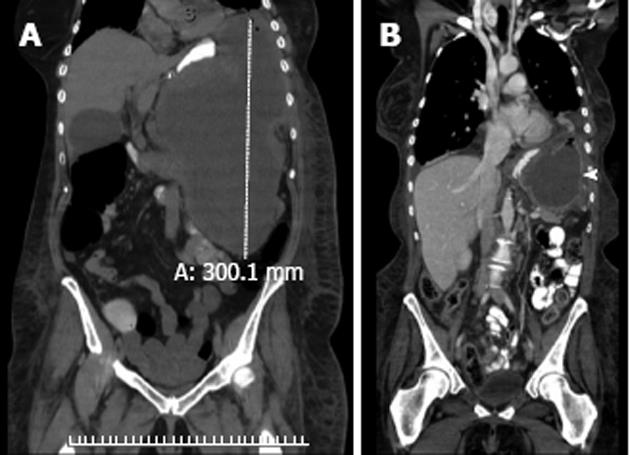
Figure 5 Neoadjuvant treatment of a locally-advanced gastrointestinal stromal tumors with imatinib mesylate.
A: This woman presented with abdominal pain and fullness. A computed tomography (CT) scan identified a massive (> 30 cm), homogeneous tumor in the gastric fundus that was exophytic and extending caudally towards the pelvic inlet; B: After tissue diagnosis confirmed a gastric gastrointestinal stromal tumor (GIST), the patient was treated with six months of low-dose imatinib mesylate (400 mg/d) until a maximal response was achieved. The coronal views of this interval CT scan demonstrated a much smaller, well-encapsulated, homogenous tumor (solid white arrowhead). She had a radical resection of the gastric GIST and was free of disease until 24 mo when she developed a metastatic lesion in the left lateral segment of the liver. Following complete metastectomy, she was treated with several targeted tyrosine kinase inhibitors until she ultimately succumbed from her metastatic disease 19 mo from her second operation and 43 mo from her initial operation.
- Citation: Roggin KK, Posner MC. Modern treatment of gastric gastrointestinal stromal tumors. World J Gastroenterol 2012; 18(46): 6720-6728
- URL: https://www.wjgnet.com/1007-9327/full/v18/i46/6720.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i46.6720