Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Feb 14, 2009; 15(6): 675-683
Published online Feb 14, 2009. doi: 10.3748/wjg.15.675
Published online Feb 14, 2009. doi: 10.3748/wjg.15.675
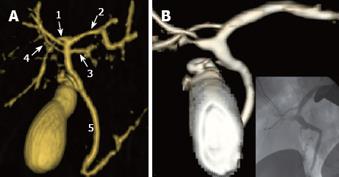
Figure 1 MDCT.
VR reconstruction images. A: 35-year-old male, potential living liver donor. Normal anatomy of hepatic artery. CHA: Common hepatic artery; GDA: Gastroduodenal artery; PHA: Proper hepatic artery; LHA: Left hepatic artery; RHA: Right hepatic artery; S4: Artery to segment 4; B: 29-year-old female, potential living liver donor. Early bifurcation of hepatic artery. Two large arterial branches to segment 4 arising from LHA and RHA; C: 25-year-old male, potential living liver donor. LHA arising from left gastric artery. The artery to segment 4 arising from the gastroduodenal artery.
Figure 2 Thirty-two-year-old male, potential living liver donor.
VR reconstruction shows a right anterior branch arising from left portal branch. SMV: Superior mesenteric vein; SplV: Splenic vein; LPV: Left portal vein; RAPD: Right anterior portal vein; RPPV: Right posterior portal vein.
Figure 3 Forty-one-year-old male, potential living liver donor.
VR reconstruction shows normal anatomy of hepatic veins. The right lobe and right hepatic vein are blue, the left lobe and the MHV and left hepatic veins are red. A cut-plane runs 1 cm to the right of the MHV.
Figure 4 Normal anatomy of biliary drainage: Right posterior duct (RPD) and right anterior duct (RAD) drain, respectively, S6-S7 and S8-S5; right hepatic duct (RHD) is formed by confluence of RPD and RAD.
Left hepatic duct (LHD) drains S2-S3. S1-S4 can be drained by LHD or by RHD. The common hepatic duct (CHD) arises from the confluence of RHD and LHD.
Figure 5 MRCP.
VR reconstruction images. A: Twenty-two-year-old male, potential living liver donor. VR image using MRCP acquisition shows congenital anomalies of biliary drainage: RPD (1) draining in LHD (2), accessory LHD (3) and accessory RPD (4) draining in MHD (5); B: 24-year-old female, potential living liver donor. VR image after Teslascan injection shows congenital anomalies of biliary drainage: RPD draining in LHD. The finding is confirmed with intraoperative cholangiogram.
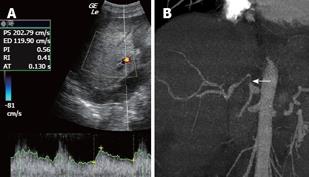
Figure 6 Fifteen-year-old male underwent orthotopic LT (OLT) for biliary atresia.
A: Ten days after OLT, CDUS shows a pathologic resistance index (< 0.5) and pathologic acceleration time (> 0.08), strongly suspicious for stenosis; B: AngioMDCT confirms a stenosis of the hepatic artery after the anastomosis (arrow).
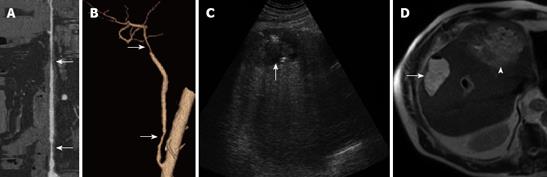
Figure 7 Fifty-four-year-old male underwent living related liver transplant (LRLT) for HCC in HCV-related cirrhosis.
A and B: 3 mo after LRLT, a lumen stripe reconstruction (A) and VR reconstruction (B) show irregularities (arrow) of aortohepatic by-pass. Six months after LRLT, the patient was admitted to hospital with fever; C: US shows a hypoechoic and inhomogeneous lesion in the right lobe (arrow); D: MR T2W images show a hyperintense lesion, confirming an abscess in the right lobe (arrow). The left lobe appears inhomogeneously and diffusely hyperintense, showing a large abscess (head of arrow).
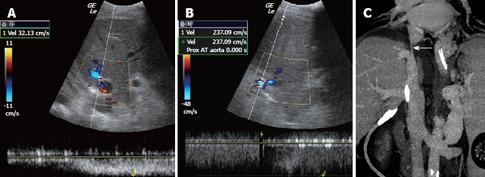
Figure 8 Fifty-one-year-old male underwent OLT for HCC in HCV-related cirrhosis.
A and B: Eight days after OLT, CDUS shows a high velocity gradient between the subhepatic (A) and suprahepatic (B) segments of the inferior vena cava, with a velocity of 32 cm/s and 237 cm/s, respectively, strongly suspicious for stenosis; C: MDCT with MPR image confirms stenosis of the suprahepatic segment of the inferior vena cava (arrow).
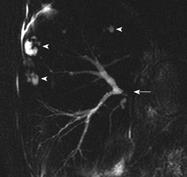
Figure 9 Sixty-one-year-old male underwent OLT for primary biliary cirrhosis, with bilio-enteric anastomosis.
MRCP shows a severe anastomotic stricture (arrow) and multiple intrahepatic biliary leakages (head of arrows).
- Citation: Caruso S, Miraglia R, Maruzzelli L, Gruttadauria S, Luca A, Gridelli B. Imaging in liver transplantation. World J Gastroenterol 2009; 15(6): 675-683
- URL: https://www.wjgnet.com/1007-9327/full/v15/i6/675.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.675