Copyright
©2009 The WJG Press and Baishideng.
World J Gastroenterol. Jun 28, 2009; 15(24): 3038-3045
Published online Jun 28, 2009. doi: 10.3748/wjg.15.3038
Published online Jun 28, 2009. doi: 10.3748/wjg.15.3038
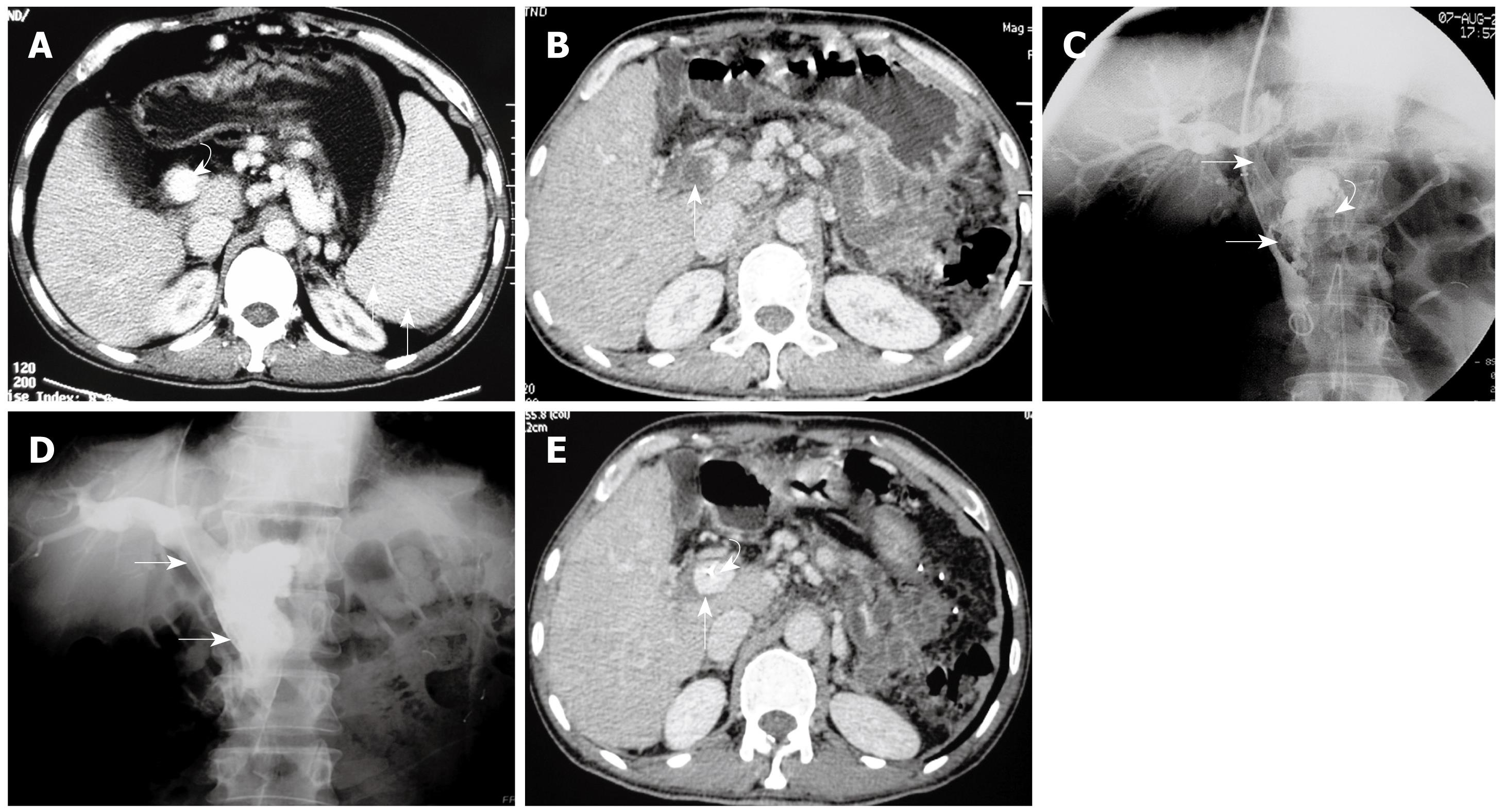
Figure 1 Case 1: A 40-year-old man with low-grade fever, abdominal pain, distension, and nausea for 12 d.
He had undergone splenectomy 4 wk previously. A: Selected axial image from before open splenectomy contrast-enhanced CT shows splenomegaly (arrows) and patent portal vein (curved arrow); B: Selected axial image from admission contrast-enhanced CT, on postoperative day 28, shows massive thrombus within the PV (arrow); C: Pre-treatment direct venography via transjugular approach access to the portal vein shows massive thrombosis of the PV extending into the SMV (arrows). Note the stump of the splenic vein (curved arrow); D: Follow-up direct portal venography via the infusion catheter, obtained 5 d after the catheter infusion of thrombolytics, shows patency of the main PV-SMV (arrows); E: CT image at the same level as in Figure 1B obtained 5 d after the interventional procedure, before the infusion catheter removal, shows the wide patent main PV (arrow). Note the infusion catheter within the PV (curved arrow).
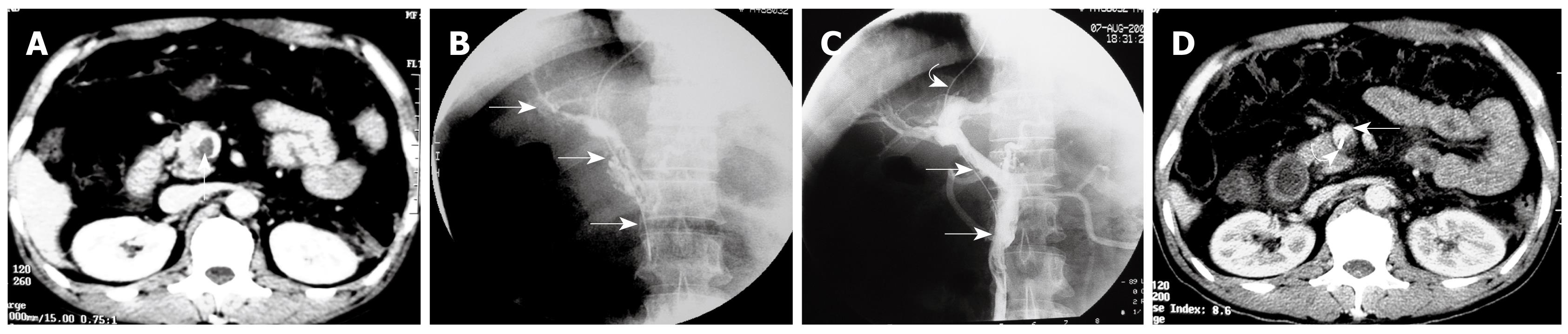
Figure 2 Case 2: A 43-year-old man with epigastric pain, diarrhea, fever, and vomiting for 1 wk.
He had undergone splenectomy 3 wk previously. A: Selected axial image from admission contrast-enhanced CT, on postoperative day 21, shows thrombus (arrow) within the SMV; B: Pre-treatment direct venography via transjugular approach access to the portal vein shows extensive thrombosis of the SMV extending into the main PV and intrahepatic branches (arrows); C: Follow-up direct portal venography via the infusion catheter (curved arrow), obtained 6 d after the catheter infusion of thrombolytics, shows patent PV and SMV with only minimal residual wall thrombus (arrows); D: CT image at the same level as in Figure 2A obtained 6 d after the catheter infusion of thrombolytics, before the infusion catheter removal, shows the wide patent SMV (arrow) with only minimal residual wall thrombus. Note the infusion catheter within the SMV (curved arrow).
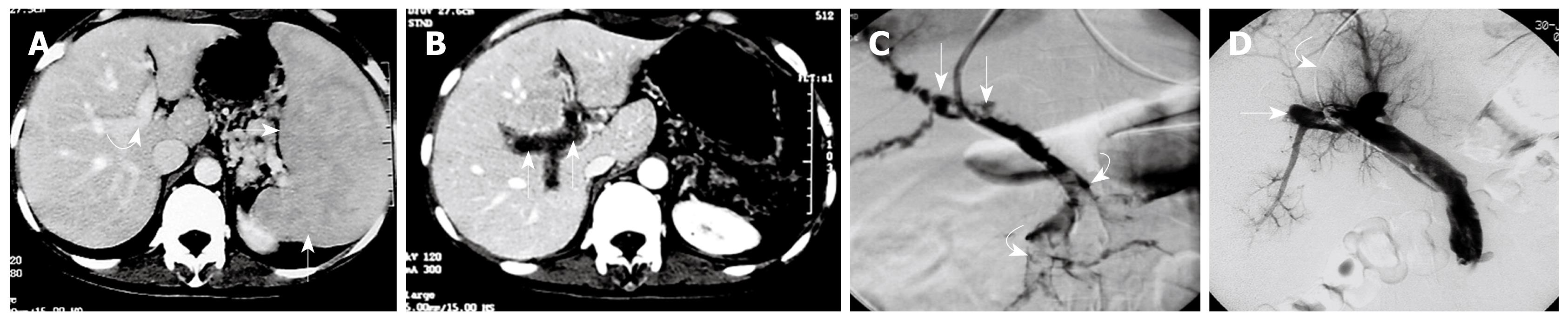
Figure 3 Case 3: A 38-year-old woman with abdominal pain, nausea, distension, and vomiting for 3 d.
She had undergone splenectomy 2 wk previously. A: Selected axial image from before open splenectomy contrast-enhanced CT shows splenomegaly (arrows) and patent portal vein (curved arrow); B: Selected axial image from admission contrast-enhanced CT, on postoperative day 14, shows extensive thrombus within the PV (arrows); C: Pre-treatment direct venography via transjugular approach access to the portal vein showing extensive PV (arrows) and SMV (curved arrows) thrombosis, without collateral drainage; D: Follow-up direct portal venography via the infusion catheter (curved arrow), obtained 5 d after the catheter infusion of thrombolytics, shows patent PV and SMV with residual thrombosis within the intrahepatic portal venous branches (arrow).
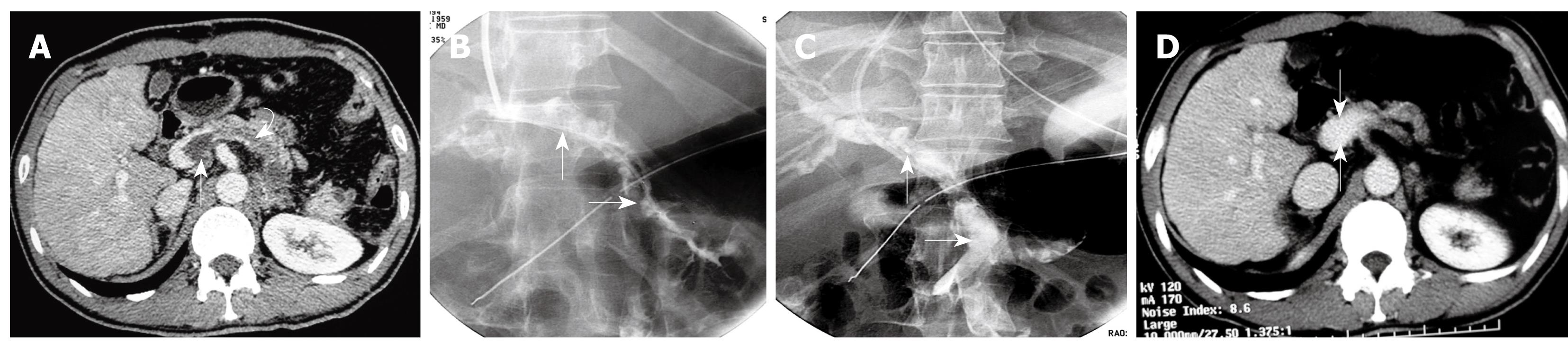
Figure 4 Case 4: A 42-year-old man with abdominal pain, diarrhea, and nausea for 2 wk.
He had undergone splenectomy 4 wk previously. A: Selected axial image from admission contrast-enhanced CT demonstrates massive thrombus within the proximal of SMV (arrow) and the stump of the splenic vein (curved arrow); B: Pre-treatment direct venography via transjugular approach access to the portal vein showing extensive PV-SMV thrombosis (arrows), without collateral drainage; C: Immediate follow-up direct portal venography after catheter fragmentation and aspiration of the PV-SMV thrombosis, shows 75% reduction of thrombosis in the SMV and PV (arrow). The catheter infusion of thrombolytics was continued for 4 d and further improvement was confirmed by CT follow-up; D: Contrast-enhanced CT image at the same level as in Figure 4A obtained 5 d after completion of the interventional procedure shows a wide patent SMV (arrows).
- Citation: Wang MQ, Lin HY, Guo LP, Liu FY, Duan F, Wang ZJ. Acute extensive portal and mesenteric venous thrombosis after splenectomy: Treated by interventional thrombolysis with transjugular approach. World J Gastroenterol 2009; 15(24): 3038-3045
- URL: https://www.wjgnet.com/1007-9327/full/v15/i24/3038.htm
- DOI: https://dx.doi.org/10.3748/wjg.15.3038