Copyright
©2008 The WJG Press and Baishideng.
World J Gastroenterol. Oct 21, 2008; 14(39): 6012-6017
Published online Oct 21, 2008. doi: 10.3748/wjg.14.6012
Published online Oct 21, 2008. doi: 10.3748/wjg.14.6012
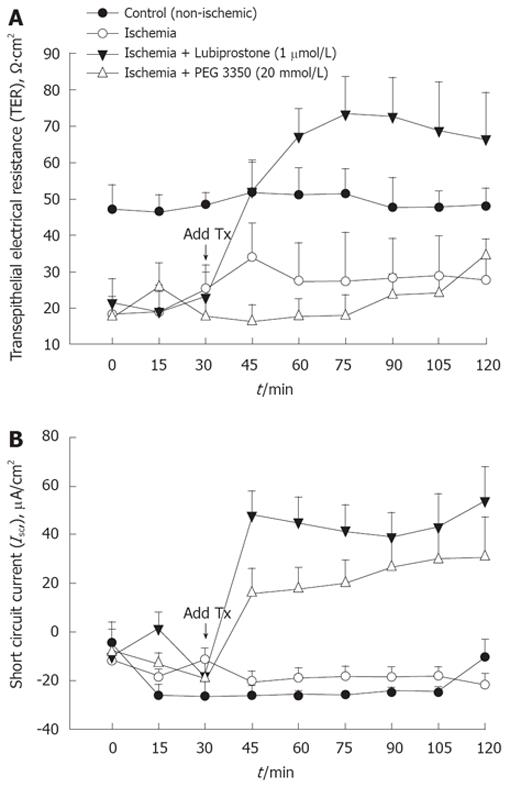
Figure 1 TER (A) and short circuit current (Isc) (B) in ischemic porcine ileum treated with lubiprostone and PEG 3350.
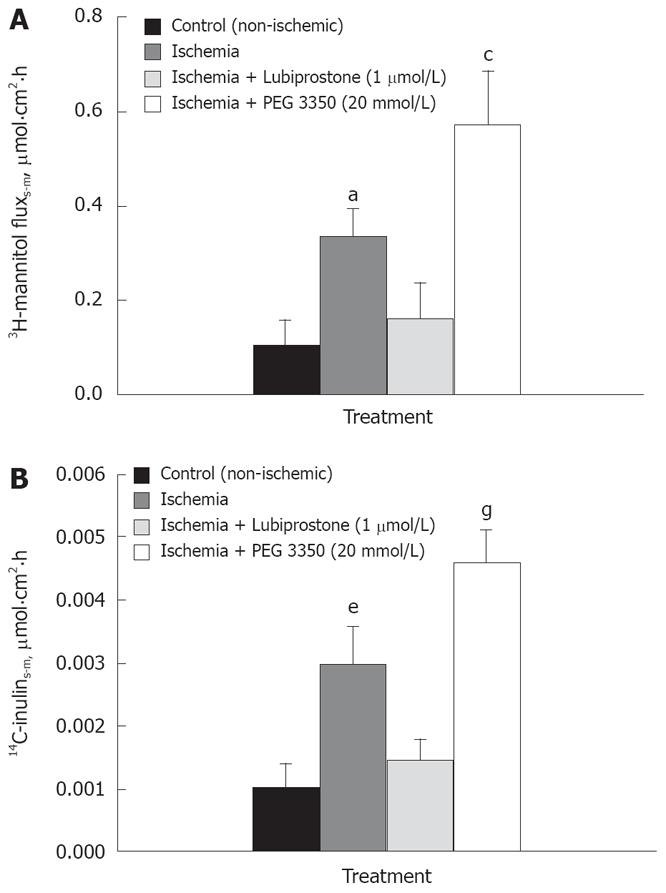
Figure 2 A: Mucosal-to-serosal flux of 3H-mannitol in porcine ileum.
aP < 0.05 ischemia vs control, ischemia/lubiprostone; cP < 0.05 ischemia + PEG3350 vs control, ischemia, ischemia + lubiprostone; B: Mucosal-to-serosal flux of 14C-inulin in porcine ileum. eP < 0.05 ischemia vs control, ischemia/lubiprostone; gP < 0.05 ischemia + PEG3350 vs control, ischemia, ischemia/lubiprostone.
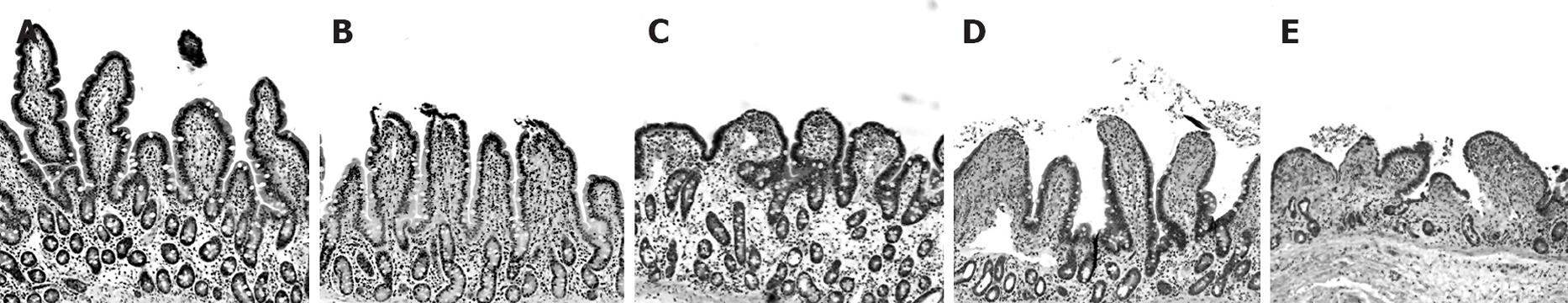
Figure 3 Light microscopic evaluation of ischemic intestinal tissues.
A: Control (non-ischemic); B: Time 0 post-ischemia; C: Time 120-min post ischemia; D: Lubiprostone-time 120 min post-ischemia; E: -PEG 3350-time 120-min post-ischemia.
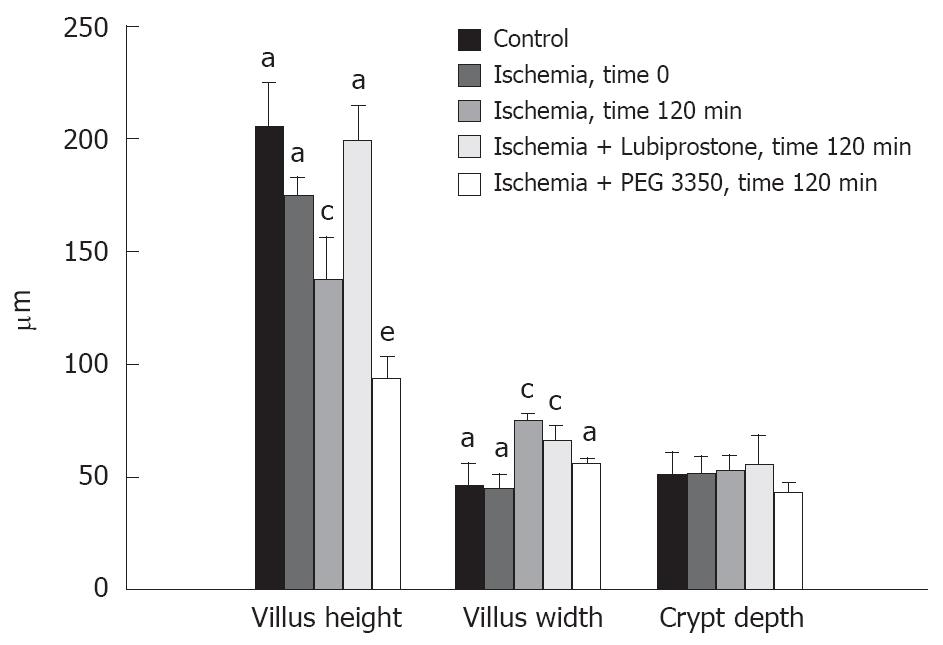
Figure 4 Morphometric evaluations of ischemic intestinal tissues.
Villus height: aP < 0.05 control, ischemia time 0 min, lubiprostone vs ischemia time 120 min, PEG 3350; cP < 0.05 ischemia time 120 min vs all other groups; eP < 0.05 PEG 3350 vs all other groups; Villus width: aP < 0.05 control, ischemia time 0 min vs ischemia time 120 min, lubiprostone; cP < 0.05 ischemia time 120 min, lubiprostone vs all other groups.
- Citation: Moeser AJ, Nighot PK, Roerig B, Ueno R, Blikslager AT. Comparison of the chloride channel activator lubiprostone and the oral laxative Polyethylene Glycol 3350 on mucosal barrier repair in ischemic-injured porcine intestine. World J Gastroenterol 2008; 14(39): 6012-6017
- URL: https://www.wjgnet.com/1007-9327/full/v14/i39/6012.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6012