Copyright
©2008 The WJG Press and Baishideng.
World J Gastroenterol. Sep 14, 2008; 14(34): 5290-5300
Published online Sep 14, 2008. doi: 10.3748/wjg.14.5290
Published online Sep 14, 2008. doi: 10.3748/wjg.14.5290
Figure 1 Endoscopic view of the rectal stump from one UC patient (TR) showing a hard and ulcerated mass inducing stenosis of the anastomosis, not passed by the colonoscope.
Histological analysis of the lesion detected an adenocarcinoma of the rectal stump.
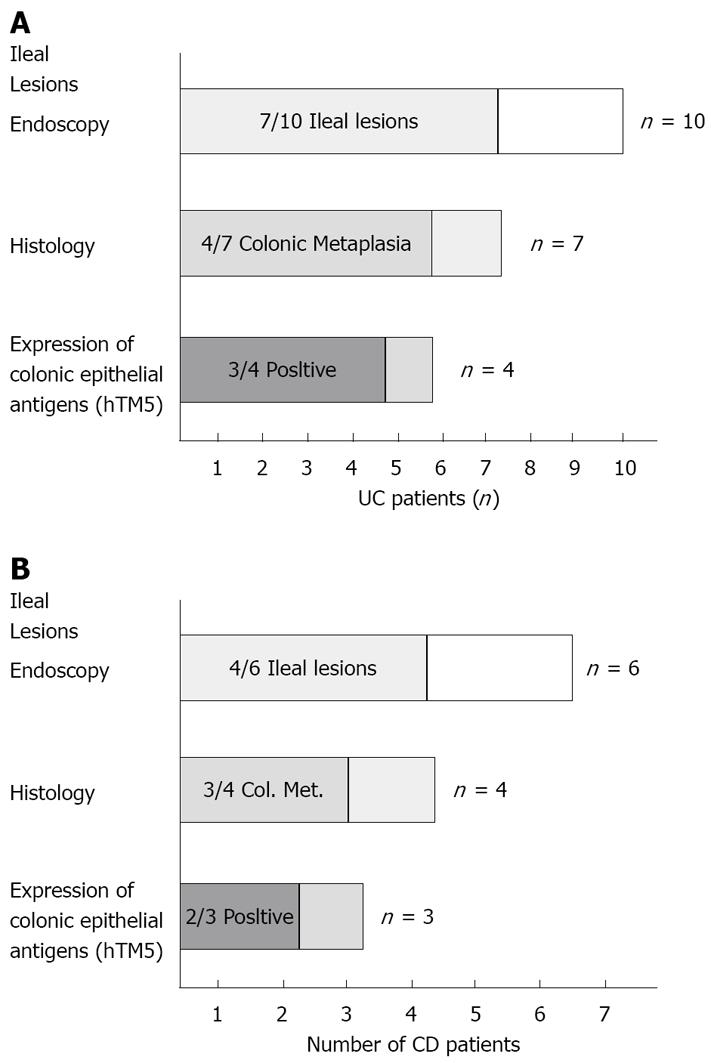
Figure 2 Histograms indications.
A: The number of UC patients after IRA showing: Lesions in the neo-terminal ileum as assessed by endoscopy; Histological findings compatible with colonic metaplasia; Expression of hTM5-related colon epithelial antigens; B: The number of CD patients with IRA showing ileal recurrence at endoscopy, inflammatory changes at histology (including those compatible with colonic metaplasia) and expression of hTM5-related colonic epithelial antigens.
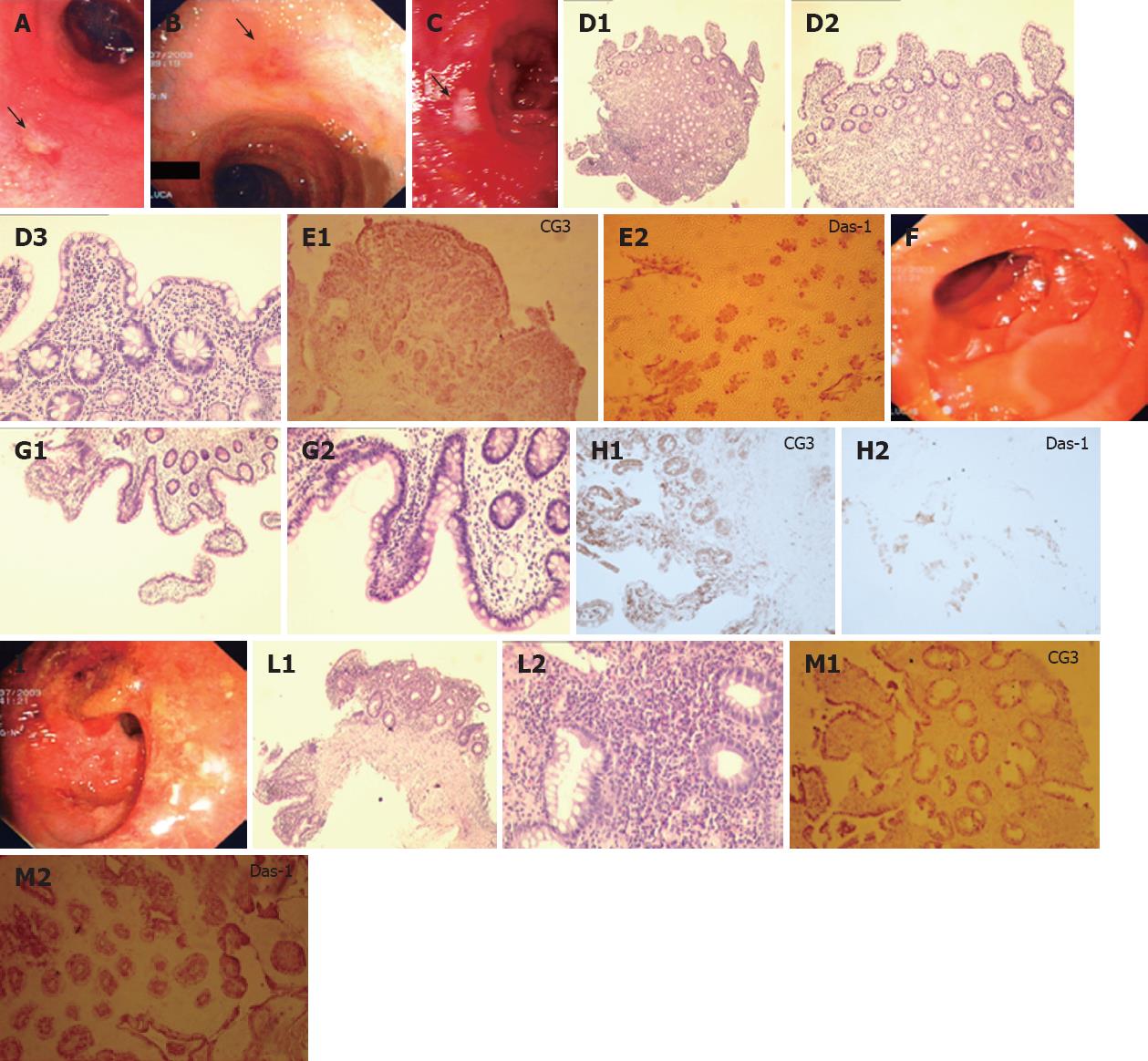
Figure 3 Endoscopic view, histological analysis and immunohistochemistry against CG3 and Das-1 MoAbs of biopsy samples taken from the neo-terminal ileum and rectal stump from a second UC patient (DLE) with IRA.
A-C: Endoscopic views of the neo-terminal ileum at 3 endoscopies, showing focal erosions and ulcers at all times; D: Histological analysis of ileal biopsy samples, compatible with changes towards colonic epithelium, including villous atrophy; E: Immunostochemistry showing staining against CG3 (E1) and Das-1 (E2) MoAbs in the same ileal samples. F-H: Endoscopic view (F), histological (G1, G2) and immunohistochemical analysis against CG3(H1) and Das-1 MoAbs (H2) of the uninvolved ileum, showing no inflammation or colonic metaplasia. I-M: Endoscopic view (I), histological (L1, L2) and immunohistochemical analysis using CG3(M1) and Das-1 MoAbs (M2) of the rectal stump, showing typical UC lesions and staining against hTM5-related antigens.
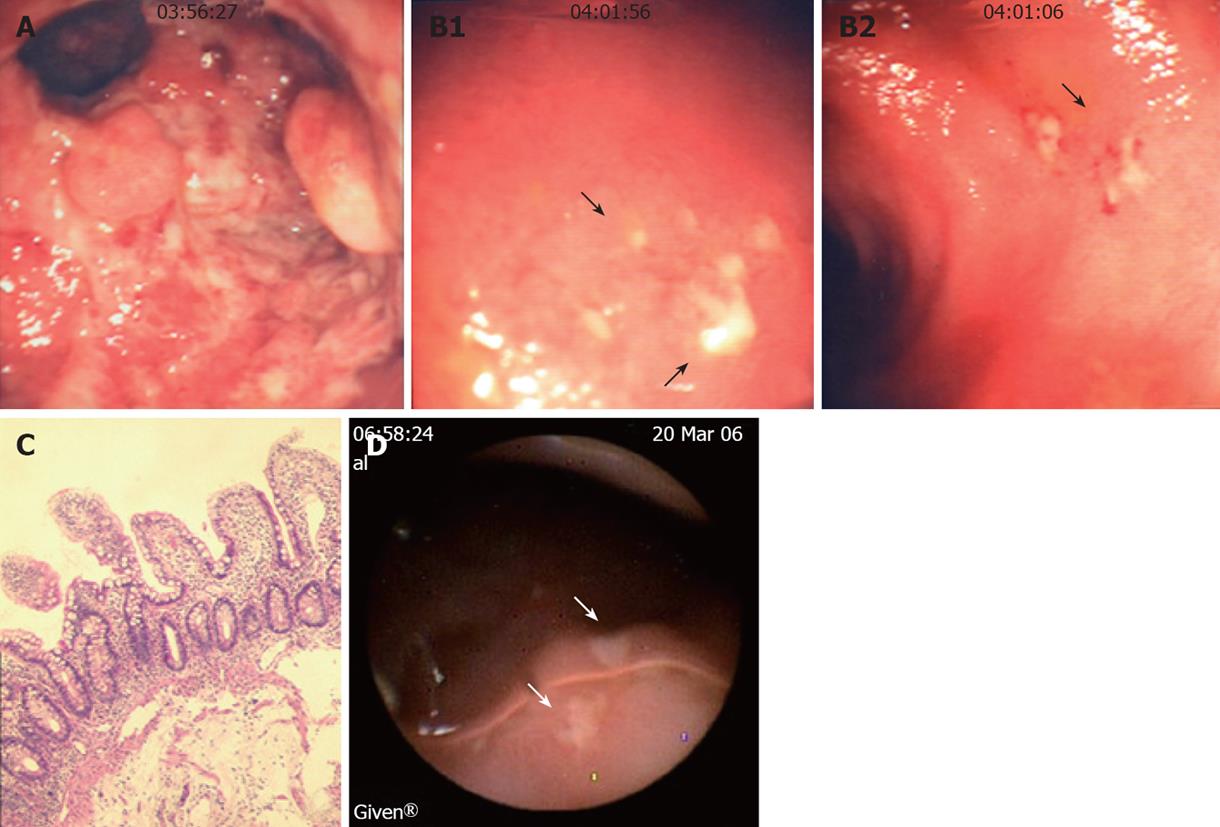
Figure 4 Endoscopic view, histological analysis and WCE images of the rectum and neo-terminal ileum from a third UC patient (LRA) with IRA.
A: Endoscopic view of the rectal stump showing erosions and pseudopolyps; B: Endoscopic views of the ileum showing small focal ulcers above the anastomosis; C: Ileal biopsy sample from the same patient showing no villous atrophy or colonic metaplasia by histology; D: WCE images showing in the neo-terminal ileum above the anastomosis, 2 ulcers covered by fibrin (arrows) surrounded by macroscopically normal ileum.
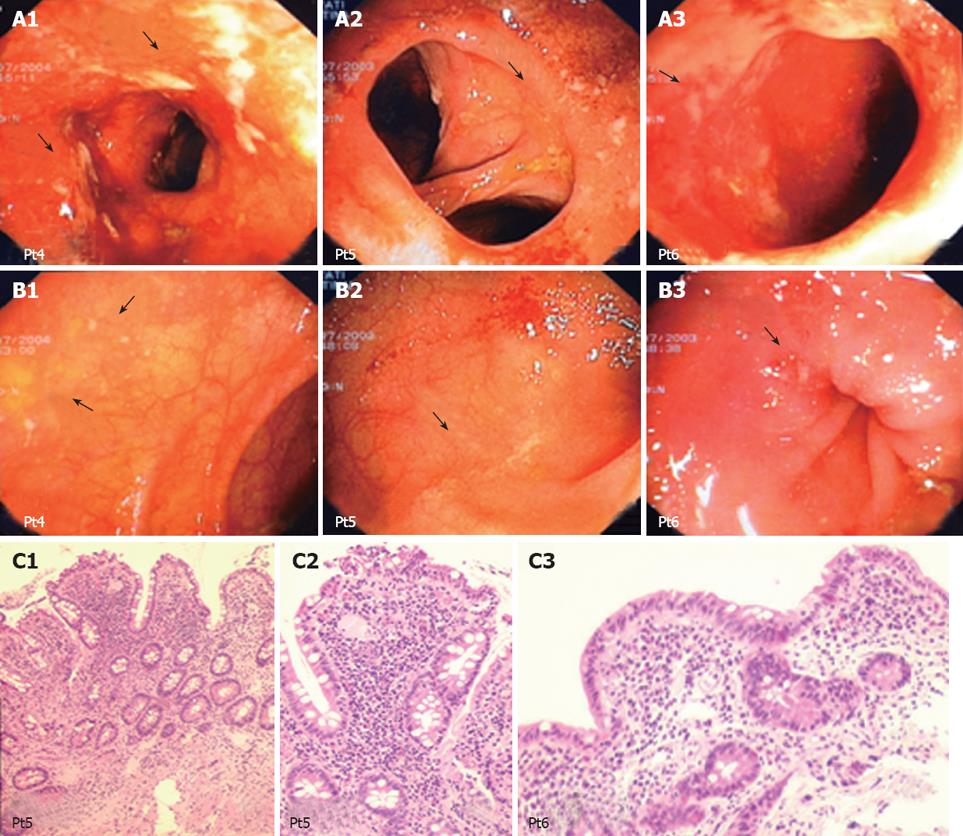
Figure 5 Endoscopic view and histological analysis of the anastomosis and neo-terminal ileum from 3 UC patients with IRA.
A: Endoscopic views of the anastomosis from 3 UC patients showing focal small ulcers; B: Endoscopic views of the neo-terminal ileum from the same 3 UC patients, scattered ulcerations surrounded by macroscopically uninvolved ileum; C: Histological analysis of biopsy samples taken from the involved neo-terminal ileum from patients 5 and 6, showing changes towards colonic metaplasia.
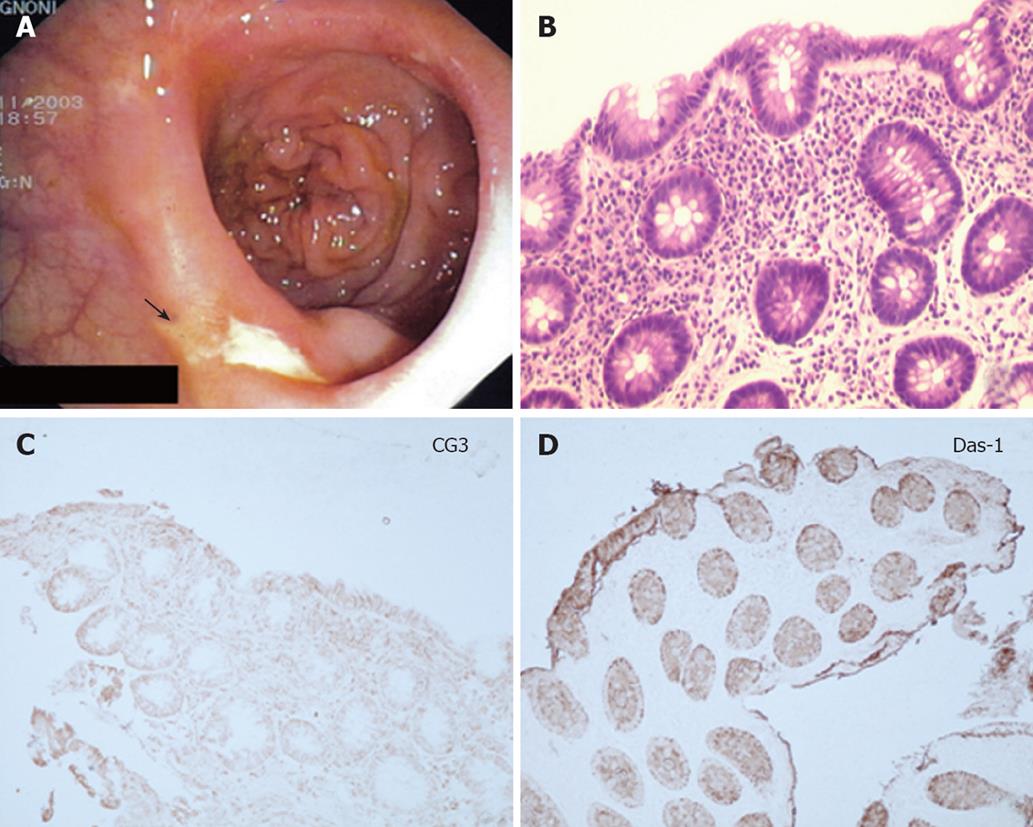
Figure 6 Endoscopic view (A), histological (B) and immunohis-tochemical analysis using CG3 (C) and Das-1 MoAbs (D) of the neo-terminal ileum form one CD patient.
Endoscopy shows CD recurrence (grade 2), histology lesions compatible with changes of the ileum towards colonic epithelium and immunohistochemistry staining against CG3 and Das-1 MoAbs.
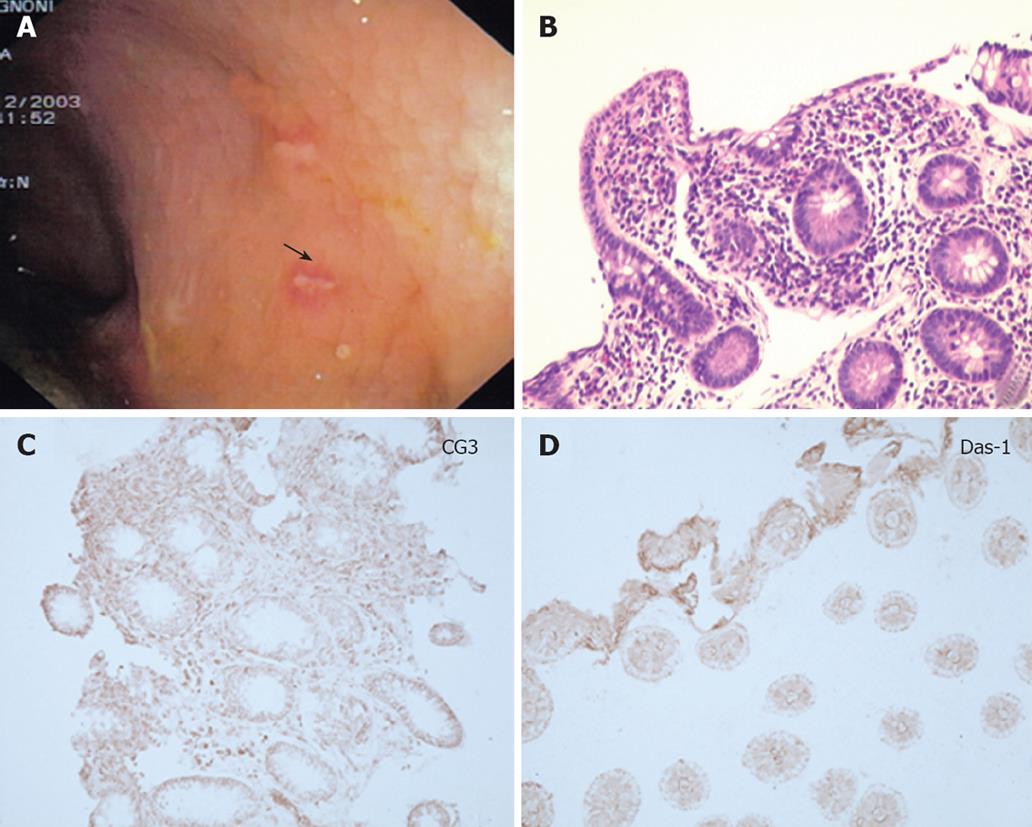
Figure 7 Endoscopic view (A), routine histochemical (B) and immunohistochemistry analysis using CG3 (C) and Das-1 MoAbs (D) of the neo-terminal ileum from a second CD patient.
Endoscopy detected recurrence of the anastomosis and neo-terminal ileum (grade 3), histology lesions compatible with changes of the ileal epithelium towards colonic epithelium and immunohistochemistry the expression of colonic epithelial antigens, compatible with colonic metaplasia.
- Citation: Biancone L, Calabrese E, Palmieri G, Petruzziello C, Onali S, Sica GS, Cossignani M, Condino G, Das KM, Pallone F. Ileal lesions in patients with ulcerative colitis after ileo-rectal anastomosis: Relationship with colonic metaplasia. World J Gastroenterol 2008; 14(34): 5290-5300
- URL: https://www.wjgnet.com/1007-9327/full/v14/i34/5290.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.5290