Copyright
©2006 Baishideng Publishing Group Co.
World J Gastroenterol. Apr 21, 2006; 12(15): 2320-2327
Published online Apr 21, 2006. doi: 10.3748/wjg.v12.i15.2320
Published online Apr 21, 2006. doi: 10.3748/wjg.v12.i15.2320
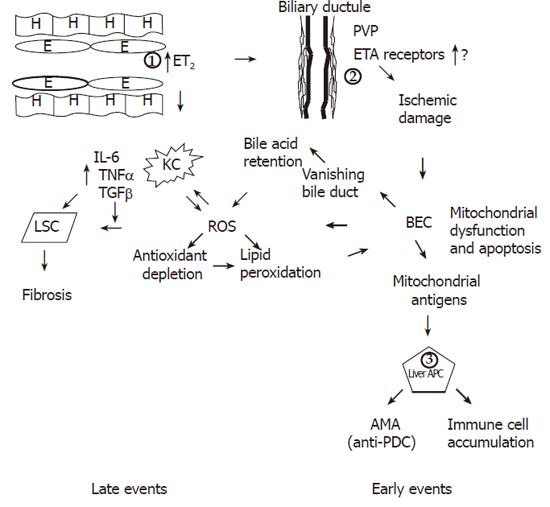
Figure 1 Figure 1 Occurrence of late and early events in the unifying model.
The fundamental early defect in PBC is the overproduction of ET2 by endothelial cells (1) possibly driven by virus [95-98] or other microbial pathogens in genetically predisposed individuals. ET2 is a chemoattractant for Kupffer cells and also causes contraction of stellate cells leading to early portal hypertension. ET2 leads to ischemic damage of BEC (2) through constriction of the PVP with resultant BEC mitochondrial dysfunction and membrane disruption by ROS generation and eventually apoptosis leading to the vanishing bile duct syndrome. Mitochondrial antigens possibly generated through caspase cleavage, are presented by hyper-responsive liver dendritic cells (APC) (3) and lead to immune cell accumulation and AMA production. The second fundamental defect occurring later in the disease process is the production of ROS. Together with ingestion of BEC apoptotic bodies, ROS drives the accumulated Kupffer cells to produce more ROS and pro-inflammatory cytokines and TGFβ, which in turn leads to fibrosis. ROS is also produced after development of the vanishing bile duct syndrome as a result of bile acid retention. Finally through antioxidant depletion or through an insufficient increase of antioxidants ROS leads to lipid peroxidation and further BEC apoptosis and mitochondrial dysfunction. Genetically determined control may be exercised at levels 1,2 and 3.
- Citation: Kouroumalis E, Notas G. Pathogenesis of primary biliary cirrhosis: A unifying model. World J Gastroenterol 2006; 12(15): 2320-2327
- URL: https://www.wjgnet.com/1007-9327/full/v12/i15/2320.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i15.2320