Copyright
©2005 Baishideng Publishing Group Inc.
World J Gastroenterol. Mar 21, 2005; 11(11): 1610-1615
Published online Mar 21, 2005. doi: 10.3748/wjg.v11.i11.1610
Published online Mar 21, 2005. doi: 10.3748/wjg.v11.i11.1610
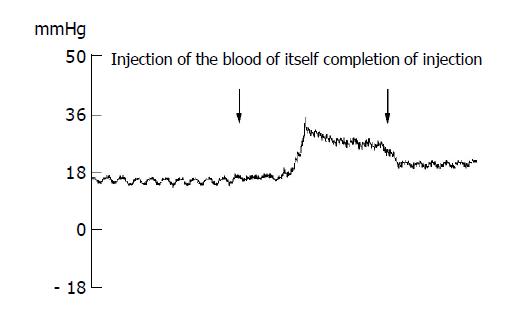
Figure 1 Changes in the pressure of the lateral ventricle during acute brainstem hemorrhage in rabbit.
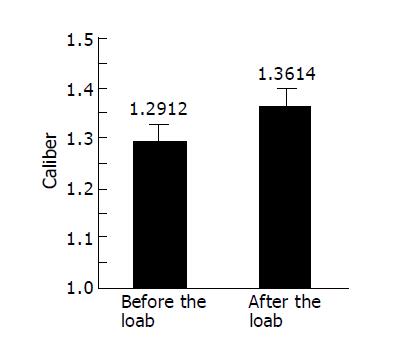
Figure 2 Changes in caliber of jejunal mesentery small vessels under the load of rabbit’s brainstem hemorrhage.
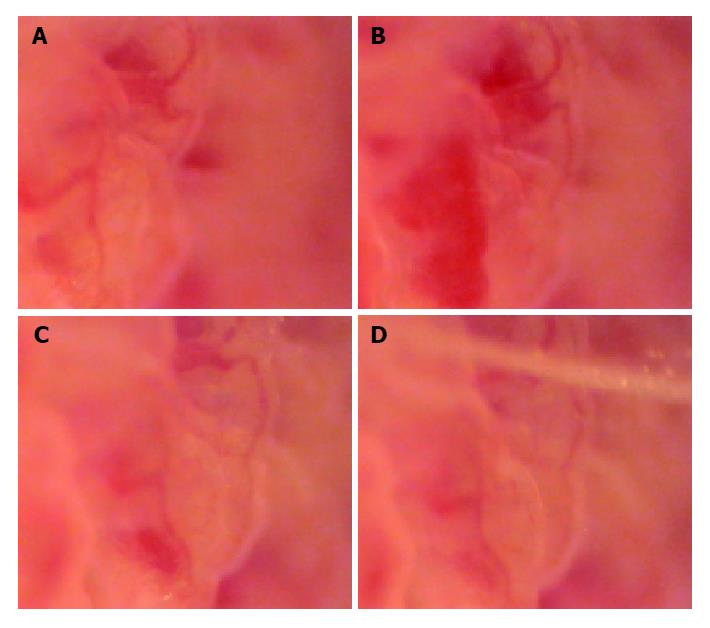
Figure 3 Changes of microcirculation of jejunal mucosa.
A: Photograph of microcirculation of jejunal mucous membrane, 6 s before the load of rabbit’s brainstem hemorrhage (×185); B: Photograph of jejunal mucous membrane, 10 min 26 s after the load of rabbit’s brainstem hemorrhage; it showed the local congestion of villus mucosa (×185); C: Photograph of jejunal mucous membrane, 30 min 32 s after the load of rabbit’s brainstem hemorrhage; it showed that the local congestion of villus mucosa had relieved (×185); D: Photograph of jejunal mucous membrane, 40 min 46 s after the load of rabbit’s brainstem hemorrhage; it showed that the local congestion of villus mucosa had ameliorated obviously (×185).
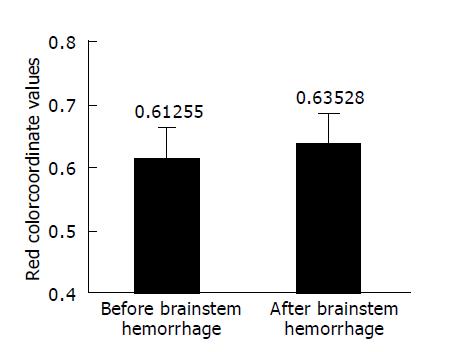
Figure 4 Paired t-test for red color coordinate mean values of jejunal mucous membrane before and after rabbit’s brainstem hemorrhage.
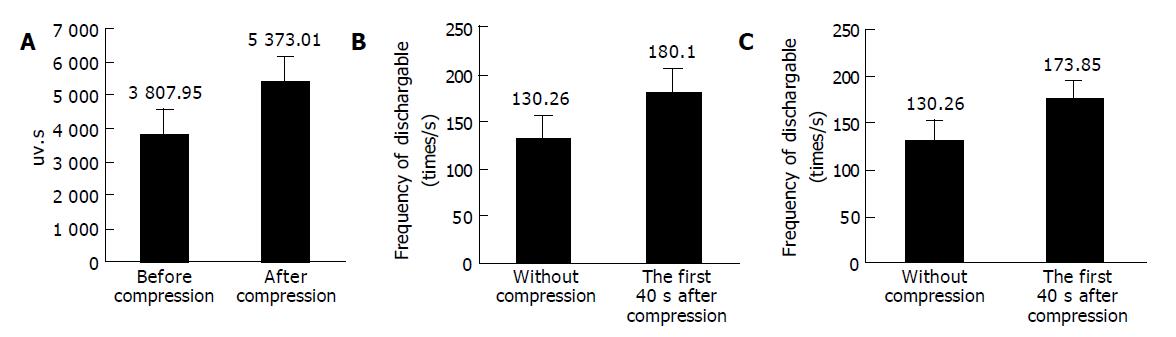
Figure 5 Comparison of electric discharge of vagus nerve.
A: The comparison of the electric discharge of vagus nerve through analyzing the absolute value of an area of wave form before and after the compression (from 4 to 40 s under the intracranial hypertension), and the neural discharge of vagus nerve had increased after intracranial hypertension, n = 20, P<0.05; B: The comparison of the electric discharge of vagus nerve before and during the first 4 s after the rabbit’s lateral ventricle compression. We analyzed the electric discharge frequency of the dischargeable wave in each time segment by setting a single liminal value line, and the neural discharge of vagus nerve had increased after intracranial hypertension; C: The comparison of the electric discharge of vagus nerve before the compression and during continuous compression (from 4 to 40 s). We analyzed the electric discharge frequency of the dischargeable wave in each time segment by setting a single liminal value line, and the neural discharge of vagus nerve had increased after intracranial hypertension.
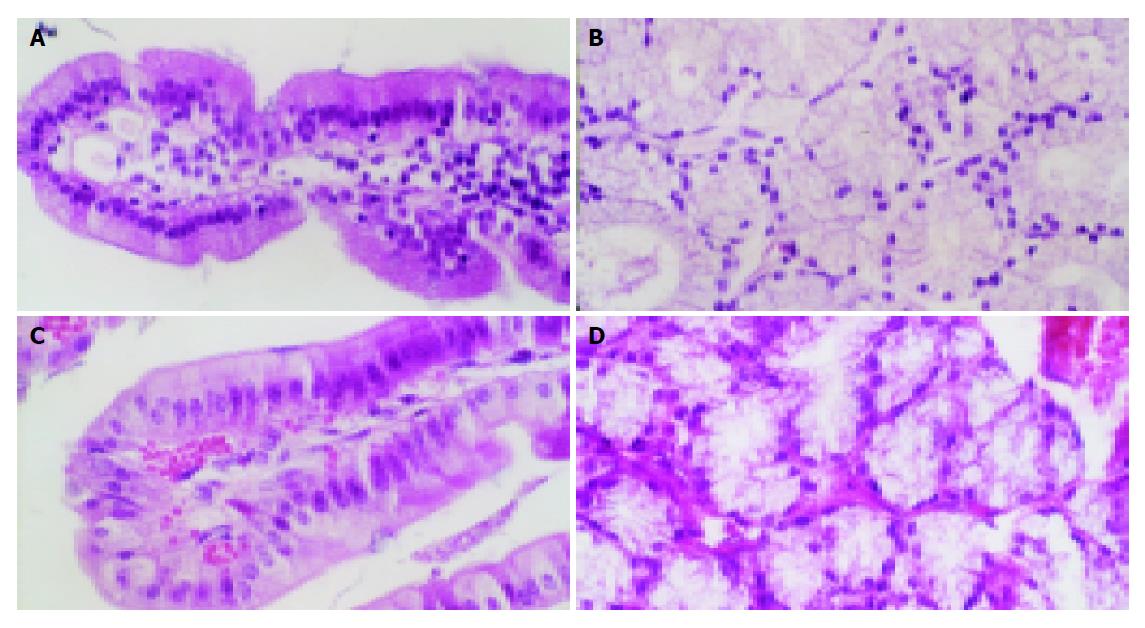
Figure 6 HE stain of duodenal structure of rabbits.
A: HE stain of normal rabbit’s duodenal villus. The minute blood vessel had not dilated and red blood cells had not leaked out from capillary lumens; B: HE stain of normal rabbit’s mucous glands of duodenum. The minute blood vessel had not dilated; C: HE stain of the rabbit’s duodenal villus, which were 48 h after brainstem hemorrhage. The capillaries had obviously dilated and red blood cells had leaked out from capillary lumens; D: HE stain of the rabbit’s mucous glands of duodenum, which were 48 h after brainstem hemorrhage. The capillaries had obviously dilated and red blood cells had leaked out from capillary lumens.
- Citation: Jin XL, Zheng Y, Shen HM, Jing WL, Zhang ZQ, Huang JZ, Tan QL. Analysis of the mechanisms of rabbit’s brainstem hemorrhage complicated with irritable changes in the alvine mucous membrane. World J Gastroenterol 2005; 11(11): 1610-1615
- URL: https://www.wjgnet.com/1007-9327/full/v11/i11/1610.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i11.1610