Copyright
©The Author(s) 2004.
World J Gastroenterol. Oct 1, 2004; 10(19): 2859-2863
Published online Oct 1, 2004. doi: 10.3748/wjg.v10.i19.2859
Published online Oct 1, 2004. doi: 10.3748/wjg.v10.i19.2859
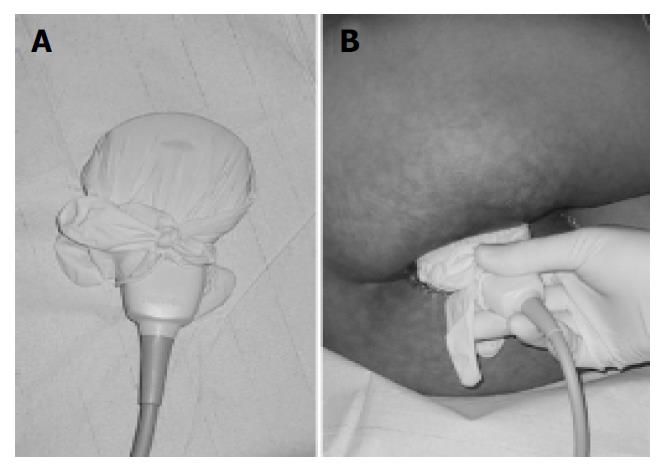
Figure 1 A regular latex examination glove filled with ultra-sound contact gel was used to cover the probes for hygienic reasons (A).
The examinations were performed in the left lat-eral position with the probe placed above the anus (B).
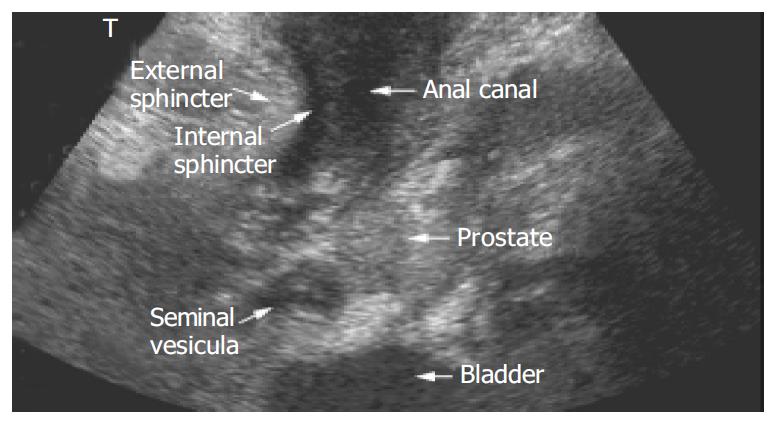
Figure 2 A general overview over perianal anatomy and pa-thology can be obtained using a regular convex 3.
5 Mhz probe.
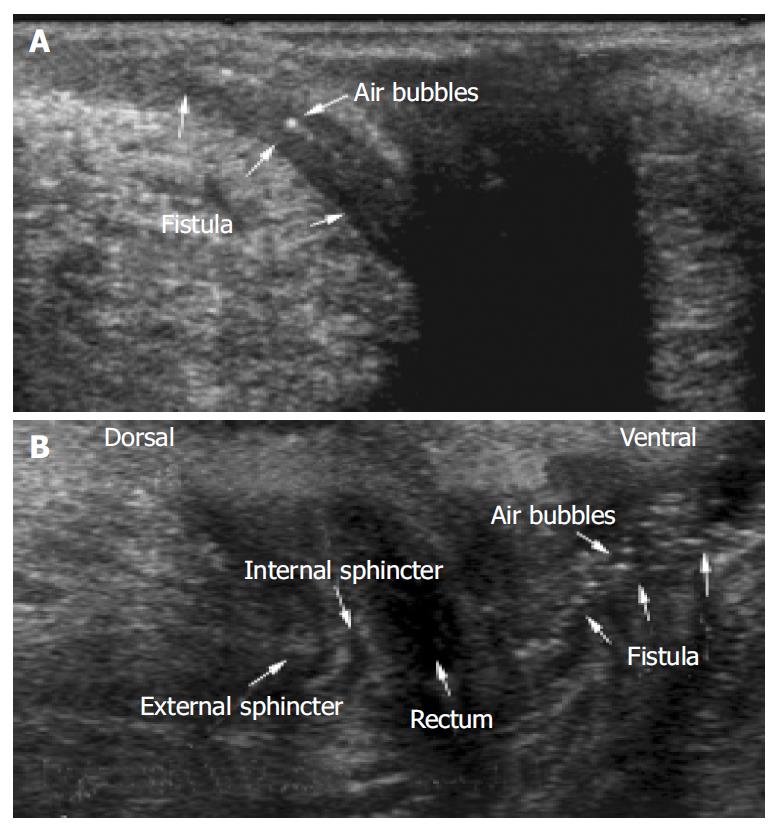
Figure 3 Perianal imaging of entero-cutaneous fistulae using a 10 MHz ultrasound probe.
Hyperechoic dots resemble air bubbles within the fistulous track. The rectum represents as hypo- anechoic structure. External and internal anal sphincter can be distinguished.
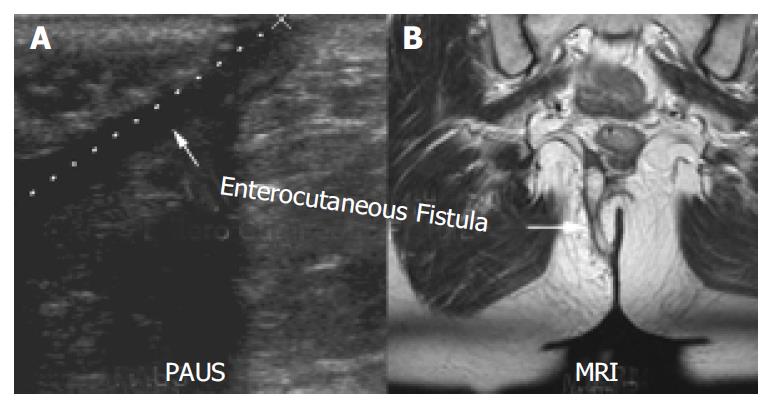
Figure 4 Enterocutaneous fistula detected with PAUS (A) was confirmed using MRI (oblique coronary T2-FSE sequence with-out fat saturation) (B).
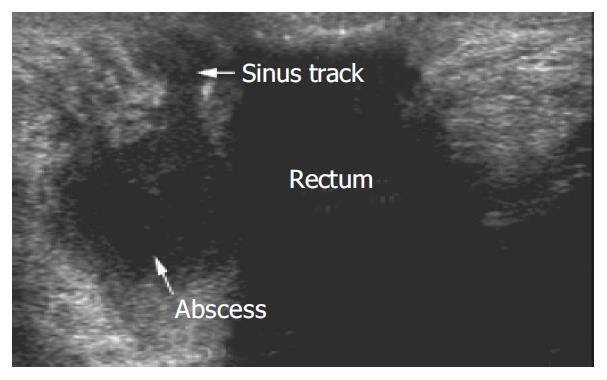
Figure 5 Typical appearance of a pararectal abscess, dorsal of the rectum.
Furthermore a sinus track could be detected that perforated the external sphincter and ceased in multiple small sinus tracks that did not have a cutaneous opening.
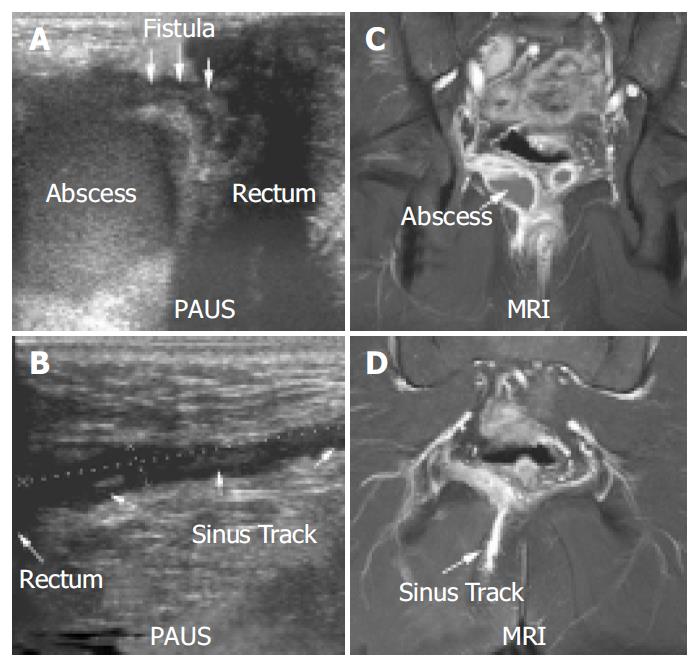
Figure 6 PAUS (A + B) and MRI (C + D) imaging (coronary fat-saturated T1-SE sequence after gadolinium administration) of a perianal abscess.
In contrast to MRI, PAUS was able to clearly identify a connection between the rectum and the abscess (A + C). Both methods could identify a sinus track that began within the abscess and ended in the gluteal fat (B + D). A scale (cm) is shown on the left side of the PAUS images for orientation.
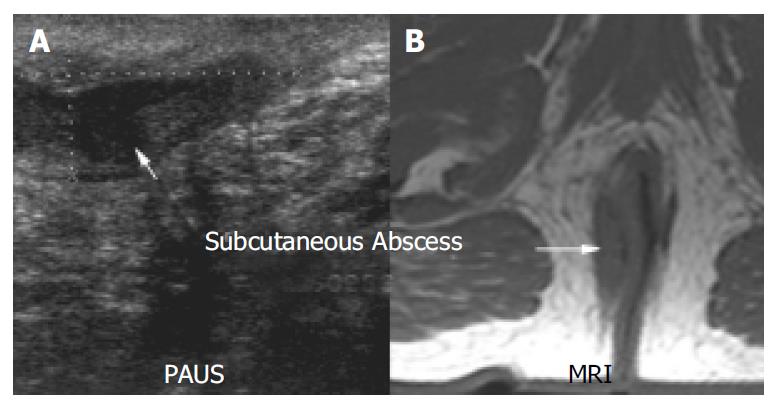
Figure 7 Comparison of PAUS (A) and MRI (B) imaging (transverse T1-SE sequence) of a subcutaneous abscess.
A small fistula from the rectum to the abscess could be detected with PAUS and MRI.
- Citation: Wedemeyer J, Kirchhoff T, Sellge G, Bachmann O, Lotz J, Galanski M, Manns MP, Gebel MJ, Bleck JS. Transcutaneous perianal sonography: A sensitive method for the detection of perianal inflammatory lesions in Crohn’s disease. World J Gastroenterol 2004; 10(19): 2859-2863
- URL: https://www.wjgnet.com/1007-9327/full/v10/i19/2859.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i19.2859