Published online Nov 6, 2021. doi: 10.12998/wjcc.v9.i31.9691
Peer-review started: July 6, 2021
First decision: July 26, 2021
Revised: August 2, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: November 6, 2021
Adrenoleukodystrophy (ALD) is caused by a deficit in the ABCD1 gene, which leads to demyelination of neurons and dysfunction of the adrenal cortices and testicles. Of the three known phenotypes, 30%-50% of male ALD patients present with the adrenomyeloneuropathy phenotype, characterized by gait disturbance as the initial symptom.
A 46-year-old man with a prior diagnosis of ALD was admitted to a Korean medicine hospital for the treatment of gait disturbance. His ability to walk was severely impaired at admission, significantly affecting the patient’s quality of life. He was treated with acupuncture, pharmacopuncture, electroacupuncture, and herbal medicine for 23 d. The 25-Foot Walk test (25FW), timed up and go (TUG), comfortable gait speed (CGS), numeric rating scale (NRS), Berg Balance Scale (BBS), Tinetti test, manual muscle test (MMT), and 3-level version of EuroQol-5 dimension (EQ-5D-3L) were used to evaluate the patient. The outcomes of the 25FW, TUG, and CGS improved during hospitalization. From the time of admission to discharge we observed: A decrease in NRS scores in the lower extremities and the lower back; an increase of 3 points in the BBS; a 1-point increase in the balancing part of the Tinetti Test; MMT and EQ-5D-3L perfor
Traditional Chinese medicine treatments could be a therapeutic option to alleviate issues related to gait disturbance in ALD.
Core Tip: A 46-year-old male patient with adrenoleukodystrophy (ALD) associated with gait disturbance was treated with acupuncture, pharmacoacupuncture, electroacupuncture, and herbal medicine with conventional medicine. Interventions improved gait speed, balance, and pain. Traditional Chinese medicine is a promising form of treatment for gait disturbance in ALD.
- Citation: Kim H, Kim T, Cho W, Chang H, Chung WS. Traditional Chinese medicine for gait disturbance in adrenoleukodystrophy: A case report and review of literature. World J Clin Cases 2021; 9(31): 9691-9698
- URL: https://www.wjgnet.com/2307-8960/full/v9/i31/9691.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i31.9691
Adrenoleukodystrophy (ALD) is one of the most common diseases in peroxisomal disorders[1]. According to a survey conducted in Japan, the prevalence is one person in every 30000–50000[2]. It is caused by a deficit in the ABCD1 gene[3,4], which is involved in the decomposition process of very-long-chain fatty acids[5]. This leads to demyelination of neurons and dysfunction of adrenals and testicles[6-8]. ALD can be divided into three phenotypes: The progressive cerebral type, adrenomyeloneuropathy, and the Addison-only phenotype[9]. Thirty to fifty percent of male ALD patients present with the adrenomyeloneuropathy phenotype, which is characterized by the presence of gait disturbance as the first symptom. This gait issue is a type of ataxia originating from the spine, similar to that of multiple sclerosis or acute sensory neuropathy. These patients walk while looking at the floor to compensate for the loss of proprioception; in other words, they lose balance upon closing their eyes[10]. Symptoms of spasticity, weakness, and pain in the lower extremities also follow[11]. For the treatment of gait disturbance in ALD, oral baclofen is prescribed; however, a high dose of baclofen is required, which could cause lethargy or nausea. For these reasons, intrathecal baclofen has been tested in patients, although relevant publications to date are limited to case reports[12-14]. Additionally, because the patho
A traditional Chinese medicine (TCM) has been used for the treatment of ALD, although at the time of writing, only one case report[17] has been published. In addition, the parameters were not properly evaluated before and after intervention, making it difficult to discuss its implications and draw conclusions. For TCM treatment of gait disturbance in other diseases, a randomized controlled trial[18] concluded that acupuncture improved gait speed and walking function in 27 patients with Parkinson’s disease. The use of TCM for the treatment of multiple sclerosis has also been reported, with at least partially beneficial results[19-21]. A systematic review and meta-analysis[22] reported that TCM can improve gait disturbance in cerebrovascular disease. In this case report, we treated an ALD patient with gait disturbance by applying TCM and evaluated the outcome using various assessment tools before and after intervention. We provide a detailed description of the patient and outcomes of our treatment.
A 46-year-old man was admitted to a Korean medicine hospital in 2020 for the treatment of gait disturbance.
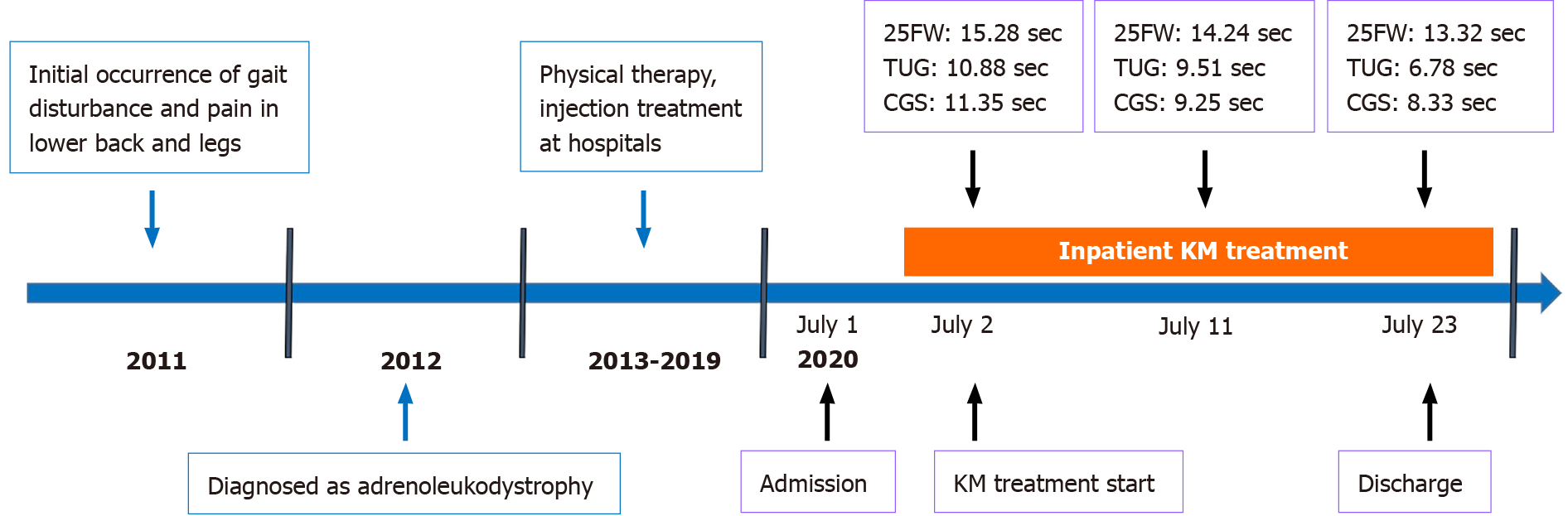
The patient visited a hospital in 2011 (39 years old at the time) with symptoms of gait disturbance, lower back pain, and pain in both legs immediately after a car accident. Medical professionals did not consider these symptoms to be caused by the accident because of the mildness of this traumatic event. Additional symptoms of dysuria and bowel obstruction were observed. Finally, the patient underwent gene testing and was diagnosed with ALD in 2012. Although he continued to receive rehabilitative treatment, botulinum toxin injections, and oral medications, including afloqualone, acetyl-L-carnitine, pramipexole dihydrochloride monohydrate, and clonazepam, the gait-related symptoms had not improved. Specifically, the oral medication did not lead to any improvement in his gait-related symptoms; thus, the patient stopped taking it of his own accord. His condition did not worsen after discontinuing oral medication.
The patient didn’t have any previous medical history.
He could not walk for 5 min and could not climb three steps in one attempt. He presented with a duck-waddle gait, moving the body from one side to another, and had poor scores in the 25-Foot Walk test (25FW), timed up and go (TUG) test, and comfortable gait speed (CGS) test (Table 1).
| Date | 25FW (s) | TUG (s) | CGS (s) | NRS | BBS | Tinetti test | MMT | EQ-5D | EQ-VAS | |
| LBP | Leg pain | |||||||||
| 7/1 | 15.28 | 10.88 | 11.35 | 4 | 3 | 45 | 20 | G/G | 22222 | 50 |
| 7/5 | 15.17 | 9.97 | 10.50 | 4 | 2 | - | - | - | - | - |
| 7/8 | 14.73 | 9.96 | 10.39 | 4 | 2 | - | - | - | - | - |
| 7/11 | 14.24 | 9.51 | 9.25 | 4 | 2 | - | - | - | - | - |
| 7/14 | 14.24 | 9.3 | 9.14 | 4 | 2 | - | - | - | - | - |
| 7/17 | 14.02 | 8.51 | 9.21 | 3 | 1 | - | - | - | - | - |
| 7/20 | 13.35 | 7.75 | 8.92 | 3 | 1 | - | - | - | - | - |
| 7/23 | 13.32 | 6.78 | 8.33 | 3 | 1 | 48 | 21 | G/G | 22222 | 50 |
From the gene testing, he was diagnosed with ALD. Other laboratory examinations including liver function tests were normal.
His previous medical records showed normal electromyography, normal chest radiography, normal brain magnetic resonance imaging (MRI), and mild disc bulging at C3-6, and annular fissure to the right central part of L5-S1 on spinal MRI.
“I was diagnosed with ALD in 2012. Subsequently, I visited many large-scale university hospitals and experienced various kinds of doctors and treatments. However, there has been almost no improvement. I felt that my gait disturbance gradually worsened. I felt like I was grasping at straws and visited the Korean medicine hospital. After admission, it did not improve for about a week. I was even thinking of transferring to other hospitals. After approximately one week, I felt a slight change in the movement of my ankles during walking. It felt like I had a little more power in the movement. Subsequently, lower back pain and leg pain improved. The reduction of pain allowed me to walk more easily. I could not walk for 5 min when I was admitted, but at the second week of hospitalization, I could walk for about 30 min without resting. In the third week, I could walk up six floors and was very surprised at my change because I could only walk up two steps before admission. I think I can hang out easily at home with my family with a comfortable mind. I look forward to going back home in a far better condition.”
After gene testing, the patient was diagnosed with ALD.
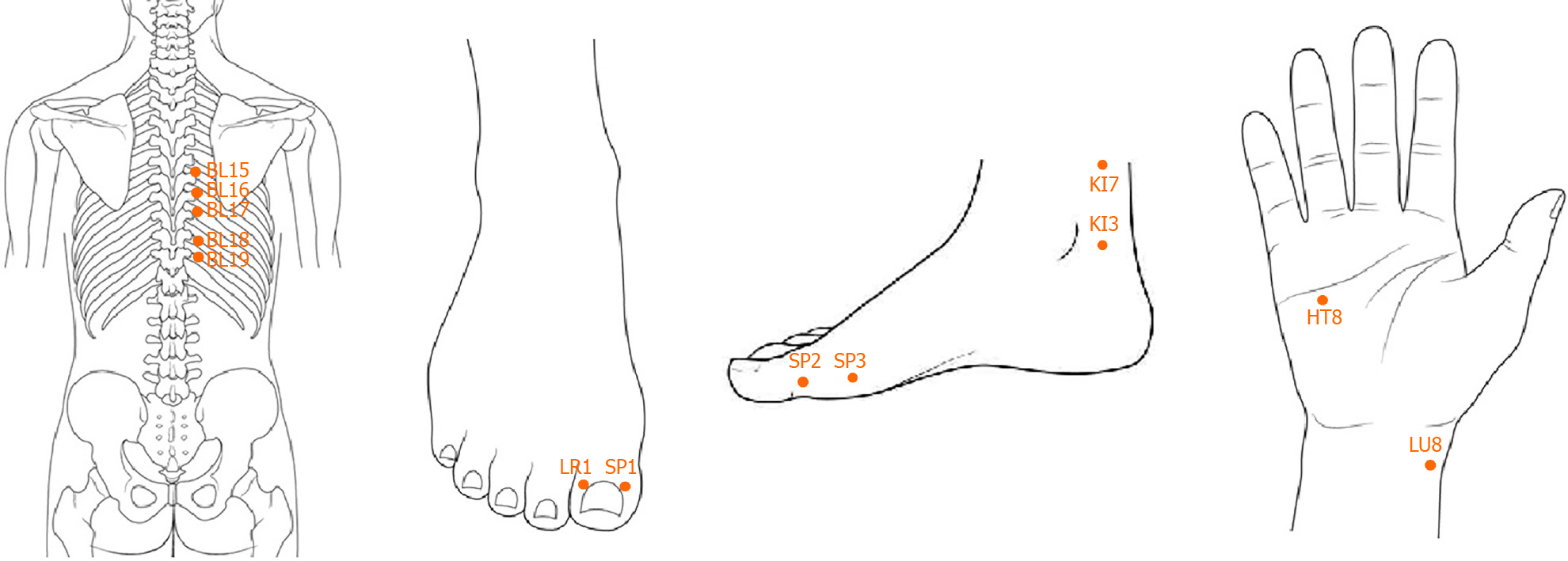
Disposable stainless-steel needles (0.25 mm × 40 mm, DongBang Acupuncture Inc., Boryung, South Korea) were inserted once every day during hospitalization at the acupoints for spleen tonification (HT8, SP2, LR1, SP1) and kidney tonification (LU8, KI7, SP3, KI3), as dictated by Saam acupuncture[23] (Figure 1).
Pharmacopuncture is a TCM method in which fluid extracted from herbal medicine is injected into acupoints using a syringe, thus combining the effects of both acupuncture and herbal medicine[24]. Jungsongouhyul pharmacopuncture distilled from Gardenia jasminoides, Corydalis tuber, Olibanum, Mastic, Commiphora myrrha, Semen Persicae, Paeonia lactiflora Pall., Salvia miltiorrhiza Bunge, and Caesalpinia sappan Linnaeus, was injected along the acupoints (BL15, BL16, BL17, BL18, BL19) on both sides of the spine subcutaneously (Figure 1). A dose of 0.1 mL was administered at each point once daily.
Electroacupuncture is the application of electrical stimulation with a small electric current to acupuncture needles[25]. It can improve the electrical stimulus of certain physiological reactions, and may thus provide a more rapid analgesic effect[26]. Disposable stainless steel needles (0.25 mm × 40 mm, DongBang Acupuncture Inc., Boryung, South Korea) were inserted to a depth of 20 mm at ST36, ST37, SP10, ST34 bilaterally, and electrical stimulation (STN-111, Stratek Inc., Anyang, South Korea) was applied to the needles at a frequency of 4 Hz (the electrical intensity of visible muscle contraction) for 20 min, once per day for 6 d per week during hospitalization.
Jinmutanggagam, an herbal medicine consisting of Radix Aconiti Lateralis Preparata, Acanthopanax Radicis Cortex, Cibotium barometz, Cannabis Fructus, Poria cocos Wolf, Paeonia lactiflora Pall., Atractylodes rhizoma Alba, Zingiberis rhizoma Crudus, and Aconitum jaluense, was orally administered three times daily, in accordance with TCM theory.
During the 23 d of hospitalization, the patient was treated with TCM comprising acupuncture, pharmacopuncture, electroacupuncture, and herbal medicine. Various assessment tools, such as the 25FW, TUG, CGS, numeric rating scale (NRS), berg balance scale (BBS), Tinetti test, manual muscle test (MMT) on ankles, knees, and hips, and the 3-level version of EuroQol-5 dimension (EQ-5D-3L), were used for the evaluation of gait condition, pain, and quality of life. 25FW decreased from 15.28 s to 13.32 s, TUG decreased from 10.88 s to 6.78 s, and CGS decreased from 11.35 s to 8.33 s between admission and discharge, respectively (Table 1). NRS scores for lower back pain and pain in both legs decreased, especially in the lower extremities, from 3 to 1. The BBS score increased by 3 points from 45 to 48. These changes were based on three 1-point tasks: Standing with eyes closed, standing with feet together, and standing on one foot. The Tinetti test showed a 1-point improvement from 20 to 21 in standing balance in the balance section, resulting in a change to a possible narrow stance without support. Performances in the MMT and EQ-5D-3L remained the same between admission and discharge. In addition to the results of these quantitative questionnaires, an improved ability to walk up the stairs was observed, with the patient being capable of climbing two steps at admission to six floors (approximately 150 steps) at discharge. The patient was advised to maintain activities while avoiding the occurrence of pain. The timeline for medical history and clinical outcomes is shown in Figure 2.
There were no adverse events reported by the patient or observed by the medical professionals.
After 23 d of TCM treatment, the gait function of the patient improved noticeably. The patient’s performance in the 25FW, TUG, and CGS, which were used for evaluating gait speed, continuously improved during treatment. The faster the gait speed, the lower the variation in the center of gravity of the human body, allowing the patient to walk more stably and safely[27]. In this respect, the presence of improvement in gait speed is clinically important to patients with gait disturbance. Pain is another important factor in individuals with gait problems. Bodily pain affects gait patterns, and an unnatural gait causes pain. This patient showed relief in pain in both the lower back and legs. The patient also showed improvements in balance, as demonstrated in the BBS and Tinetti test. In detail, standing for 10 s with eyes closed in the BBS and standing independently in the Tinetti test became possible at the time of discharge.
We observed no changes in the MMT between admission and discharge. Although this test assesses the strength of muscles, it consists of only six items, rendering it difficult to observe differences in this case. Whilst the patient’s muscle power did improve, unless a recovery to perfectly normal strength is reached, the MMT outcome remains the same as prior to treatment: ‘Good’. This explanation applies to the ankle, knee, and hip joints. The EQ-5D-3L also remained the same because it only comprises the three ratings ‘no problem’, ‘some problem’, and ‘unable’, which made it difficult to observe changes during the 3 wk of treatment.
We treated the patient with various TCM tools. Acupuncture with the Saam acupuncture method was conducted. This method originates from traditional Korean medicine and requires the process of diagnosis for patients based on TCM theory before the procedure. The patient showed a deficiency in the spleen and kidney, requiring a tonification method. Pharmacopuncture of the acupoints along the spine was also performed. The distilled liquid made from eight herbs eases the muscles and removes abnormal fluid in the local area[28]. In animal studies, pharmacopuncture reduced substance P and increased neurotrophic factors[29], and was shown to have neuroprotective effects in mice with traumatic brain injury[30]. The acupoints BL15-19, which pharmacopuncture was injected through, conform to anatomical areas of dorsal root ganglia. Therefore, stimulation of this area may help in the synthesis and isolation of neurotransmitters, making it possible to produce analgesic and neuroprotective effects. Electroacupuncture was conducted for the purpose of strengthening the legs. Continuous electrical stimulation to ST36 and ST37 is thought to reeducate neurons and muscles in the restoration of muscle strength[31]. The case in this study showed excessive compensatory flexion of hip and knee joints for the decreased movement of ankle joints. Stimulation was applied to strengthen the tibialis anterior muscles and to normalize the quadriceps muscles. Electroacupuncture is also known to have analgesic effects[32] and may contribute to the relief of pain in both lower extremities. The type of herbal medicine used in this case is known to be effective for patients with excessive abnormal fluid in the body, according to TCM theory. The main herb used was Radix Aconiti Lateralis Preparata, which is known to induce descending pain-inhibitory tracts by stimulating κ-opioid receptors in myelin, resulting in pain relief[33]. Neoline, one of the constituents of this herb, has been observed to exert analgesic effects in animal models of peripheral neuropathy[34]. It is therefore likely that these actions relieved the pain in the lower back and legs of the patient in the present case report.
This case study has some limitations. First, there was no follow-up evaluation after treatment completion. A longer period of observation could yield a better assessment of changes in the condition of the patient and allow insights into the long-term effects of the treatment. Second, some of the methods used to evaluate treatment outcomes had a low sensitivity to changes in the patient. Although the patient’s improvements were reflected by other assessment tools, there were no changes in the MMT and EQ-5D-3L between admission and discharge. Muscle power-measuring medical devices may be used instead in future studies.
Given the paucity of other reports regarding the TCM approach for ALD, this case report can provide a basis for treatment options for gait issues in ALD patients.
A TCM approach for the treatment of an ALD patient showed desirable results regarding gait speed, balance, and pain. Thus, TCM could be a therapeutic option for the remission of gait disturbance in ALD. In clinical settings, this approach can be used to treat affected individuals. Prospective and large-scale clinical trials need to be conducted in the future with a longer follow-up period to more thoroughly investigate the effectiveness of TCM for the treatment of ALD with gait disturbance.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beraldo RF, Moro N, Suleyman H S-Editor: Fan JR L-Editor: A P-Editor: Li X
| 1. | Engelen M, Kemp S, de Visser M, van Geel BM, Wanders RJ, Aubourg P, Poll-The BT. X-linked adrenoleukodystrophy (X-ALD): clinical presentation and guidelines for diagnosis, follow-up and management. Orphanet J Rare Dis. 2012;7:51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 299] [Cited by in F6Publishing: 320] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 2. | Takemoto Y, Suzuki Y, Tamakoshi A, Onodera O, Tsuji S, Hashimoto T, Shimozawa N, Orii T, Kondo N. Epidemiology of X-linked adrenoleukodystrophy in Japan. J Hum Genet. 2002;47:590-593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Migeon BR, Moser HW, Moser AB, Axelman J, Sillence D, Norum RA. Adrenoleukodystrophy: evidence for X linkage, inactivation, and selection favoring the mutant allele in heterozygous cells. Proc Natl Acad Sci U S A. 1981;78:5066-5070. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 195] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Mosser J, Douar AM, Sarde CO, Kioschis P, Feil R, Moser H, Poustka AM, Mandel JL, Aubourg P. Putative X-linked adrenoleukodystrophy gene shares unexpected homology with ABC transporters. Nature. 1993;361:726-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 858] [Cited by in F6Publishing: 797] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 5. | Singh I, Moser AE, Goldfischer S, Moser HW. Lignoceric acid is oxidized in the peroxisome: implications for the Zellweger cerebro-hepato-renal syndrome and adrenoleukodystrophy. Proc Natl Acad Sci U S A. 1984;81:4203-4207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 229] [Cited by in F6Publishing: 260] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Hein S, Schönfeld P, Kahlert S, Reiser G. Toxic effects of X-linked adrenoleukodystrophy-associated, very long chain fatty acids on glial cells and neurons from rat hippocampus in culture. Hum Mol Genet. 2008;17:1750-1761. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Karapanou O, Vlassopoulou B, Tzanela M, Papadopoulos D, Angelidakis P, Michelakakis H, Ioannidis G, Mihalatos M, Kamakari S, Tsagarakis S. X-linked adrenoleukodystrophy: are signs of hypogonadism always due to testicular failure? Hormones (Athens). 2014;13:146-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Whitcomb RW, Linehan WM, Knazek RA. Effects of long-chain, saturated fatty acids on membrane microviscosity and adrenocorticotropin responsiveness of human adrenocortical cells in vitro. J Clin Invest. 1988;81:185-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 122] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Jung ES, Ko A, Kang HC. X-linked adrenoleukodystrophy; recent advances in classification, diagnosis and management. J Korean Child Neuro Soc. 2016;24:71−83. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Jia MR, Wu WZ, Li CM, Cai XH, Zhang L, Yan F, Zhu C, Gu MH. Clinical characteristics and phenotype distribution in 10 Chinese patients with X-linked adrenoleukodystrophy. Exp Ther Med. 2019;18:1945-1952. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Powers JM, DeCiero DP, Cox C, Richfield EK, Ito M, Moser AB, Moser HW. The dorsal root ganglia in adrenomyeloneuropathy: neuronal atrophy and abnormal mitochondria. J Neuropathol Exp Neurol. 2001;60:493-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Hjartarson HT, Ehrstedt C, Tedroff K. Intrathecal baclofen treatment an option in X-linked adrenoleukodystrophy. Eur J Paediatr Neurol. 2018;22:178-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Hashimoto Y, Takahashi K, Yamamoto Y, Ogata T, Arai T, Okuda Y. [Anesthetic Management of an Adrenoleukodystrophy Patient for Intrathecal Baclofen Therapy]. Masui. 2016;65:392-394. [PubMed] [Cited in This Article: ] |
| 14. | Chu ML, Sala DA, Weiner HL. Intrathecal baclofen in X-linked adrenoleukodystrophy. Pediatr Neurol. 2001;24:156-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Morales-Casado MI, López-Ariztegui N, Muñoz-Escudero F, Navarro-Bejarano Á, Pérez-Matos JA. [Improvement of walking in patients with adrenoleukodystrophy treated with fampridine as a compassionate use]. Neurologia. 2021;36:393-395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Birnbaum G, Iverson J. Dalfampridine may activate latent trigeminal neuralgia in patients with multiple sclerosis. Neurology. 2014;83:1610-1612. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Lim J, Hwang MW, Ham TI, Lee SK, Koh BH, Song IB. A case of treatment of a Taeumin patient diagnosed to adrenoleukodystrophy. J Sasang Consti Med. 2004;16:155−161. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Fukuda S, Kuriyama N, Egawa M. Acupuncture for Gait Disturbance in Parkinson's Disease: Immediate Effects of Acupuncture Treatment. J Am Geriatr Soc. 2015;63:2189-2190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Mojaverrostami S, Bojnordi MN, Ghasemi-Kasman M, Ebrahimzadeh MA, Hamidabadi HG. A Review of Herbal Therapy in Multiple Sclerosis. Adv Pharm Bull. 2018;8:575-590. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Karpatkin HI, Napolione D, Siminovich-Blok B. Acupuncture and multiple sclerosis: a review of the evidence. Evid Based Complement Alternat Med. 2014;2014:972935. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 21. | Criado MB, Santos MJ, Machado J, Gonçalves AM, Greten HJ. Effects of Acupuncture on Gait of Patients with Multiple Sclerosis. J Altern Complement Med. 2017;23:852-857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Chen BL, Guo JB, Liu MS, Li X, Zou J, Chen X, Zhang LL, Yue YS, Wang XQ. Effect of Traditional Chinese Exercise on Gait and Balance for Stroke: A Systematic Review and Meta-Analysis. PLoS One. 2015;10:e0135932. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Park M, Kim S. A Modern Clinical Approach of the Traditional Korean Saam Acupuncture. Evid Based Complement Alternat Med. 2015;2015:703439. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Korean Pharmacopuncture Institute. Pharmacopuncturology. Seoul: Elsevier Korea, 2011. [Cited in This Article: ] |
| 25. | Liu AJ, Li JH, Li HQ, Fu DL, Lu L, Bian ZX, Zheng GQ. Electroacupuncture for Acute Ischemic Stroke: A Meta-Analysis of Randomized Controlled Trials. Am J Chin Med. 2015;43:1541-1566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | Han JS. Electroacupuncture: an alternative to antidepressants for treating affective diseases? Int J Neurosci. 1986;29:79-92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 61] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Orendurff MS, Segal AD, Klute GK, Berge JS, Rohr ES, Kadel NJ. The effect of walking speed on center of mass displacement. J Rehabil Res Dev. 2004;41:829-834. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 187] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 28. | Park J, Lee H, Shin BC, Lee MS, Kim B, Kim JI. Pharmacopuncture in Korea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2016;2016:4683121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Jung MJ, Lee JH, Yeom SR, Lee SK, Song YS, Kim KB, Kwon YD. Effects of Ohyaksungi-san (Wuyaoshungi-san) and Jungsongouhyul pharmacopuncture on pain reduction and nerve regeneration after crush injury in rat sciatic nerve. J Korean Med Rehabil. 2009;19:51−72. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Jong IM, Choi JB. Neuroprotective effects of neutral pharmacopuncture for blood stasis and Tangguisusangami-tang(Dangguixusanjiawei-tang) in the experimental traumatic brain injury rats. J Oriental Rehab Med. 2010;20:13−26. [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Huang LP, Zhou S, Lu Z, Tian Q, Li X, Cao LJ, Yu JH, Wang H. Bilateral effect of unilateral electroacupuncture on muscle strength. J Altern Complement Med. 2007;13:539-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. 2014;120:482-503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 466] [Cited by in F6Publishing: 454] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 33. | Shu H, Arita H, Hayashida M, Chiba S, Sekiyama H, Hanaoka K. Inhibition of morphine tolerance by processed Aconiti tuber is mediated by kappa-opioid receptors. J Ethnopharmacol. 2006;106:263-271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Kawaguchi M, Satoh Y, Otsubo Y, Kazama T. Molecular hydrogen attenuates neuropathic pain in mice. PLoS One. 2014;9:e100352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |