Copyright
©The Author(s) 2021.
World J Clin Cases. Jul 6, 2021; 9(19): 5028-5036
Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5028
Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5028
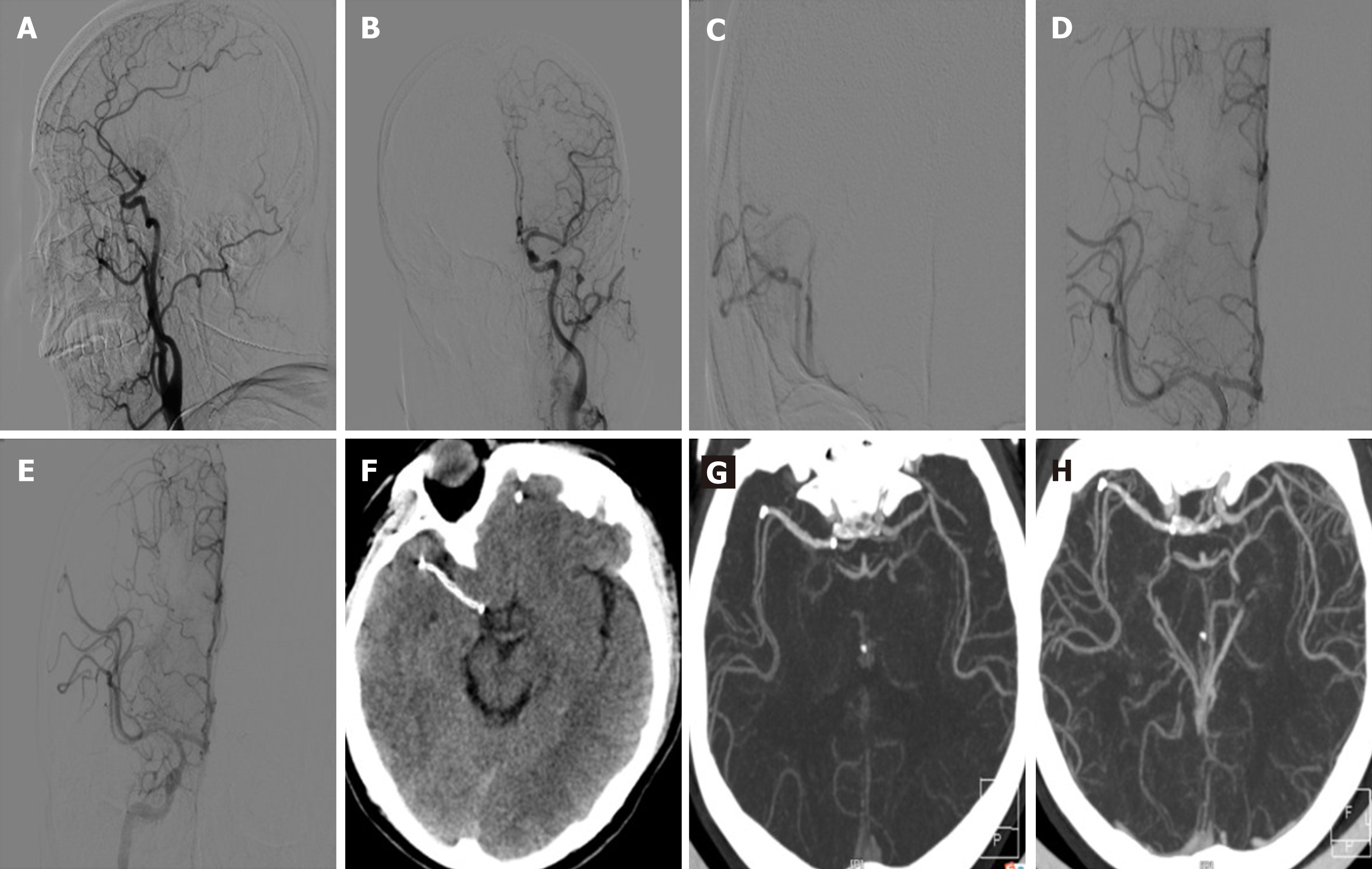
Figure 2 A 54-year-old male was admitted to the hospital with numbness and weakness in his left limb for 1 h.
His admission National Institutes of Health Stroke Scale (NIHSS) score was 14 points, rt-PA intravenous thrombolysis after bridging endovascular treatment was performed, and immediately after surgery his NIHSS score was 2 points. The modified Rankin scale score was 0 points after 3 mo. A: Digital subtraction angiography lateral view shows proximal occlusion of the right middle cerebral artery; B: Left internal carotid artery angiography shows that the left anterior middle cerebral artery blood circulation was unobstructed; C: Micro-catheter angiography confirmed that the far end of the right middle cerebral artery was unobstructed; D: The Solitaire AB stent (4 mm × 20 mm) was unfolded (before being released) and the distal blood flow modified thrombolysis in cerebral infarction was above 2b/3; E: The distal blood flow was maintained after 15 min. The Solitaire AB stent was released; F: Immediately after surgery, there was no bleeding observed on head computed tomography (CT), and the shape of the stent was visible; G: Three days postoperatively, CT angiography (CTA) showed that the Solitaire AB stent was in good shape and the distal blood flow was smooth; H: The 3-month re-examination by CTA showed that the stent was in good shape and the distal blood flow was smooth.
- Citation: Wang XF, Wang M, Li G, Xu XY, Shen W, Liu J, Xiao SS, Zhou JH. Efficacy of Solitaire AB stent-release angioplasty in acute middle cerebral artery atherosclerosis obliterative cerebral infarction. World J Clin Cases 2021; 9(19): 5028-5036
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5028.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5028