Published online Mar 26, 2020. doi: 10.12998/wjcc.v8.i6.1129
Peer-review started: December 11, 2019
First decision: January 17, 2020
Revised: January 30, 2020
Accepted: March 11, 2020
Article in press: March 21, 2020
Published online: March 26, 2020
Processing time: 105 Days and 10.8 Hours
Systemic sclerosis is a rare connective tissue disease characterized by localized or diffuse skin thickening and fibrosis, which usually accumulates in various organs throughout the body. Tachyarrhythmia is a common clinical manifestation of cardiovascular damage in systemic sclerosis patients. However, few studies have reported the use of catheter ablation and an implantable cardioverter defibrillator in patients with systemic sclerosis complicated by ventricular tachycardia.
A 39-year woman with an 11-year history of systemic sclerosis was referred to our hospital due to three syncopal episodes in the past 6 mo. The results of an electrocardiogram and a transthoracic echocardiogram revealed ventricular tachycardia and left ventricular systolic and ventricular septum segmental motion abnormalities, respectively. The results of an electrocardiogram showed a sinus rhythm with complete blockage of the left bundle branch. In light of the progressive nature of systemic sclerosis, the presence of a left bundle branch block, and the decreased ejection fraction, a cardiac resynchronization therapy-defibrillator was implanted. The patient’s clinical conditions improved, and at the 3-mo follow-up, the patient was free of ventricular tachycardia and all cardiac symptoms.
We report the first case of systemic sclerosis complicated by ventricular tachycardia that was successfully treated with a cardiac resynchronization therapy-defibrillator.
Core tip: Systemic sclerosis, a rare connective tissue disease, associates with various cardiovascular diseases. Tachyarrhythmia is a common clinical manifestation of cardiovascular damage in systemic sclerosis patients, and the occurrence of ventricular abnormalities is closely correlated with death. We report the first successful case of cardiac resynchronization therapy-defibrillator implantation in a patient with systemic sclerosis complicated by ventricular tachycardia.
- Citation: Chen YY, Yan H, Zhu JH. Successful treatment of systemic sclerosis complicated by ventricular tachycardia with a cardiac resynchronization therapy-defibrillator: A case report. World J Clin Cases 2020; 8(6): 1129-1136
- URL: https://www.wjgnet.com/2307-8960/full/v8/i6/1129.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i6.1129
Systemic sclerosis is a rare connective tissue disease characterized by localized or diffuse skin thickening and fibrosis, which usually accumulates within various organs throughout the body. It can be classified into two subtypes: Diffuse cutaneous systemic sclerosis and limited cutaneous systemic sclerosis. Systemic sclerosis patients also present with various cardiovascular diseases, with myocardial fibrosis revealed in 80% of subjects during autopsy[1]. Tachyarrhythmia is a common clinical manifestation in systemic sclerosis patients. In a previous study, 24-h Holter recordings were carried out on 183 patients with systemic sclerosis. Ventricular ectopic beats were observed in 67% of the patients, and ventricular tachycardia was noticed in 7% of the patients. Most importantly, the occurrence of ventricular abnormalities has been reported to be closely associated with death[2].
A 39-year-old woman with a history of systemic sclerosis was admitted to our hospital for treatment following three syncopal episodes within the past 6 mo.
The patient’s cardiac symptoms started 6 mo ago and worsened in the past 1 mo.
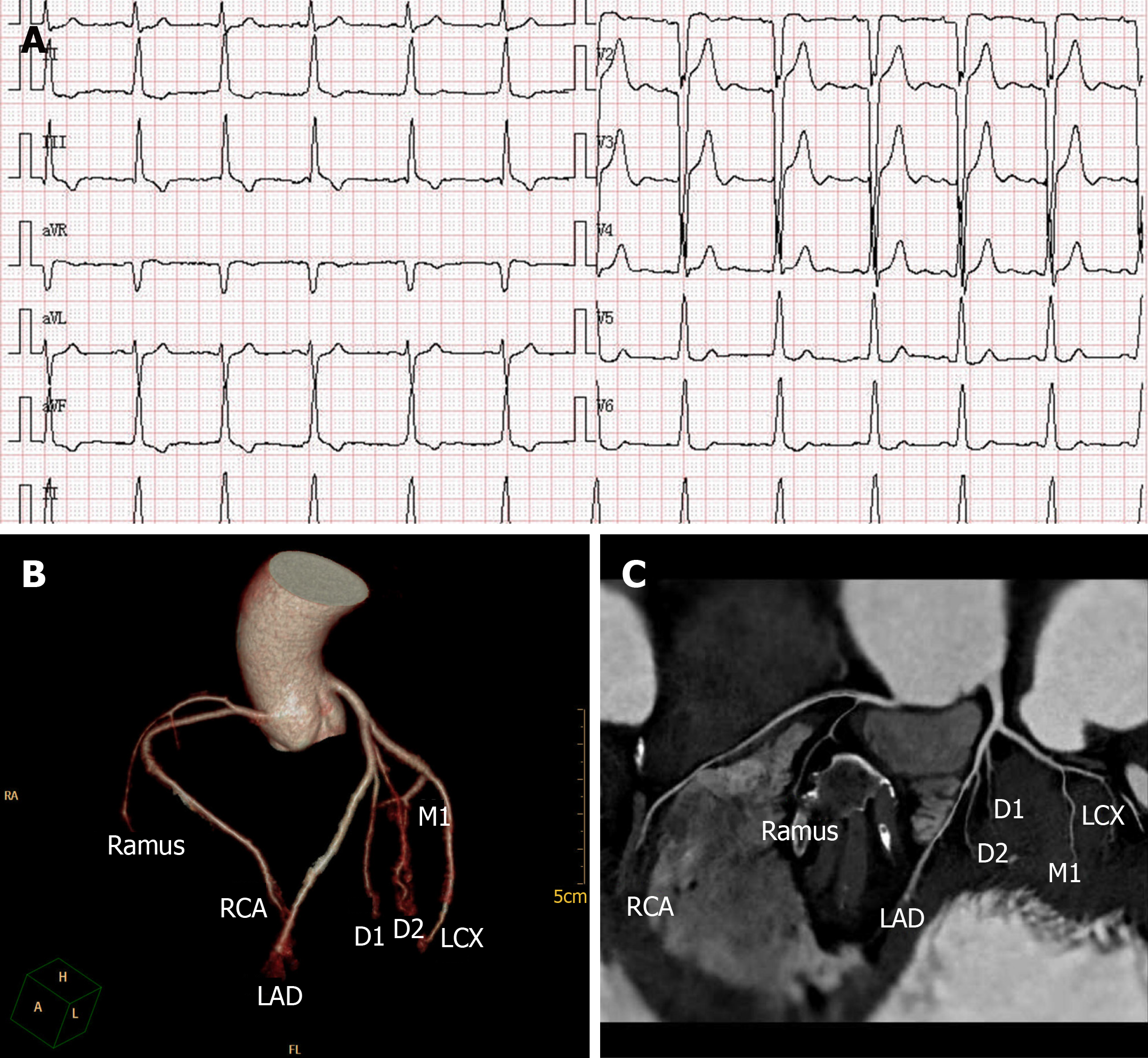
The patient was diagnosed with diffuse systemic sclerosis based on Raynaud’s phenomenon and presented with pain; sclerodactyly; sclerotic changes extending from the fingers to the forearms, as well as on the face and trunk; and positive results of an anti-Scl70 antibody test and a skin biopsy at our hospital 11 years ago. Timeline of the diagnosis and treatment is shown in Table 1. The patient was well controlled by treatment with prednisone, colchicine, and hydroxychloroquine until 2017, after which her conditions progressively worsened. The results of an electrocardiogram (ECG) at rest showed a sinus rhythm with QS waves from V1 to V3, an intraventricular conduction block (QRS duration, 118 ms), and a change of the ST-T wave (Figure 1A). The results of a transthoracic echocardiogram (TTE) showed left ventricular diastolic dysfunction, normal left ventricular systolic function with an ejection fraction of approximately 59%, and tachycardia. The results of coronary computed tomography angiography showed no abnormality (Figure 1B and C), whereas those of chest computed tomography showed lung nodules. The cardiothoracic ratio was 54%. In laboratory tests, the serum creatine kinase level was 323 IU/L, and the creatine kinase-muscle brain level was 31 IU/L. The erythrocyte sedimentation rate was 30 mm/h, and the cardiac troponin I level was 0.613 ng/mL. The patient’s clinical conditions improved greatly after treatment with prednisone and aspirin.
| Time | Events |
| 2007 | The patient was diagnosed with diffuse systemic sclerosis based on Raynaud’s phenomenon, sclerotic changes, and positive results of an anti-Scl70 antibody test and a skin biopsy |
| 2017 | The patient’s conditions progressively worsened and electrocardiogram at rest showed a sinus rhythm with QS waves from V1 to V3, and an intraventricular conduction block |
| January-June 2019 | The patient had three syncopal episodes, electrocardiogram revealed monomorphic wide QRS complex ventricular tachycardia, and she was recovered from syncope by electrocardiography |
| July 2019 | Electrocardiogram showed sinus rhythm with complete left bundle branch block (QRS duration 126 ms), and the patient was successfully treated with a cardiac resynchronization therapy-defibrillator (St. Jude Medical Unify CD3231-40) on July 25, 2019 |
The patient was a farmer and had no family history of any major diseases.
The patient had New York Heart Association class II cardiac status. A physical examination revealed Raynaud’s phenomenon, skin tightening, waxy luster, depressed scars, escharosis of the fingertips, and a facial rash. The heart rate ranged from 60 to 90 bpm, and the blood pressure was 92/58 mmHg. On auscultation, no cardiac murmur was detected.
Besides microcytic hypochromic anemia (hemoglobin level, 110 g/L), the results of laboratory tests were normal. Antinuclear antibodies were present at a titer of 1:80, and the patient was positive for the anti-Scl-70 antibody.
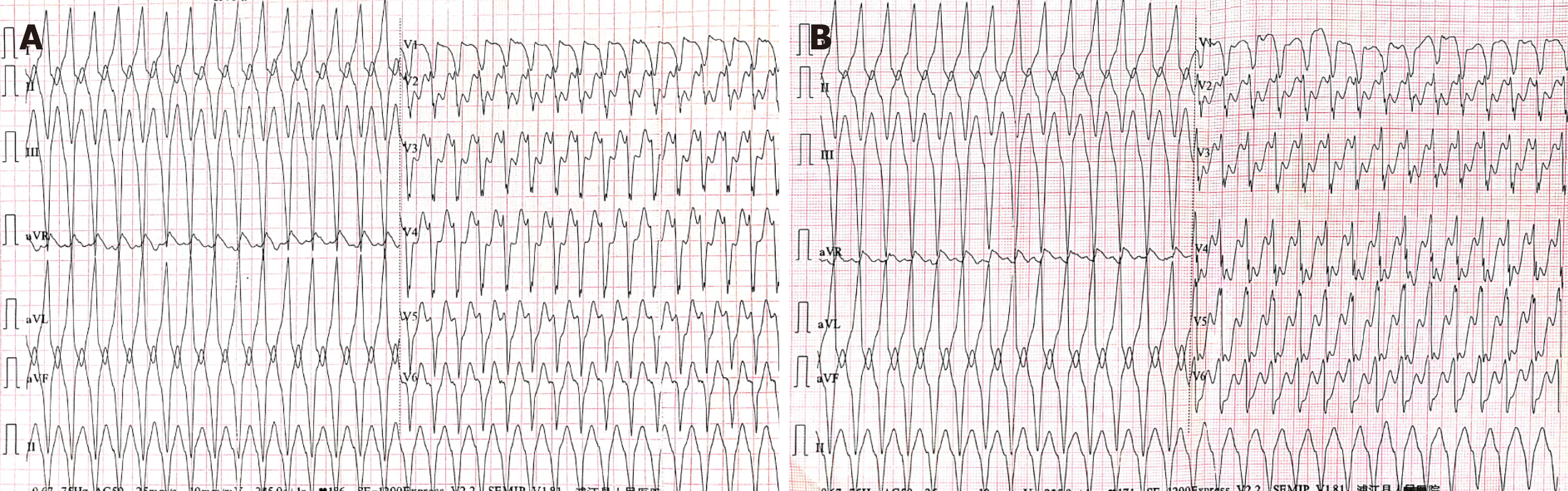
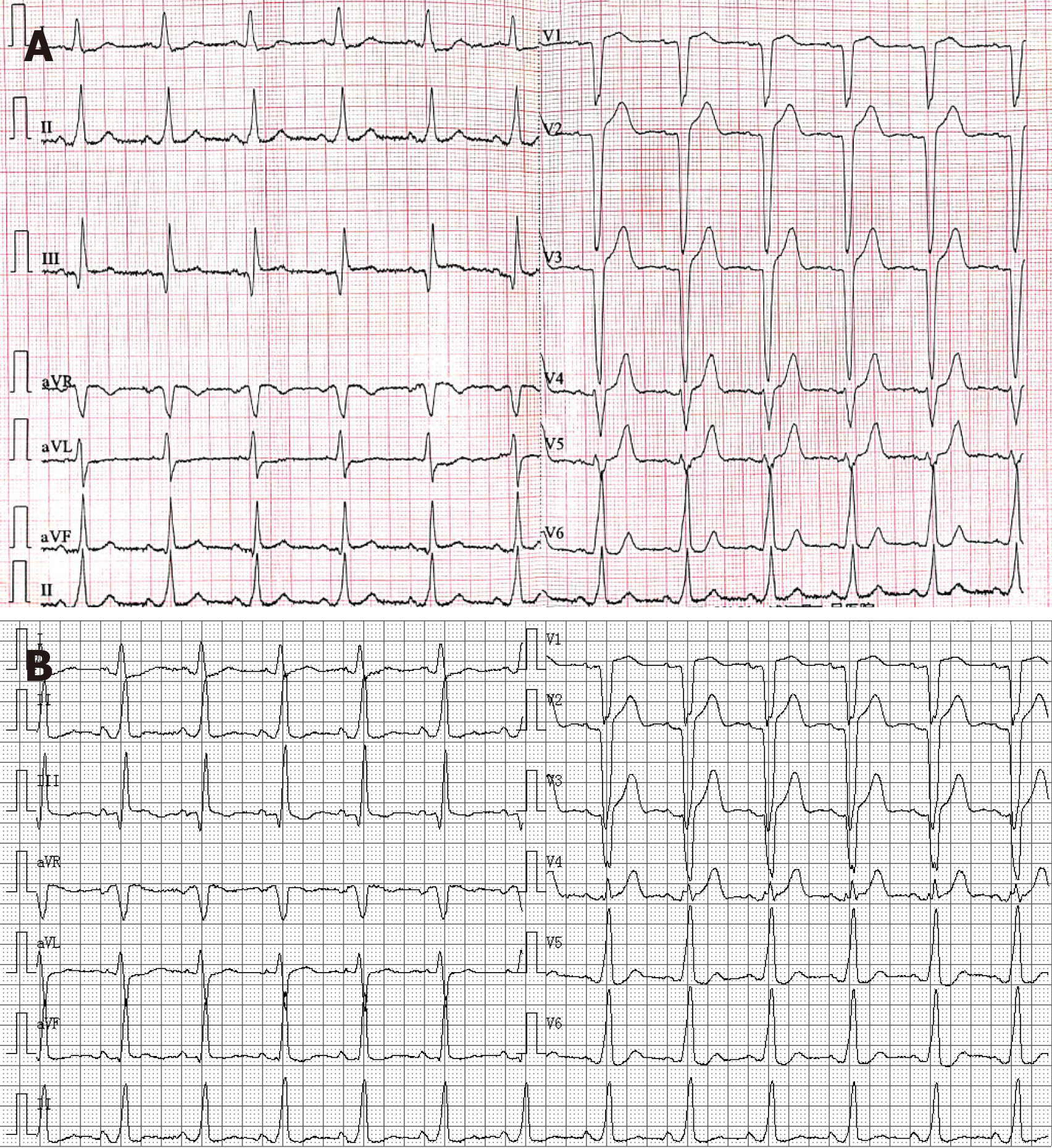
The results of an ECG performed during attack revealed monomorphic wide QRS complex ventricular tachycardia with a heart rate of 186 bpm (Figure 2A and B). The results of TTE showed left ventricular systolic dysfunction with an ejection fraction of 44% and ventricular septum segmental motion abnormalities. The patient recovered from syncope by electrocardiography at a local hospital and electrocardiogram recorded sinus rhythm and left bundle branch block (LBBB) (QRS duration, 143 ms) (Figure 3A).
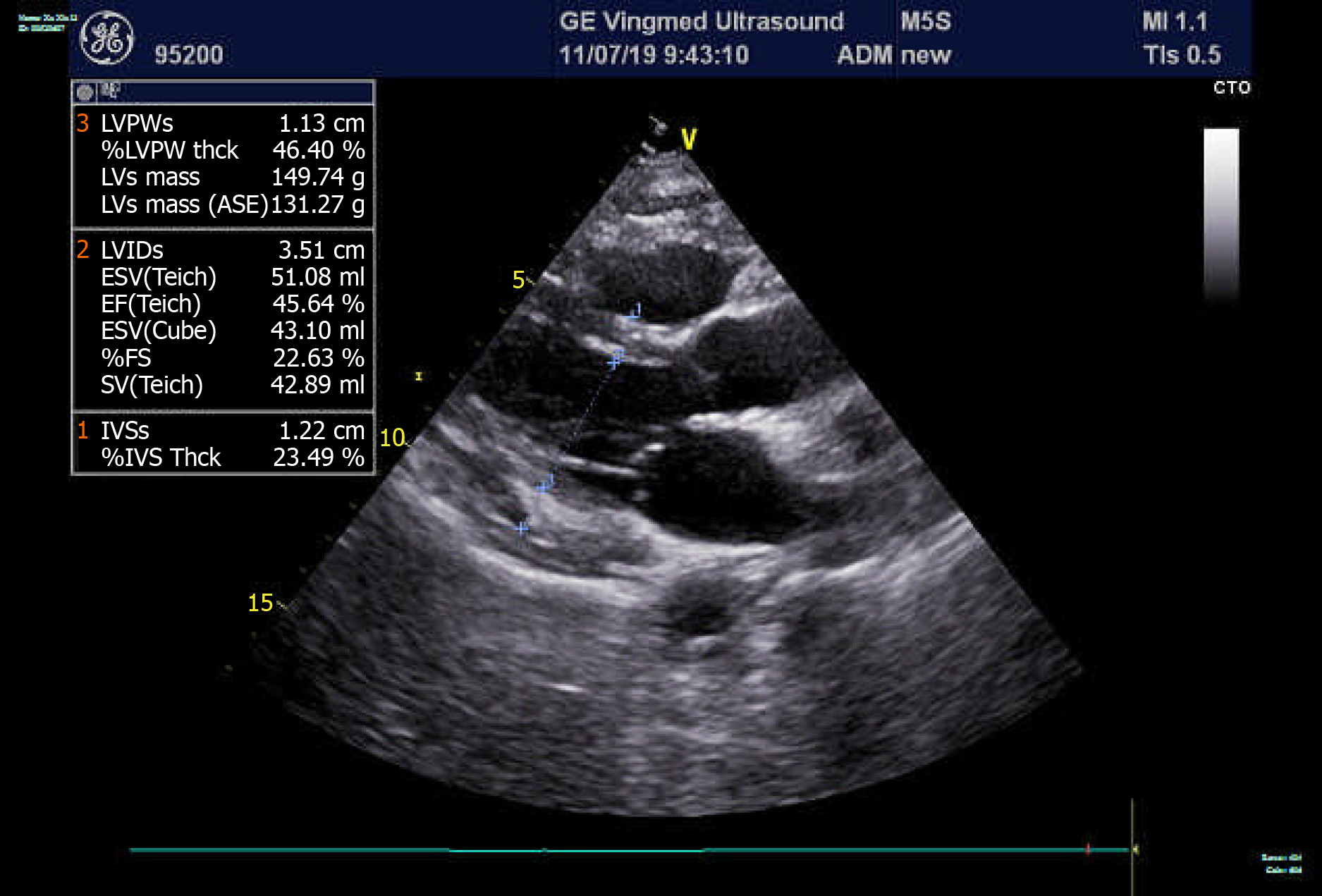
The results of an ECG performed during hospitalization showed a sinus rhythm with complete LBBB (QRS duration, 126 ms). The heart rate was 74 bpm (Figure 3B). The results of TTE showed a normal left ventricular ejection fraction (LVEF) of 58% and normal cardiac chamber size with no structural abnormality of both ventricles (Figure 4). The results of a chest X-ray showed a cardiothoracic ratio of 58%.
Based on these findings, the final diagnosis was ventricular tachycardia caused by systemic sclerosis.
In light of the progressive nature of systemic sclerosis, the presence of LBBB, and the decreased ejection fraction, the patient was successfully treated with a cardiac resynchronization therapy-defibrillator (St. Jude Medical Unify CD3231-40) on July 25, 2019.
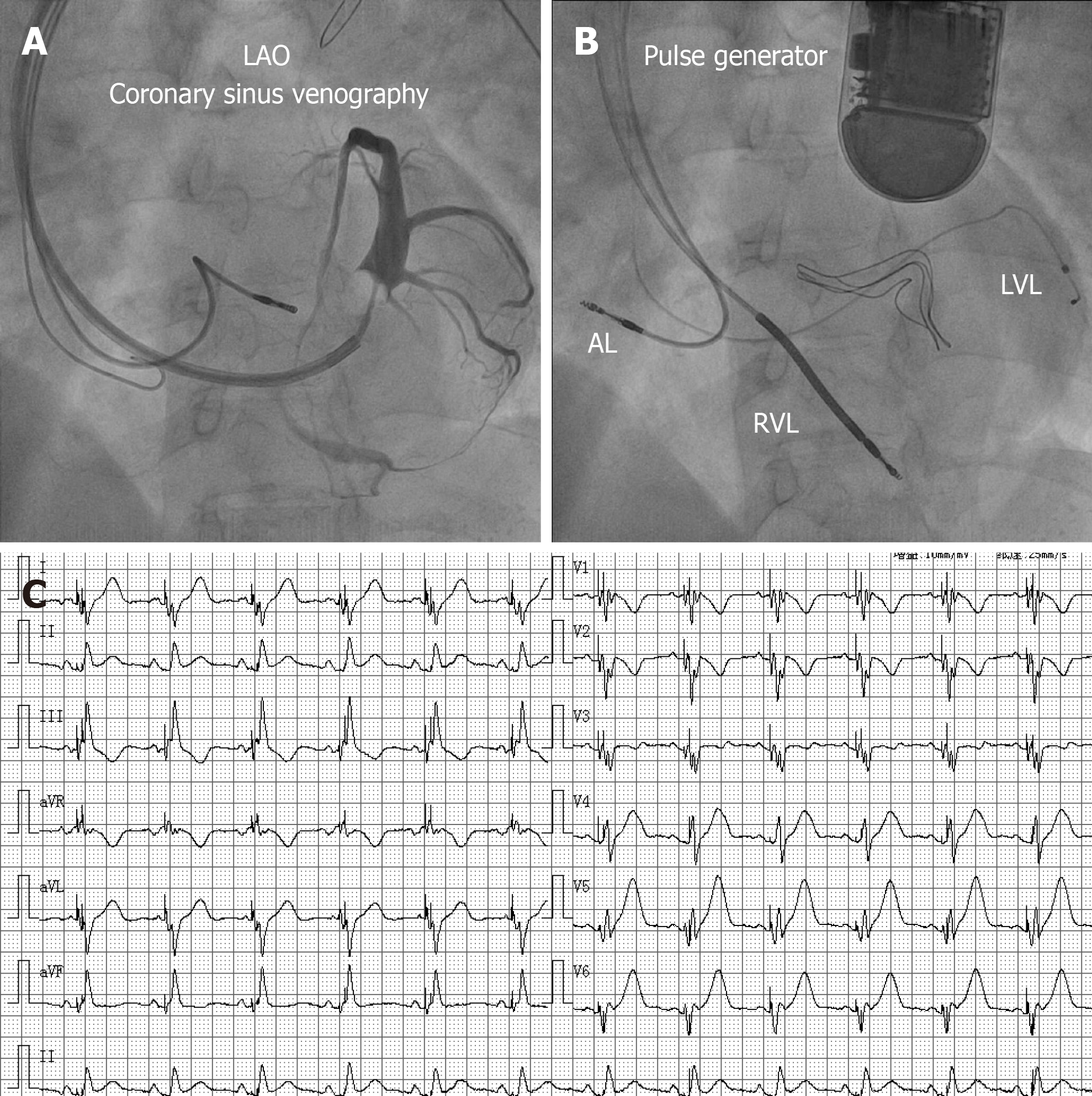
Implantation was performed under conscious sedation. We performed sinus venography from a left anterior oblique 30° angle and obtained images of the coronary vein. The target vein was subsequently identified (Figure 5A). The leads were advanced through the guidewire towards the right atrium and both ventricles. After setting the parameters of the cardiac resynchronization therapy-defibrillator, the leads were connected to the pulse generator (Figure 5B). Bisoprolol, methylpred-nisolone, amiodarone, and aspirin were started after the procedure.
The results of an ECG showed biventricular pacing and a reduction of the QRS complex duration by 22 ms (from 126 ms to 104 ms) after successful implantation of the cardiac resynchronization therapy-defibrillator (Figure 5C). During hospitalization, there was no syncopal episode, and the patient’s clinical conditions improved greatly.
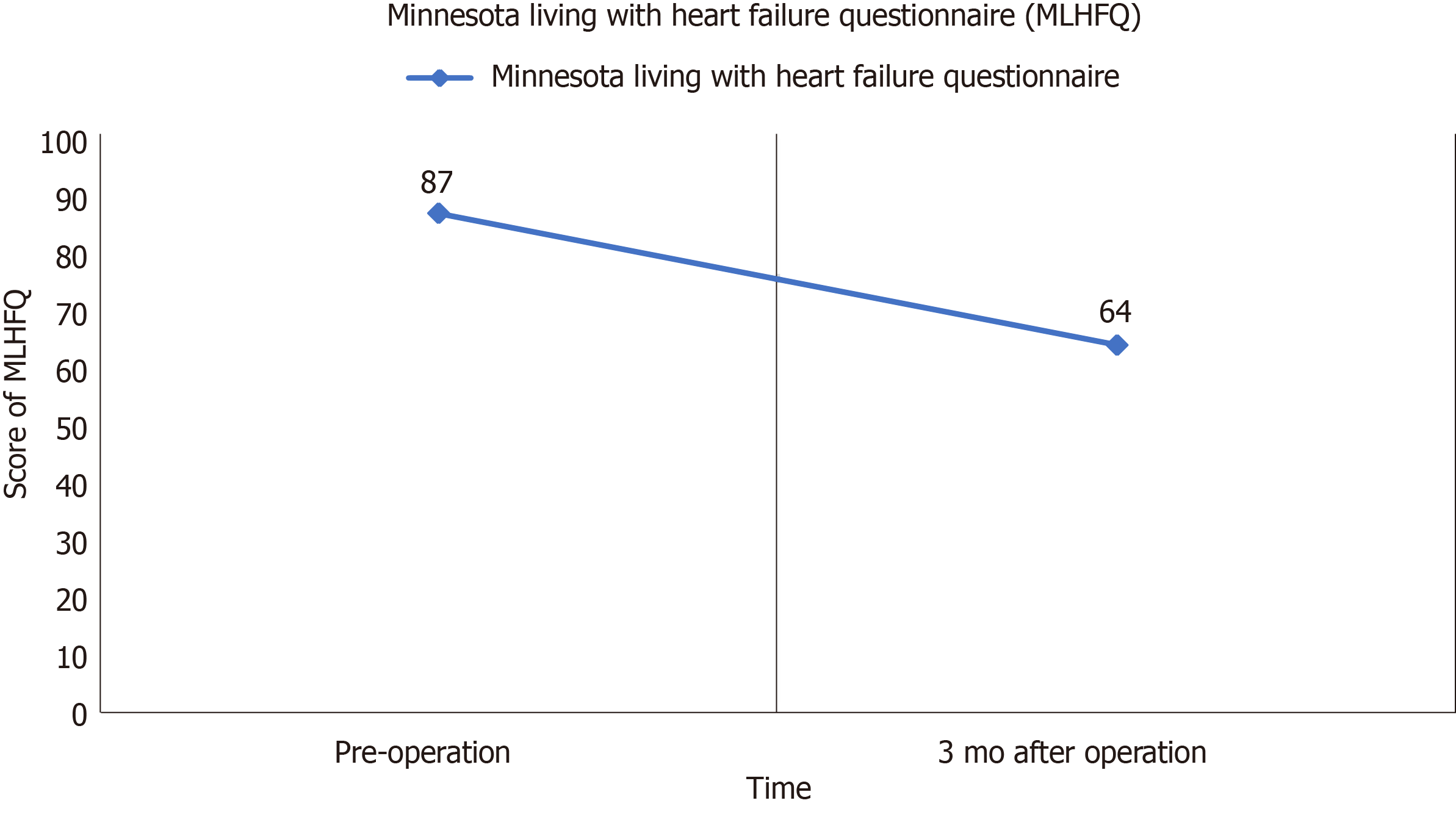
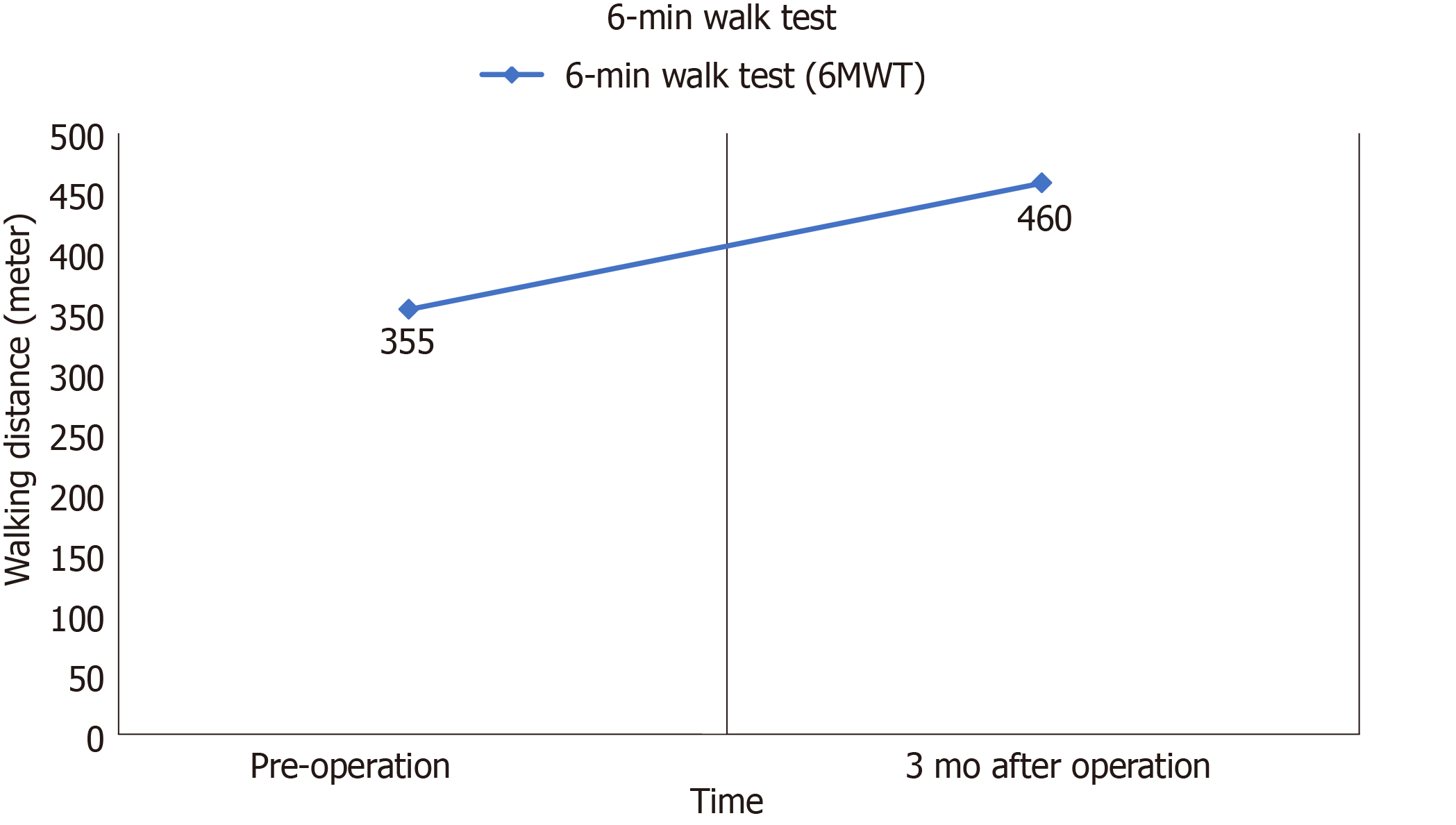
At the 3-mo follow-up, the patient reported an improvement in exercise tolerance and no cardiac symptoms (Figures 6 and 7) or ventricular tachycardia were observed. The last interrogation (October 2019) revealed a biventricular capture rate > 99%, with no ventricular tachycardia/ventricular fibrillation episodes. At the time of this writing (November 2019), the patient’s clinical conditions were stable.
We describe a case of hemodynamically unstable ventricular tachycardia with an 11-year history of systemic sclerosis that was treated with a cardiac resynchronization therapy-defibrillator. To the best of our knowledge, this is the first report of sustained monomorphic ventricular tachycardia treatment with a cardiac resynchronization therapy-defibrillator. Previous reports have described the successful treatment of systemic sclerosis patients by catheter ablation and an implantable cardioverter defibrillator for ventricular tachycardia. In 1977, John and colleagues reported the first case of using a cryoprobe to ablate drug-resistant ventricular tachycardia in a systemic sclerosis patient by surgery[3]. Subsequently, the first implantable cardioverter defibrillator was used to treat patients with systemic sclerosis complicated by ventricular tachycardia[4]. Seven systemic sclerosis patients with sustained ventricular tachycardia were successfully treated by endocardial catheter mapping and transcatheter ablation in four studies from 1999 to 2012. At the 1-mo follow-up, only one patient died of cardiogenic shock after ablation. The remaining patients did not experience ventricular tachycardia episodes after ablation. These studies demonstrate that catheter ablation is safe and effective for systemic sclerosis patients with sustained ventricular tachycardia[5-8]. Marsico and colleagues reported that ten systemic sclerosis patients with heart involvement received an implantable cardioverter defibrillator. Three out of the ten patients experienced ventricular tachycardia but recovered after electric shock. Their clinical conditions were improved at the 36-mo follow-up. Our results indicate that an implantable cardioverter defibrillator may prevent sudden cardiac death in patients with systemic sclerosis complicated by ventricular tachycardia[9].
Cardiac resynchronization therapy, which is primarily used for the treatment of patients with heart failure, can improve cardiac performance, alleviate cardiac symptoms, improve quality of life, and reduce morbidity and mortality. The high-level recommendations for cardiac resynchronization therapy in the 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure are mainly for symptomatic patients with a QRS duration >130 ms, a LBBB QRS morphology, and an LVEF ≤ 35% despite optimal medical therapy[10]. A cardiac resynchronization therapy-defibrillator was implanted for several reasons. First, our patient had a LBBB QRS morphology in the sinus rhythm and a progressive increase of the QRS duration that reached 126 ms in two years. Second, our patient complained of breathlessness, tiredness, and reduced exercise tolerance, which are typical symptoms of heart failure, and the patient had NYHA class II cardiac status. Third, the results of an ultrasound cardiogram revealed left ventricular dyssynchrony. Due to the pathological characteristics of scleroderma, it can cause myocardial fibrosis, coronary microvascular damage, and paralysis, which can eventually lead to aggravation of heart failure.
The patient was not a candidate for cardiac ablation because ventricular tachycardia was not induced. Furthermore, the results of the ECG indicated that ventricular tachycardia originated from the right ventricular apex. Due to the poor hemodynamic tolerance and very high heart rate usually reached during tachycardia, successful ablation is uncommon in cases of tachycardia. Thus, the patient was treated by cardiac resynchronization therapy after consultation with members of her family.
Although cardiac resynchronization therapy is not generally recommended for patients with a QRS duration < 130 ms, a LBBB QRS morphology, and an LVEF > 35%, our patient showed improvement of symptoms and quality of life at the 3-mo follow-up, indicating that the therapy has a potential application in patients with systemic sclerosis complicated by ventricular tachycardia. Further studies are needed to evaluate the long-term complications and treatment outcomes.
In conclusion, we report the first case of systemic sclerosis complicated by ventricular tachycardia successfully treated with a cardiac resynchronization therapy defibrillator. Further studies are needed to explore the application of this therapy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barik R, Pastromas S S-Editor: Gong ZM L-Editor: Wang TQ E-Editor: Xing YX
| 1. | Fernandes F, Ramires FJ, Arteaga E, Ianni BM, Bonfá ES, Mady C. Cardiac remodeling in patients with systemic sclerosis with no signs or symptoms of heart failure: an endomyocardial biopsy study. J Card Fail. 2003;9:311-317. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Kostis JB, Seibold JR, Turkevich D, Masi AT, Grau RG, Medsger TA, Steen VD, Clements PJ, Szydlo L, D'Angelo WA. Prognostic importance of cardiac arrhythmias in systemic sclerosis. Am J Med. 1988;84:1007-1015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in RCA: 96] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Gallagher JJ, Anderson RW, Kasell J, Rice JR, Pritchett EL, Gault HJ, Harrison L, Wallace AG. Cryoablation of drug-resistant ventricular tachycardia in a patient with a variant of scleroderma. Circulation. 1978;57:190-197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in RCA: 121] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Martinez-Taboada V, Olalla J, Blanco R, Armona J, Sueiro JF, Rodriguez-Valverde V. Malignant ventricular arrhythmia in systemic sclerosis controlled with an implantable cardioverter defibrillator. J Rheumatol. 1994;21:2166-2167. [PubMed] [Cited in This Article: ] |
| 5. | Rankin AC, Osswald S, McGovern BA, Ruskin JN, Garan H. Mechanism of sustained monomorphic ventricular tachycardia in systemic sclerosis. Am J Cardiol. 1999;83:633-636, A11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Camino A, Madrid AH, Rebollo JM, Peña G, Socas AG, Moro C. [Radiofrequency ablation of recurrent monomorphic ventricular tachycardia in a patient with severe systemic scleroderma]. Rev Esp Cardiol. 2001;54:405-408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Lacroix D, Brigadeau F, Marquié C, Klug D. Electroanatomic mapping and ablation of ventricular tachycardia associated with systemic sclerosis. Europace. 2004;6:336-342. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Chung HH, Kim JB, Hong SH, Lee HJ, Joung B, Lee MH. Radiofrequency catheter ablation of hemodynamically unstable ventricular tachycardia associated with systemic sclerosis. J Korean Med Sci. 2012;27:215-217. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Bernardo P, Conforti ML, Bellando-Randone S, Pieragnoli P, Blagojevic J, Kaloudi O, Guiducci S, Porta F, Padeletti L, Gensini GF, Matucci-Cerinic M. Implantable cardioverter defibrillator prevents sudden cardiac death in systemic sclerosis. J Rheumatol. 2011;38:1617-1621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8928] [Cited by in RCA: 9214] [Article Influence: 1023.8] [Reference Citation Analysis (3)] |