Copyright
©The Author(s) 2020.
World J Clin Cases. Feb 26, 2020; 8(4): 848-853
Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.848
Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.848
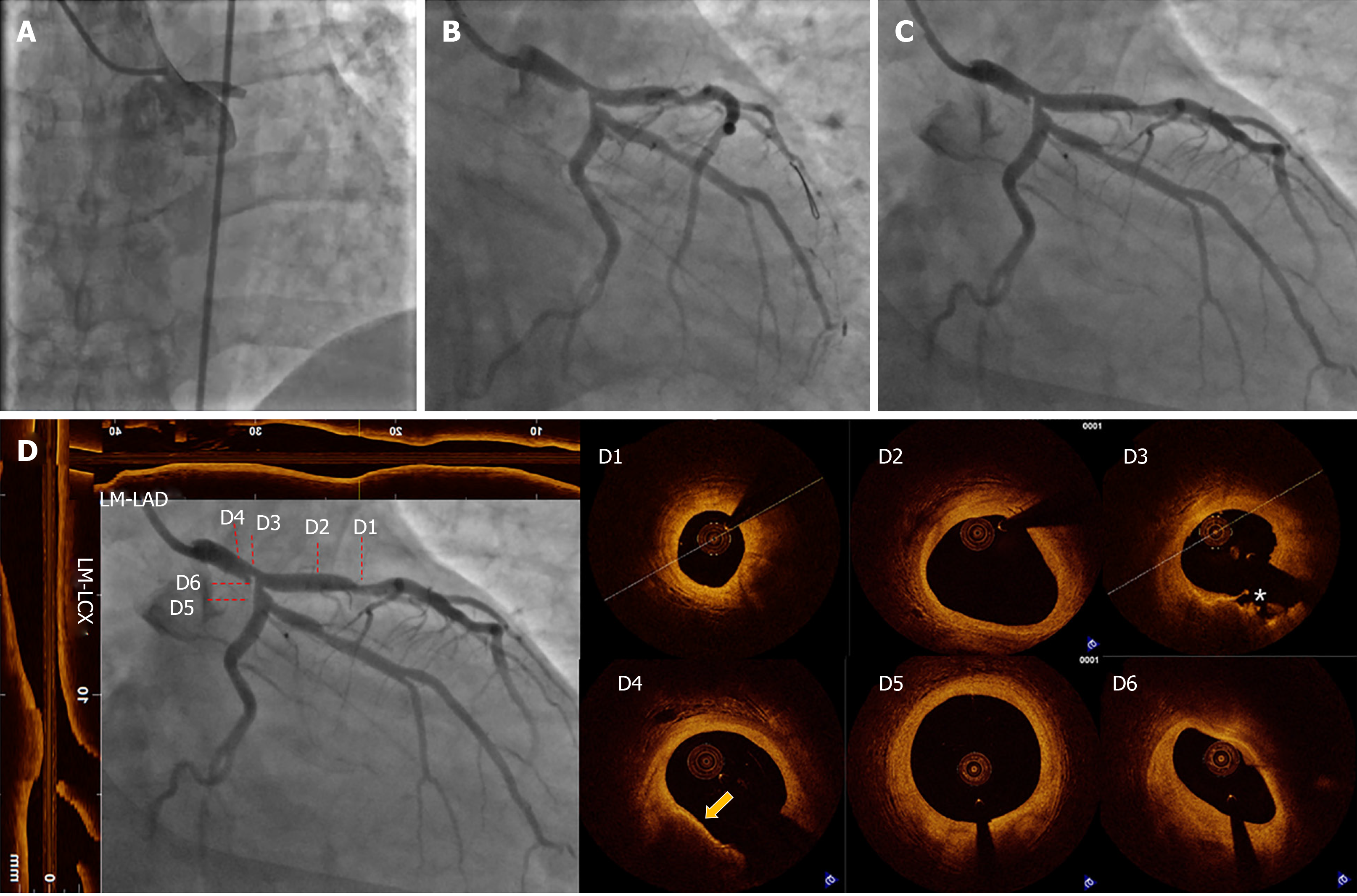
Figure 1 Coronary angiography and optical coherence tomography of the primary intervention and follow-up.
A: Emergency coronary angiography (CAG) showed acute occlusion of the left main (LM) artery; B: CAG after thrombus aspiration. There was severe stenosis in the distal LM and ostium left circumflex artery (LCX). In addition, moderate stenosis in the proximal left anterior descending artery (LAD) was observed; C: CAG one week after acute myocardial infarction was almost identical to the previous result (B); D: CAG, longitudinal and cross-sectional optical coherence tomography images one week after acute myocardial infarction. Longitudinal optical coherence tomography images were adjusted with the direction and position of the CAG. (D1: Moderate stenosis in the proximal LAD, minimal lumen area = 2.91 mm2, stable thick cap plaque; D2: Normal coronary vessel in the proximal LAD; D3: Cross-section of the filling defect. A severe stenosis with plaque rupture (indicated by asterisks), minimal lumen area = 3.19 mm2, MLD = 4.28 mm; D4: Thin fibrous cap atheroma in the LM body (indicated by the yellow arrow); D5: Normal section in the proximal LCX; D6: Ostium of the LCX. One mm proximal of D5, the sharp sectional change between D5 and D6 with no evidence of atheroma indicates it was caused by the carina). CAG: coronary angiography, OCT: optical coherence tomography, LAD: left anterior descending artery, LCX: left circumflex artery, LM: left main.
- Citation: Du BB, Tong YL, Wang XT, Liu GH, Liu K, Yang P, He YQ. Rescue treatment and follow-up intervention of a left main acute myocardial infarction with typical carina shift under 3D optical coherence tomography: A case report. World J Clin Cases 2020; 8(4): 848-853
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/848.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.848