Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3517
Peer-review started: May 23, 2019
First decision: August 1, 2019
Revised: August 23, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 6, 2019
While in children intussusception is often idiopathic, in adults it is commonly caused by a pathologic condition functioning as a lead point. It is important to note that a variety of pathologic conditions may trigger intussusception, with malignancy being a relatively frequent culprit in adults; this should be considered high on the differential diagnosis during evaluation.
This is a case of a 40-year-old female presenting to the emergency department (ED) with three days of acute on chronic, peri-umbilical abdominal pain described as waxing and waning, and pressure-like in nature. Initial computed tomography (CT) of the abdomen and pelvis with contrast in the ED (after her pain had resolved) re-demonstrated a previously noted 13 mm lesion in the gastric antrum but no clear cause of the pain. Endoscopic ultrasound was pursued, and the mass lesion was sampled via fine needle biopsy. Post-procedure the patient experienced another episode of severe pain which prompted a repeat stat CT abdomen and pelvis with contrast; this re-demonstrated the 13 mm antral lesion and in addition was remarkable for a gastro-gastric intussusception. An upper gastrointestinal gastrograffin series was ordered (completed only after the pain had subsided) and showed resolution of the intussusception. Histopathology was consistent with a diagnosis of low-grade neuroendocrine tumor (NET). Surgery was initially deferred during the hospitilization given the low grade pathology of the lesion; however further multidisciplinary discussion between Surgery, Oncology, and Gastroenterology recommended resection given the patient’s recurrent abdominal pain with the NET functioning as a lead point for further intussusception, and the patient thus underwent robotically-assisted wedge resection.
We present a unique case of severe, intermittent, peri-umbilical pain related to gastro-gastric intussusception caused by an antral NET lead point. The case highlights the importance of considering neoplasms as the cause of intussusception in adults and the greater diagnostic yield when imaging is obtained while symptoms (in this case severe, episodic abdominal pain) are most apparent.
Core tip: Intussusception in adults is an important etiology to consider in patients with acute abdominal pain; the cause may be a neoplasm, which can function as a lead point, and timely imaging is a vital part of the diagnostic evaluation. This case report describes a 40 years-old female with multiple emergency department visits for acute abdominal pain with and what was initially thought to be an incidental 13 mm gastric antral mass. The patient was ultimately diagnosed with gastric-gastric intussusception and a gastric neuroendocrine tumor as a lead point.
- Citation: Zhornitskiy A, Le L, Tareen S, Abdullahi G, Karunasiri D, Tabibian JH. Gastro-gastric intussusception in the setting of a neuroendocrine tumor: A case report. World J Clin Cases 2019; 7(21): 3517-3523
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3517.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3517
The clinical presentation of intussusception includes symptoms of abdominal pain and/or bowel obstruction due to telescoping of a portion of a bowel segment into the lumen of another. It is most frequently seen in children, where it is commonly idiopathic; in adults, intussusception is predominantly secondary to a pathologic condition acting as a lead point (e.g., a stricture due to inflammatory bowel disease, large polyp, or hamartoma), with more than half of cases being caused by an underlying malignancy.
A 40-year-old female presenting to the emergency department (ED) with three days of severe, pressure-like, peri-umbilical abdominal pain.
The patient’s abdominal pain was waxing and waning in nature, exacerbated by food and associated with nausea and occasional diarrhea. The patient denied melena, hematochezia, change in stool caliber, weight loss, early satiety, flushing, fevers or chills. She had experienced multiple episodes of pain over the past six months resulting in two ED visits. On the most recent episode one month prior, she presented with similar abdominal pain, at which time computed tomography (CT) of the abdomen and pelvis with contrast showed a 13 mm mass in the gastric antrum. The antral lesion, however, appeared too small to be causing the patient’s pain, and given spontaneous resolution of her pain, she was discharged.
Notable for well controlled rheumatoid arthritis and cholecystectomy five years ago.
Family history includes gastric cancer in her father that was diagnosed at 61 years old.
Vital signs on presentation were notable for tachycardia to 101 beats per minute and hypertension of 159/105 mm Hg. Physical examination revealed a non-distended, soft, abdomen with diffuse tenderness to minimal palpation, without rebound tenderness.
Laboratory studies, including complete blood count, serum electrolytes, lactate, and gastrin levels, were within normal limits.
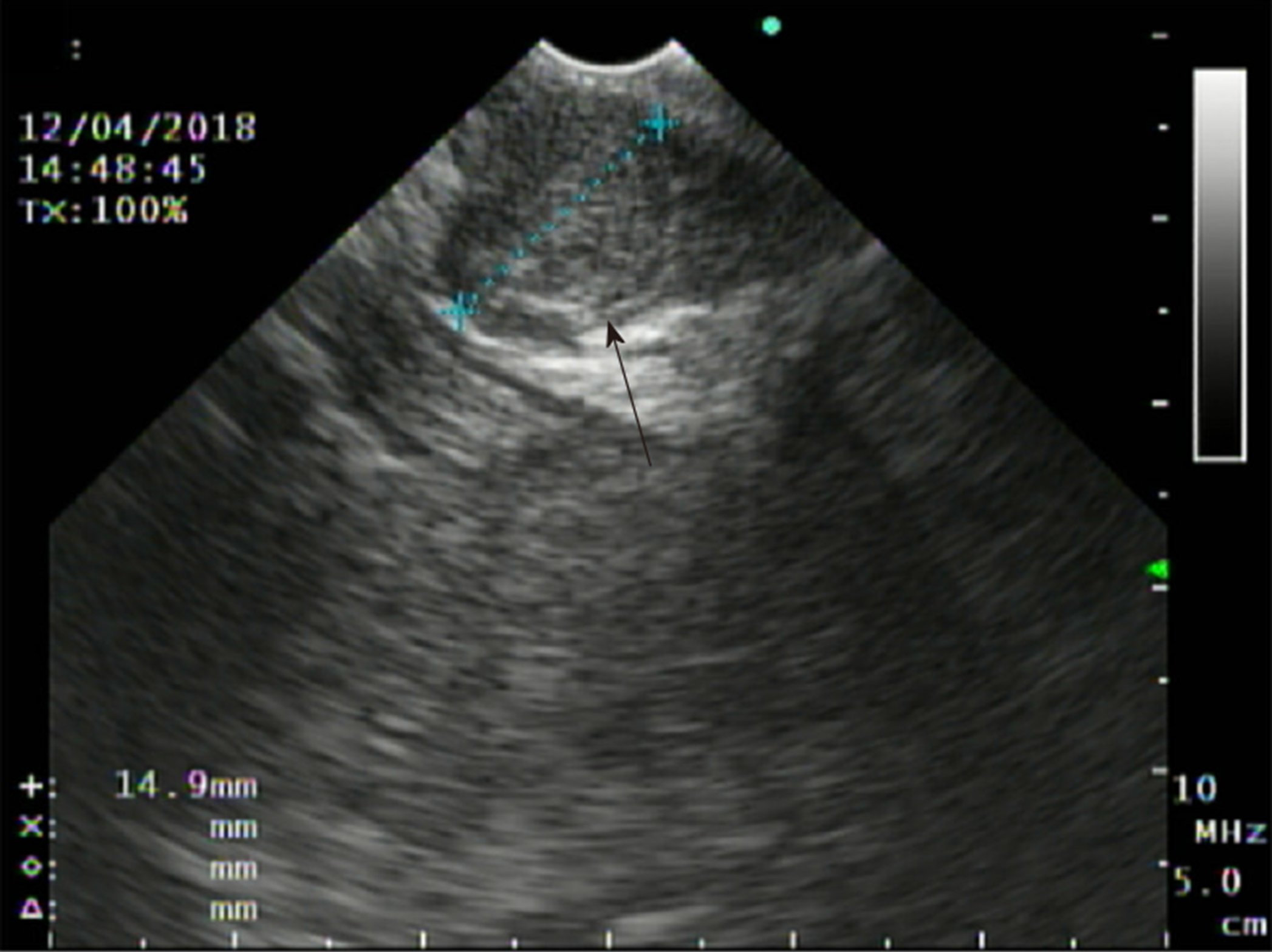
In the ED, initial CT abdomen and pelvis with contrast was ordered but not completed until after resolution of the patient’s abdominal pain. It re-demonstrated a 13 mm mass in the gastric antrum seen on CT during her last presentation to the ED one month prior but was otherwise unremarkable. An endoscopic ultrasound was recommended to further investigate the antral lesion; a 13 mm subepithelial, hypoechoic lesion was seen in the antrum, and fine needle biopsy (FNB) was performed (Figure 1). Several hours after the procedure, the patient again had an episode of the same abdominal pain she had been experiencing; this prompted a stat CT of the abdomen with contrast that showed a gastro-gastric intussusception (Figures 2 and 3) without any evidence of bleeding or other FNB-related adverse events. The pain again subsided with supportive measures.
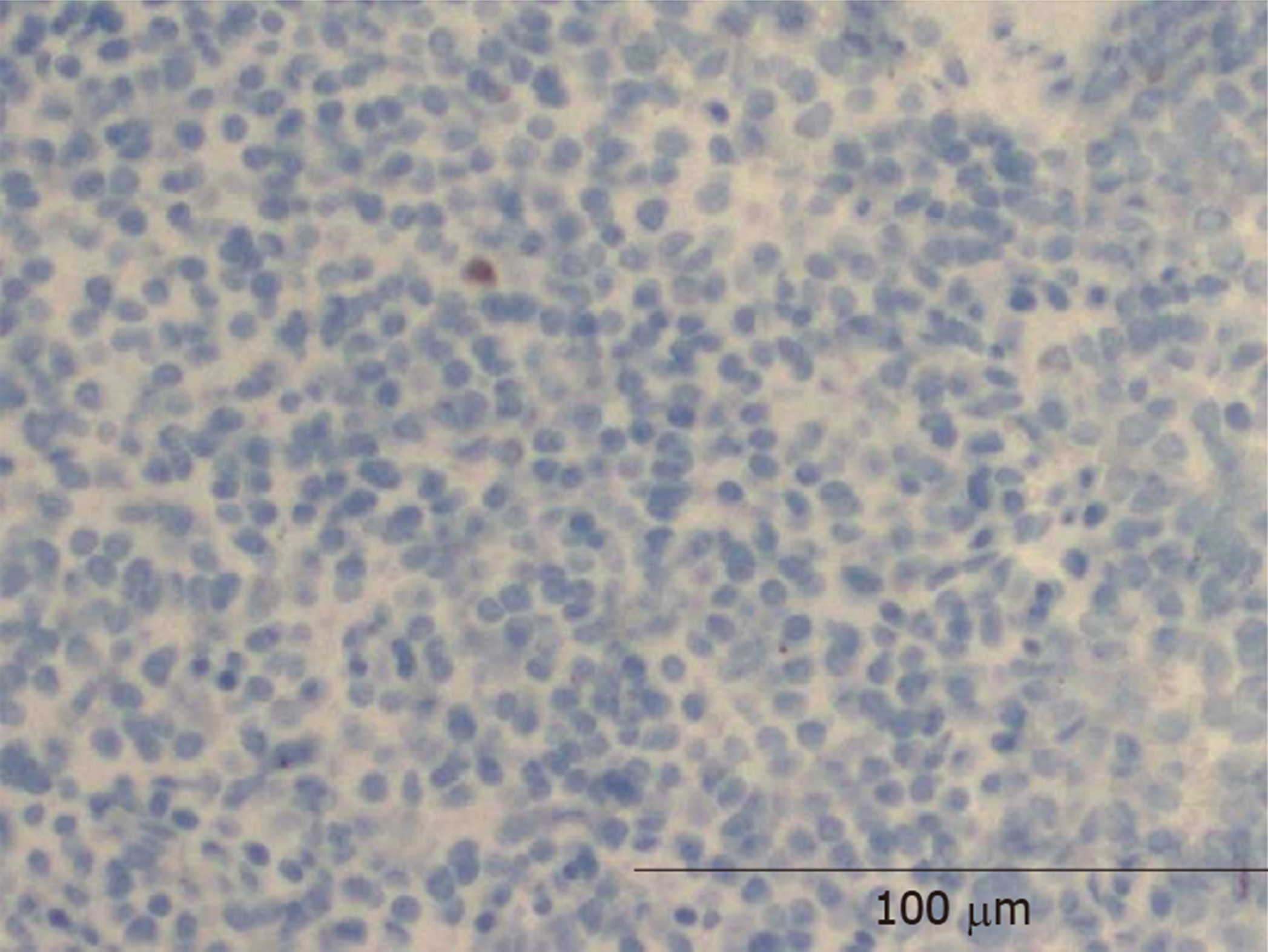
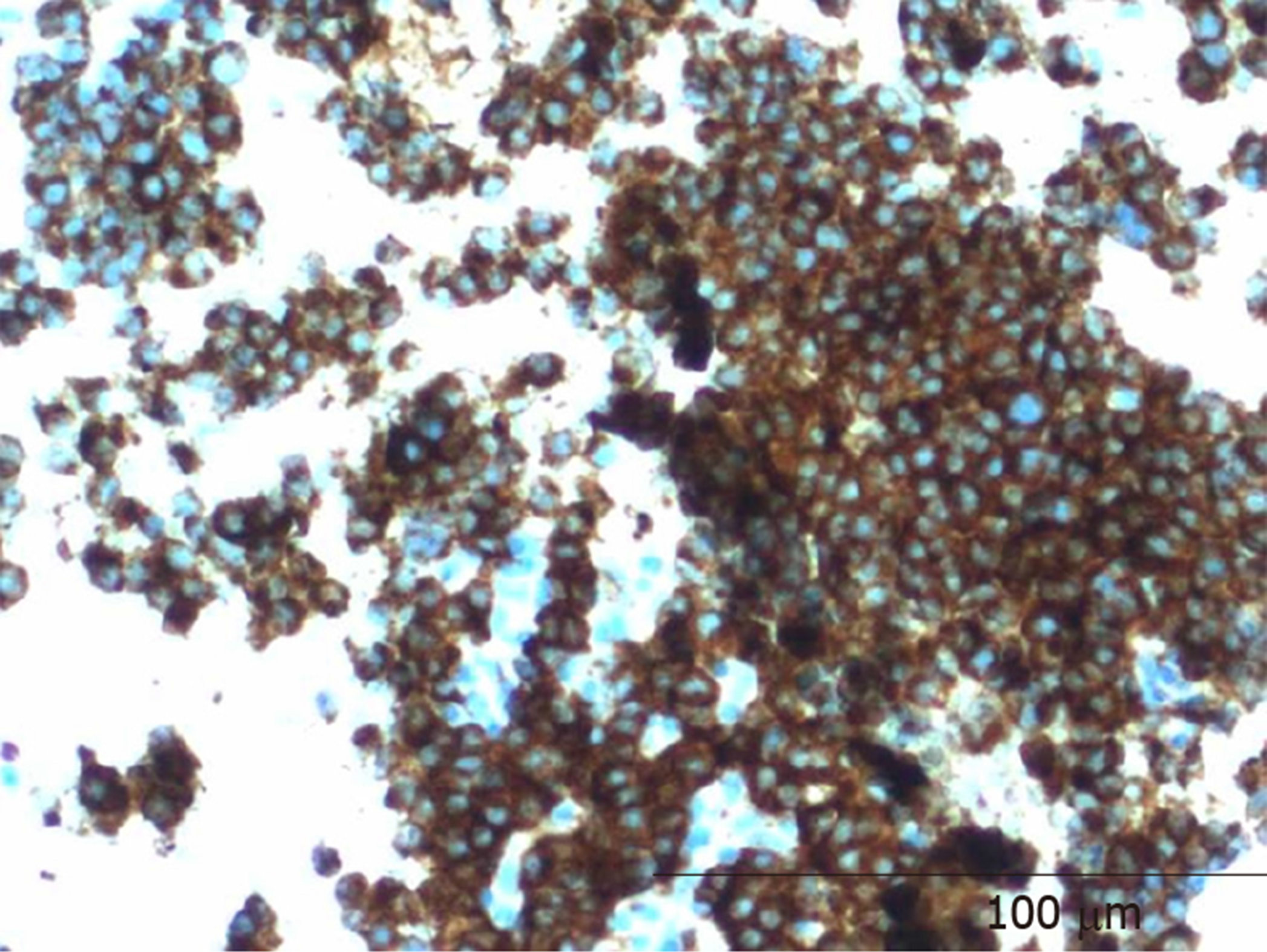
Histopathology was notable for a low mitotic rate, with Ki67 index < 1%, and staining positive for synaptophysin and chromogranin, suggestive of a grade 1 neuroendocrine tumor (NET) (Figures 4 and 5).
Gastro-gastric intussusception secondary to a gastric NET functioning as a lead point.
General surgery was consulted for management of the intussusception and recommended an upper gastrointestinal gastrograffin series for further visualization. The study was completed after resolution of the patient’s abdominal pain and demonstrated resolution of the intussusception. Given the location of the tumor, its low-grade nature based on Ki67 and mitotic count, as well as the resolution of symptoms, a multidisciplinary decision was made to defer any surgical interventions during the hospitalization and instead continue further workup as an outpatient with close Oncology, Gastroenterology, and Surgery follow-up.
A follow-up nuclear medicine octreotide whole body scan was performed showing an intense focus of uptake at the antrum corresponding to the known mass with no other areas of uptake that would be suggestive of signs of metastasis. The patient continued to note episodes of severe abdominal pain during outpatient clinic visits and repeat multidisciplinary discussion between Surgical Oncology and Gastroenterology resulted in the decision to proceed with surgical resection and she is now status post robot-assisted partial gastrectomy and doing clinically well. While it was acknowledged that the risk of metastasis is low given the histopathology, the tumor’s continued presence appeared to be the underlying cause of her recurrent abdominal pain as it remained a lead point for repeat intussusception, hence warranting surgical resection.
This case highlights what is most frequently seen in adults as the cause of intussusception: a pathologic condition functioning as lead point. However, there are multiple interesting aspects of this case that have not previously been described in published literature, including the tumor location and underlying NET as a lead point.
The nomenclature for neuroendocrine masses is confusing with the acronyms neuroendocrine neoplasms (NEN), NET, and neuroendocrine carcinomas (NEC) often used interchangeably. According to the World Health Organization (WHO), the overarching term is NEN with NETs referring to masses that show more benign characteristics while NECs are more aggressive and have malignant features[1]. Simply put, NENs are a heterogenous group of tumors that can be found throughout the body and are characterized by their endocrine functions, which are monoamines synthesis and secretion. These neoplasms are quite rare and account for only 0.5% of all newly diagnosed malignancies. The most frequent primary sites are the gastrointestinal tract (62%) and the lung (22%)[2]. Histologically, NETs are well-differentiated and identified by intense immuno-expression of neuroendocrine markers such as synaptophysin and chromogranin A, whereas similarly named NECs are poorly differentiated, have decreased expression of neuroendocrine markers, and higher mitotic rates. Per 2010 WHO guidelines, NENs found in the gastrointestinal tract are classified based on their mitotic count and Ki67 proliferation[1].
The most common locations for intussusception are small bowel only (entero-enteric), large bowel only (colo-colonic), or small bowel into large bowel (termed ileo-colic or ileo-cecal if the ileocecal valve is determined to be the lead point)[2]. The frequency of the intussusception at certain sites was evaluated in a study of 745 adults and showed that 52% were found in the small intestine and 38% in the large intestine (17% ileocecal, 17% colocolic, 4% appendiceal)[3]. However, intussusception involving the proximal gastrointestinal tract such as the stomach is exceedingly rare. A recent literature review identified only 10 instances of gastro-gastric intussusception since 1950, all of which were associated with a mass, either benign or malignant, functioning as a lead point[4-13] (Table 1).
| Ref. | Age/sex | Presentation | Histological findings | Intussusception diagnostic modality |
| Grundy et al[4] | 78 F and 76 F | Dysphagia, weight loss, epigastric pain, vomiting | Leiomyoma | Fluoroscopy |
| Thomson et al[5] | 72 M | Epigastric pain, nausea, vomiting | Pedunculated intragastric tumour | Laparotomy |
| Javors et al[6] | 81 F | Anemia | Leiomyoma with leiomyoblastomatous elements | Single contrast UGI series |
| Raw[7] | 66 F | Epigastric discomfort, vomiting | Malignant gastric papilloma | Laparotomy |
| Shanbhogue et al[8] | 83 F | Melena, anemia, weight loss | Gastrointestinal stromal tumour | CT abdomen |
| Vikram et al[9] | 65 F | Epigastric pain, nausea, vomiting, epigastric mass | Hypertrophic gastric polyps | Double contrast barium meal, CT abdomen |
| Davila et al[10] | 77 F | Fever, abdominal discomfort, left lateral abdominal mass | Tubulo-villous adenoma | MR abdomen |
| Eom et al[11] | 73 F | Vomiting, general weakness | Gastric adenocarcinoma | CT abdomen |
| Jo et al[12] | 82 F | Chest pain and vomiting | Primary gastric lymphoma | CT abdomen |
The underlying etiology of intussusception is essential to consider, as it determines management. As alluded to before, in children the most common etiology of intussusception is overwhelmingly idiopathic, whereas in adults, more than half of the cases are due to an underlying malignancy, with adenocarcinoma being the most likely culprit[14]. Therefore, if initial biopsies are negative for malignancy, clinicians should maintain a high index of suspicion and have a low threshold for repeat biopsy such as in this case. A NET leading to intussusception is exceedingly rare, with only a few case reports described in the available literature[15]. Furthermore, none of these aforementioned cases involved the stomach or resulted in gastro-gastric intussusception as observed in our case.
In the absence of an underlying systemic disorder (e.g., Celiac disease, lymphoma), the mainstay of management of intussusception is typically definitive treatment with surgical resection[16,17]. This case would similarly require surgical intervention for definitive treatment since the NET continues to put the patient at risk for recurrent episodes of intussusception.
This case describes a previously unreported presentation of severe, episodic, peri-umbilical pain due to gastro-gastric intussusception caused by a gastric NET.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A, A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Caboclo JF, Imaeda H, Isik A, Dang SS S-Editor: Yan JP L-Editor: A E-Editor: Liu JH
| 1. | Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia. 2017;19:991-1002. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 405] [Cited by in F6Publishing: 392] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 2. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 428] [Cited by in F6Publishing: 452] [Article Influence: 30.1] [Reference Citation Analysis (1)] |
| 3. | Brayton D, Norris WJ. Intussusception in adults. Am J Surg. 1954;88:32-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 133] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Grundy A, Rayter Z, Shorthouse AJ. Gastrogastric intussuscepting leiomyomas. Gastrointest Radiol. 1984;9:319-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Thomson A. Gastro-gastric Intussusception Produced by Pedunculated Intragastric Tumour. Br Med J. 1950;1:525-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Javors BR, Rackson M. Gastrogastric intussusception. J Clin Gastroenterol. 1987;9:113-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Raw SC. Gastro-gastric Intussusception. Br Med J. 1950;1:905. [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Shanbhogue A, Walsh C, Fasih N. Education and imaging. Gastrointestinal: gastrogastric intussusception. J Gastroenterol Hepatol. 2009;24:169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Vikram R, McCulloch AS, Zealley IA. True gastrogastric intussusception: a rare radiologic diagnosis with surgical correlation. AJR Am J Roentgenol. 2006;186:585-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Dávila Arias C, Milena Muñoz A, Valero González MÁ, Céspedes Mas M. Gastric invagination in adults as a rare cause of constitutional syndrome. Rev Esp Enferm Dig. 2017;109:146-147. [PubMed] [Cited in This Article: ] |
| 11. | Eom BW, Ryu KW, Lee JH, Lee JY, Lee JS, Kook MC, Kim YW. Gastrogastric intussusception secondary to a gastric carcinoma: Report of a case. Surg Today. 2011;41:1424-1427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Jo HH, Kang SM, Kim SH, Ra M, Park BK, Kwon JG, Kim EY, Jung JT, Kim HG, Ryoo HM, Kang UR. [A Case of Gastro-Gastric Intussusception Secondary to Primary Gastric Lymphoma]. Korean J Gastroenterol. 2016;68:40-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Behrooz A, Cleasby M. Gastrogastric intussusception in adults: a case report with review of the literature. BJR. 2018;4:4. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Lu T, Chng YM. Adult Intussusception. Perm J. 2015;19:79-81. [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Thomas RE, Maude K, Rotimi O. A case of an intussuscepted neuroendocrine carcinoma of the appendix. World J Gastroenterol. 2006;12:971-973. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg. 2003;186:75-76. [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Onkendi EO, Grotz TE, Murray JA, Donohue JH. Adult intussusception in the last 25 years of modern imaging: is surgery still indicated? J Gastrointest Surg. 2011;15:1699-1705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |