Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2427
Peer-review started: March 28, 2019
First decision: August 1, 2019
Revised: August 15, 2019
Accepted: August 25, 2019
Article in press: August 26, 2019
Published online: September 6, 2019
Reduced level of physical activity, high-fat diet and skeletal muscle atrophy are key factors that are likely to contribute to deleterious changes in body composition and metabolic following spinal cord injury (SCI). Reduced caloric intake with lowering percentage macronutrients of fat and increasing protein intake may likely to improve body composition parameters and decrease ectopic adiposity after SCI.
To highlight the effects of dietary manipulation and testosterone replacement therapy (TRT) on body composition after SCI
A 31-year-old male with T5 SCI was administered transdermal TRT daily for 16 wk. Caloric intake and percentage macronutrients were analyzed using dietary recalls. Magnetic resonance imaging and dual-energy x-ray absorptiometry were used to measure changes in body composition.
Caloric intake and fat percentage were reduced by 445 kcal/d and 6.5%, respectively. Total body weight decreased by 8%, body fat decreased by 29%, and lean mass increased by 7%. Thigh subcutaneous adipose tissue cross-sectional area was reduced by 31%.
Manipulation of caloric intake, fat percentage, and protein percentage may have influenced body composition after SCI.
Core tip: Reduction in caloric intake with low-fat and high-protein diet may appear as a reasonable strategy to effectively lose weight and fat mass in persons with spinal cord injury. The supplement of testosterone replacement therapy (TRT) may offset for potential loss in lean mass and reduction in basal metabolic rate that is commonly observed in weight loss program. The combination of dietary manipulation and TRT is a feasible approach and does not appear to be accompanied with any side effects.
- Citation: Gorgey AS, Lester RM, Ghatas MP, Sistrun SN, Lavis T. Dietary manipulation and testosterone replacement therapy may explain changes in body composition after spinal cord injury: A retrospective case report. World J Clin Cases 2019; 7(17): 2427-2437
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2427.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2427
Individuals with spinal cord injury (SCI) are at heightened risk for developing obesity because of loss in lean mass, reduced basal metabolic rate (BMR) and decreased level of physical activity[1-3]. Prevalence of obesity is primarily attributed to disruption in energy balance following SCI. Disruption in energy balance is a function of decreased BMR and often leads to increased accumulation of total, regional fat and visceral adipose tissue (VAT)[4-6]. Reduction in leisure time physical activity, reliance primarily on wheelchairs for mobility, and poor dietary habits are major factors that contribute to the prevalence of obesity after SCI[7]. Therefore, providing an effective exercise regimen or dietary management plan may protect against disruptions in energy homeostasis. Moreover, it may reduce the heightened risk for developing secondary complications similar to glucose intolerance, insulin resistance, hyperlipidemia, and cardiovascular disease after SCI[2-5,7].
Persons with SCI often consume a high-fat diet of 35%-40% fat, well above the recommended level of 30% which is typical of the standard American diet[7-9]. Poor dietary habits were attributed to a lack of knowledge surrounding nutrition, solitary living, smoking, and socioeconomic status following SCI[9]. Moreover, studies involving human and animal models revealed associations between high fat consumption and increased VAT, serum leptin levels, pro-inflammatory cytokines, and insulin resistance[3,10]. To circumvent the aforementioned profile, implementation of a Mediterranean-style diet resulted in a 7% reduction in total body weight in three males with SCI[10]. These results are promising, however, a full account of the changes in total or regional lean and fat masses were not provided. Regional changes in body composition have been considered a major determinant of cardiometabolic profile in persons with SCI[2,3]. Furthermore, it is well established that loss in body weight has been accompanied with a reduction in lean mass in elderly individuals[11]; therefore, accounting for the changes in lean mass is highly important with dietary manipulation in men with SCI. Maintenance of lean mass may protect against further reduction in BMR and further increase in the prevalence of obesity after SCI.
Different rehabilitation approaches have been recommended for maintenance of lean mass including exercise, electrical stimulation and testosterone replacement therapy (TRT). Transdermal TRT has been administered in hypogonadal persons with SCI with testosterone level less than 325 ng/dL. A previous work showed that 43.3% of men with SCI had serum testosterone levels < 325 ng/dL[12]. Reduced circulating testosterone level may be a contributing factor to the loss in lean mass after SCI[13,14]. Furthermore, circulating serum testosterone is negatively linked with total and regional body fatness, VAT and positively linked to lean mass and thigh muscle cross-sectional area (CSA)[14]. A 1-year small scale clinical trial demonstrated the efficacy of TRT in restoring total and regional lean mass as well as increasing BMR in hypogonadal men with SCI[15]. A recent randomized clinical trial showed that 16 wk of TRT accompanied with surface neuromuscular electrical stimulation-resistance training (TRT+RT) resulted in 43% increase in muscle CSA, 2.7 kg increase in total body lean mass and a trend of 14%-17% increase in basal metabolic rate compare to TRT only in men with SCI[16].
Therefore, dietary manipulation with TRT may serve as a potential rehabilitation approach to reduce body fatness, maintain lean mass and BMR in persons with SCI. We, retrospectively, tracked the dietary habits of individual and eight additional participants for the purpose of comparing caloric and macronutrient intakes during participating in a 16 wk clinical trial. The current case report highlighted the significance of reducing caloric intake and manipulating macronutrients with TRT on the changes in total and regional body composition in a male with SCI.
The physical characteristics and demographics of one male participant as well as a comparative cohort of eight men are presented in Table 1. Each participant received a daily testosterone dose (2-6 mg/d) via transdermal patch (Androderm; Watson Laboratories, Inc, Corona, Canada) placed on the shoulders and alternated daily for 16 wk[16]. The initial TRT dose was determined based on the circulating level of serum testosterone and then adjusted according to participant’s response in a blinded fashion. A 4 mg/d of TRT was administered on a daily basis for our participant. Data from one participant of the original cohort (n = 8) was excluded due to frequent missing data points and non-compliance with dietary records. Each participant signed an informed consent prior to enrollment in the clinical trial and all study procedures were approved by the local ethics committee.
| Characteristics | Case Participant | Cohort | Total |
| (n = 1) | (n = 8) | (n = 9) | |
| Age (yr) | 31 | 36 ± 9 | 36 ± 8 |
| Sex | Male (n = 1) | Male (n = 8) | Male (n = 9) |
| Ethnicity | Caucasian (n = 1) | African American | African American |
| (n = 3) | (n = 3) | ||
| Caucasian (n = 5) | Caucasian (n = 6) | ||
| Weight (kg) | 77 | 77 ± 11 | 77 ± 10 |
| Height (m) | 1.8 | 1.8 ± 5 | 1.8 ± 5 |
| BMI (kg/m2) | 24.8 | 24 ± 4 | 24 ± 4 |
| Level of injury | T5-T6 | C6-T11 | C6-T11 |
| Time since injury (yr) | 7 | 7 ± 7 | 7 ± 7 |
| AIS classification | A | A (n = 5) | A (n = 6) |
| B (n = 3) | B (n = 3) | ||
| Level of Paralysis | Paraplegia | Paraplegia (n = 3) | Paraplegia (n = 4) |
| Tetraplegia (n = 5) | Tetraplegia (n = 5) |
Prior to enrollment in the 16 wk clinical trial, each participant completed 4 wk, a pre-trial-phase, as a control period to stabilize body weight and to record their standard dietary habits. At the beginning of this phase, body composition assessment was completed using dual energy x-ray absorptiometry (DXA) and participants did not receive any feedback to adjust or manipulate their dietary habits[16].
At the beginning of the 16 wk intervention, a registered dietitian encouraged compliance to a standard daily diet plan (45% carbohydrate, 30% fat, and 25% protein). Caloric allowances were estimated based on each participant’s BMR[7].
Each participant completed weekly 5 d dietary recalls and monthly feedback from the dietician was provided, via phone interview or emails[7]. Dietary records were evaluated using Nutrition Data System for Research (NDSR; 2016 Regents of the University of Minnesota). The following dietary variables were quantified: Total caloric intake (kcal), percentage calories from carbohydrates, percentage calories from fats, percentage calories from proteins, and total soluble fiber. Retrospective analysis revealed that the dietary habits of the case report began to change at the end of week 8. Therefore, dietary data were split into phase I (weeks 1-8) and phase II (weeks 9-16). Splitting the data allowed for the comparison in caloric intake and percentage macronutrients between phase I when the participant closely followed the recommended dietary habits and phase II, when the case report deviated from the recommended caloric intake and macronutrients. The differences in percentages carbohydrate, fat, and protein intakes were calculated between phases I and II. Data from the case report was also compared to the average consumption of the cohort to demonstrate the deviation in the dietary habits in phase II of the study.
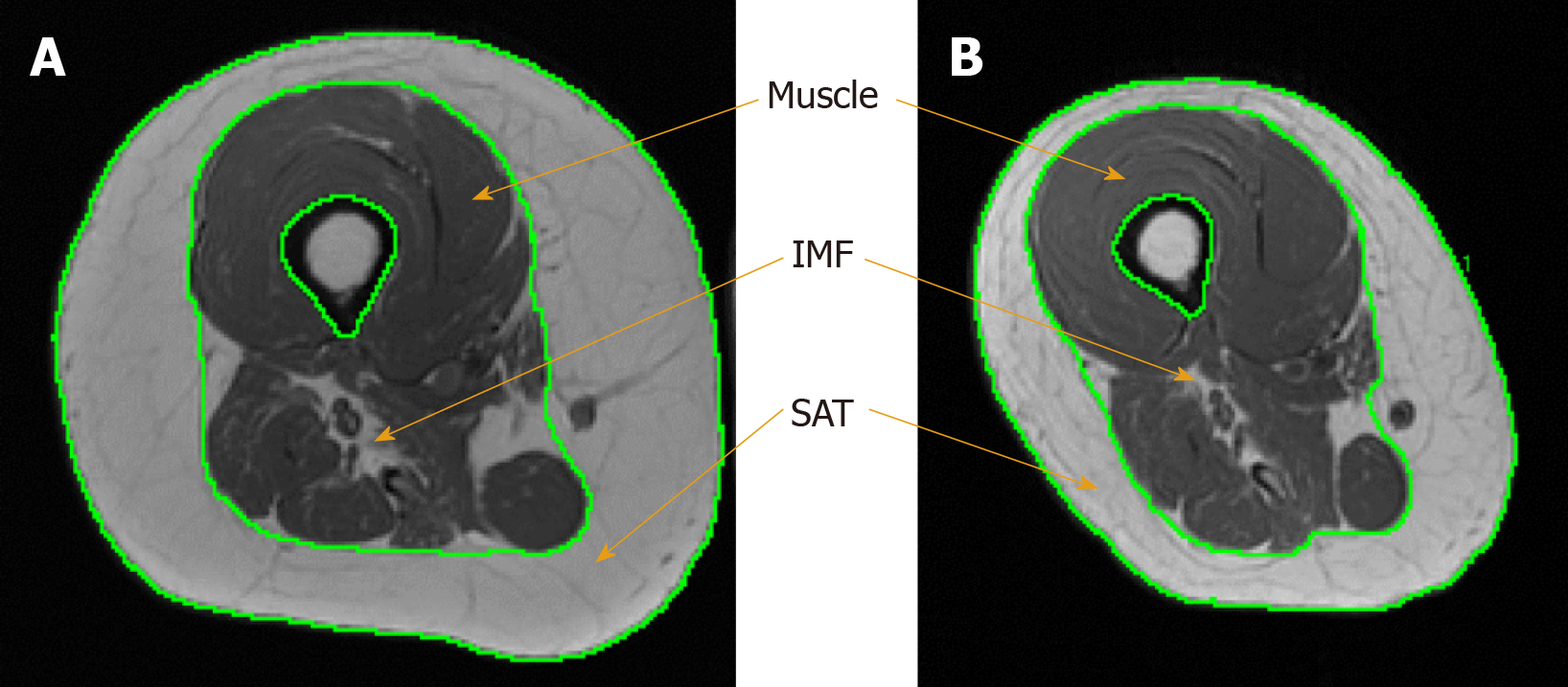
T1-weighted MRIs were obtained from a total body General Electric Signa 1.5-T MRI located within the McGuire VAMC Radiology Department at baseline and post-intervention. 12 to 15 trans-axial images (slice thickness, 0.8 cm; interslice space, 1.6 cm) were captured from hip to knee joints of the right thigh to quantify muscle and fat CSAs[17]. Four regions of interest were manually isolated using X-Vessel (Version 2.011; Michigan State University, Lansing, United States) including thigh subcutaneous adipose tissue (SAT) CSA, whole muscle CSA, absolute muscle CSA, and absolute intramuscular fat (IMF) CSA (Figure 1), as well as trunk VAT and SAT. Whole muscle CSA refers to the total muscle area of the thigh including IMF and excluding tissues of the femoral bone. Absolute muscle CSA refers to thigh muscle after accounting for IMF. IMF refers to the fat infiltrated within and between muscle fibers and is presented as an absolute value and percentage relative to the whole thigh muscle CSA[17]. To calculate CSA, the sum of pixels within a region of interest was multiplied by (FOV/matrix size)[2].
For trunk VAT and SAT, participant was positioned in a lying position on the scanning table, transverse axial images (axial in-phase/out-phase with a repetition time of 140 ms and echo time of 4.2 and 2 ms for the in-phase and the out-phase, respectively; a 42 cm field of view; matrix size of 256 × 256; 1 number of excitation; acquisition time of 40 s and slice thickness was 0.8 cm and interslice space was 0.4 cm) were obtained from the xiphoid process to L4-L5 and from L4-L5 to the femoral heads[3,14,16].
DXA scans were performed using a Lunar DXA (GE Healthcare, Chicago, IL) bone densitometer at the Richmond Virginia Medical Center at pre-trial phase, BL and PI. The clinical DXA procedures and estimates of precision were previously published[18]. Total body DXA scans were captured to assess total body weight, lean mass, and fat mass. Scans were performed for 5-10 min and analyzed by a DXA trained researcher using Lunar enCORE software Version 10 (GE Healthcare, Chicago, IL).
After an overnight fast of 10-12 h, participants were kept in a dark room for 20-30 min to attain a resting state during which BMR was measured using a canopy that was attached to a vacuum to draw expired gases to the flowmeter of the metabolic unit (COSMED KB42, manufacturer) as previously described[7,19].
The current case report is a retrospective analysis to a participant that was enrolled in our concluded clinical trial in the TRT only group[16]. For the entire 16 wk, the participant was administered 4 mg/d of TRT. His baseline testosterone level was 440 ng/dL, and increased in weeks 4, 8 and 12 to 625 ng/dL, 753 ng/dL and 613 ng/dL, respectively. At post-intervention measurement, testosterone level without using the patches dropped to 124 ng/dL.
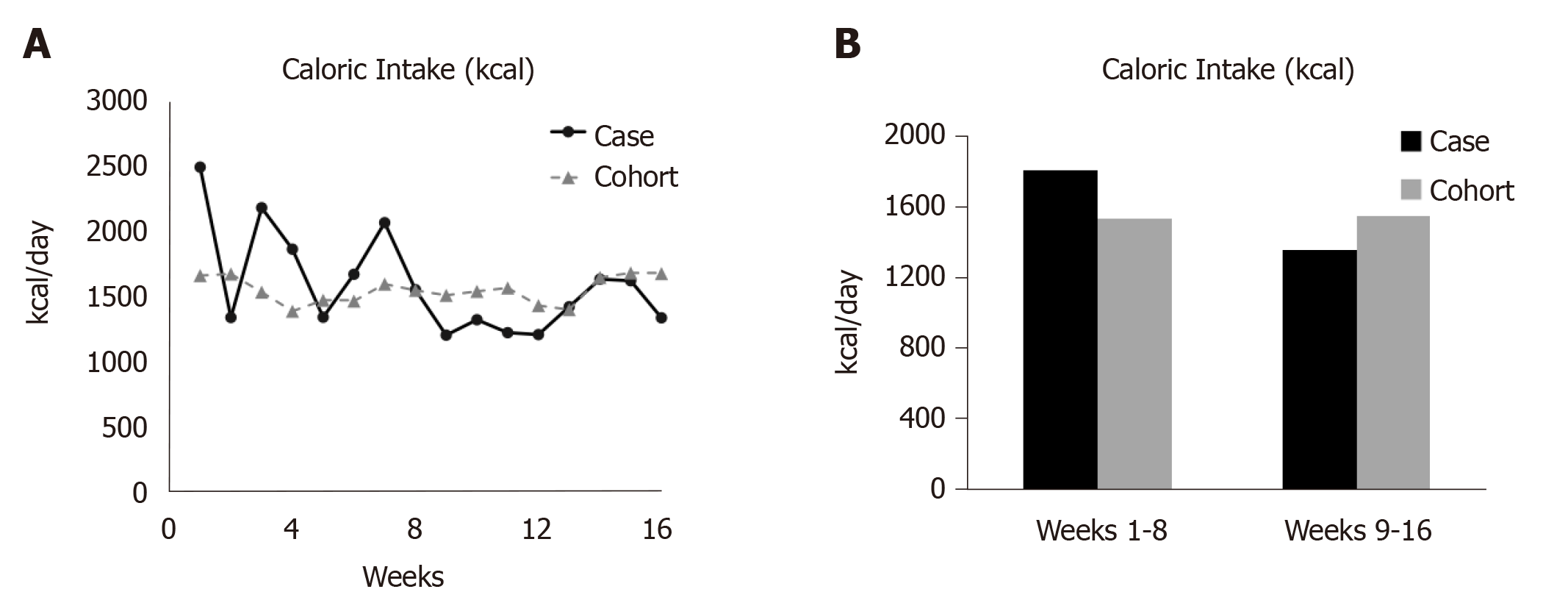
The trends for total caloric intake, percentages carbohydrate, fat, protein, and soluble fiber intake are presented in Figure 2 and Figure 3. Table 2 presents data for each dietary variable and percentages difference between the participant and the study cohort. The case report reduced total caloric intake by 25% (445 kcal/d) and consumed 12% fewer calories than his cohort during phase II (Table 2, Figure 2).
| Energy (kcal) | |||
| Case | Cohort | %difference | |
| Pre-trial | 1935 | ||
| Phase I | 1801.8 | 1528.9 ± 538 | 18% |
| Phase II | 1357.2 | 1543.2 ± 544 | - 12% |
| %difference | - 25% | 1% | |
| Calories from protein (%) | |||
| Case | Cohort | %difference | |
| Pre-trial | 19.0 | ||
| Phase I | 20.6 | 20.80 ± 5.9 | - 0.22% |
| Phase II | 28.2 | 20.25 ± 5.9 | 7.98% |
| %difference | 7.66 | - 0.54 | |
| Calories from carbohydrate (%) | |||
| Case | Cohort | %difference | |
| Pre-trial | 39.0 | ||
| Phase I | 41.1 | 41.4 ± 7.6 | - 0.30% |
| Phase II | 39.9 | 41.6 ± 10 | - 1.70% |
| %difference | - 1.17 | 0.23 | |
| Calories from fat (%) | |||
| Case | Cohort | %difference | |
| Pre-trial | 40.8 | ||
| Phase I | 36.8 | 36.0 ± 6.7 | 0.75% |
| Phase II | 30.3 | 36.7 ± 5.7 | - 6.45% |
| %difference | - 6.50 | 0.71 | |
| Soluble dietary fiber (g) | |||
| Case | Cohort | %difference | |
| Pre-trial | 6.56 | ||
| Phase I | 6.55 | 4.19 ± 1.6 | 56% |
| Phase II | 6.67 | 3.89 ± 2.1 | 71.5% |
| %difference | 2% | - 7% | |
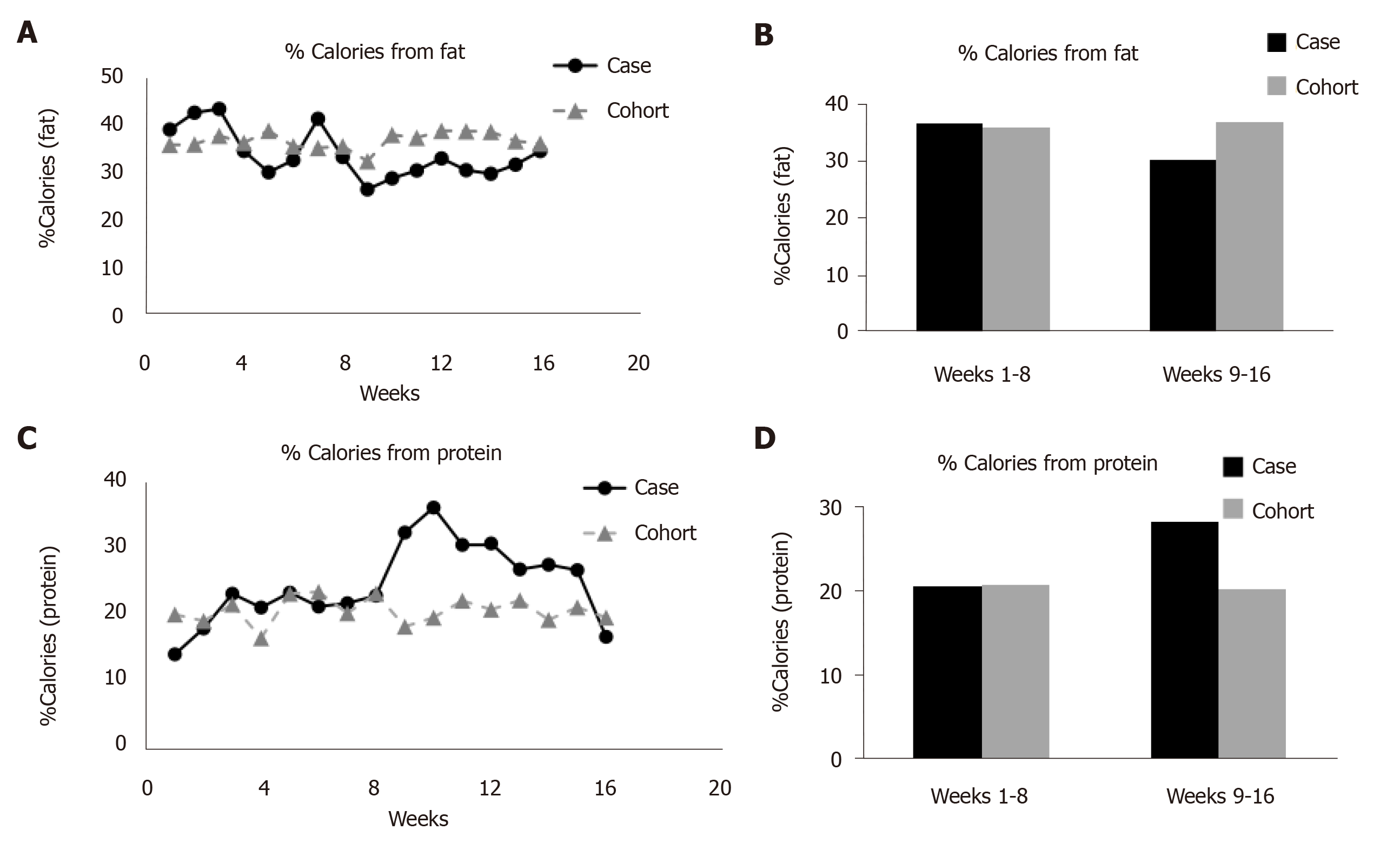
The participant and cohort both consumed 41% of their calories as carbohydrates (Table 2). The percentage carbohydrates consumed by the case report or the cohort did not change over the course of 16 wk. The case report reduced his fat intake by 7% over the course of intervention, with almost no change in fat intake (< 1%) observed by the cohort (Table 2, Figure 3). During phase I, the participant consumed roughly the same proportion of calories from fat as his cohort (case: 37%; cohort: 36%); however, during phase II, the participant consumed 6% less calories from fat.
For the case report, percentage calories from protein increased by 7.6% in phase II compared to phase I of the trial (Table 2, Figure 3). Compared to the study cohort, the case report consumed 8% more calories from protein during phase II of the trial.
Finally, soluble fiber intake remained relatively consistent in both case report and the study cohort; however, the case report consumed more than twice the amount of soluble fiber throughout the 16 wk trial (Table 2). During the first and second phases of the trial, the participant consumed roughly 60% and 70% more soluble fiber than the study cohort, respectively. Moreover, the case report increased his soluble fiber intake by 2% during phase II, while the cohort consumed 7% less soluble fiber compared to the initial phase of the trial.
Body composition assessments for the case report acquired at baseline and post-intervention are presented in Table 3. The participant reduced his total body weight by 6.4 kg (8%). Additionally, he lost 8.8 kg (29%) of body fat and gained 3.1 kg (7%) of lean mass. Moreover, the participant’s thigh SAT and absolute IMF CSAs decreased by 31 and 39%, respectively. Conversely, the participant’s whole muscle and absolute muscle CSAs increased by 4% and 9%, respectively. Figure 1 illustrates the robust changes in SAT, IMF and muscle size between baseline and post-intervention measurements. Trunk VAT and SAT CSA decreased by 12% and 22% following 16 wk.
| Body Composition | Pre-trial | BL | P1 | % Change |
| DXA-Fat (kg) | 30.6 | 30.20 | 21.41 | -29 |
| DXA-Lean (kg) | 44.4 | 43.27 | 46.39 | 7.2 |
| DXA-Body Weight (kg) | 77.9 | 76.70 | 70.30 | -8.3 |
| MRI-SAT (cm2) | - | 92.25 | 64.12 | -31 |
| MRI-W.M. (cm2) | - | 69.73 | 72.13 | 3.5 |
| MRI-ABS.M (cm2) | - | 61.62 | 67.17 | 9.0 |
| MRI-ABS.IMF (cm2) | - | 8.10 | 4.96 | -39 |
| MRI-%IMF (%) | - | 11.80 | 7.05 | -4.81 |
| MRI-VAT (cm2) | - | 46 | 40.5 | -12% |
| MRI-trunk SAT (cm2) | - | 182 | 142 | -22% |
Lipid panel demonstrated increase in low-density lipoprotein cholesterol from 121 to 130 mgdL-1 (7.4%) with concomitant decrease in triglycerides from 121 to 83 mgdL-1 (31.4%) and increase in HbA1c from 5.1% to 5.5%. No detectable changes were noted HDL-C, total cholesterol and ratio of total cholesterol: HDL-C. Baseline BMR of the case report was 1388.4 kcal/d and remained unchanged (1365.6 kcal/d) following 16 wk of administering TRT.
The current case report was analyzed in a retrospective fashion. The findings demonstrated that lowering caloric intake and percentage macronutrients of fat and protein may have contributed to positive changes in total and regional body composition in a male with chronic SCI. The addition of TRT may primarily helped to maintain lean mass and BMR; which is commonly impacted negatively during a weight loss regimen. The participant lost 8% (6.4 kg) of his total body weight, which is consistent with a previous report that noted a total body weight loss of 7% following Mediterranean-style diet in three men with SCI[10]. Whole body lean mass increased by 7% over 16 wk. Participant’s absolute thigh muscle CSA increased by 9% as accompanied with l2% and 22% decrease in trunk VAT and SAT, respectively. Clinically, these changes are highly significant because of the recognized associations between lean mass, BMR, and several cardio-metabolic disorders after SCI[2-5]. The current case report also suggests that high protein intake with TRT may have played a role in preservation of lean mass, especially with reduction in caloric intake.
A reduction in total caloric intake by 440 kcal/d may explain some of the observed changes in body composition. Despite the 25% reduction in caloric intake, we could not refer to it as a caloric restriction study because the intervention was only limited to 8 wk period. Caloric restriction studies reported period close to 6 mo up to a year[32]. Based on the current findings, it is possible to speculate that combining exercise with a similar dietary manipulation may be an effective strategy to reduce cardio-metabolic risk factors after SCI. We have previously shown that neuromuscular electrical stimulation (NMES)-resistance training for 12-16 wk accompanied with a standard dietary program (45% carbohydrate, 30% fat and 25% protein) was an effective strategy in reducing VAT in persons with SCI[16,20]. Although the case report did not receive resistance training[16], daily administration of TRT may have contributed to preservation of lean mass and loss of both VAT and SAT. This is really important because a recent report demonstrated the negative association between serum testosterone level and VAT. Persons with lower testosterone level have 72% greater VAT than those with normal testosterone level[14].
BMR accounted for 65% of the total energy expenditure and may play a major role in maintaining optimal energy balance[21]. During the first 8 wk, the participant consumed an average of 1802 kcal/d, which exceeded his measured BMR (1388.4 kcal/d). During phase II, the average caloric intake was 1357.2 kcal/d or 440 kcal lower than what has been consumed in the first 8 wk. Despite the reduction in caloric intake following Phase II, BMR remained unchanged at the end of the 16 wk. Administering TRT may have had a protective effect in maintenance of BMR by preserving lean mass, because reduction in BMR could potentially lead to further gain in body weight.
A previous trial using weekly dietary recalls suggested that persons with SCI consumed a high fat diet (32%-50% fat)[7]. The case report reduced his caloric fat intake by 6.5% between phases I and II and maintained a recommended daily allowances (RDA) of 30%. However, it remains unclear whether the improvements in body composition are primarily driven by overall caloric reduction or decreasing percentage fat intake. Additionally, percentage carbohydrate was maintained in the range between 39.9%–41.6% across the 16 wk for both the case report and cohort. The average carbohydrate consumption for the case report and the study cohort was consistently less than the recommended RDA of 45%, likely due to higher fat consumption by the study cohort throughout the 16 wk and the case report in Phase I.
Increased protein intake during phase II may have contributed to the observed gains in lean mass and decreased total-body and regional adiposity. Dietary analysis revealed that the participant increased his protein intake by 8% compared to phase I. He also consumed 8% more calories from protein than the study cohort during phase II of the trial. Increased protein consumption likely contributed to a positive nitrogen balance, creating an ideal environment for protein synthesis, especially when accompanied by TRT[9,22]. The Food and Nutrition Board of the National Academy of Sciences recommends a modest 0.8 g of protein per kg of body weight or roughly 10%-30% of daily caloric intake[23]. The current SCI guidelines recommend that persons with SCI consume 0.8-1.0 g/kg of body weight, with additional protein added in the presence of pressure ulceration[23]. We have previously shown that persons with SCI consumed close to 1.1 g/kg body weigh during 12 wk of resistance training[20]. Because the case report and the study cohort received a similar dose of TRT, it is fair to speculate that the combining effects of higher protein intake and TRT may result in increase in whole body lean mass and thigh muscle CSA in the case report. However, a recent study noted that high protein intake for 8 wk did not result in increase in muscle size after SCI[24]. The authors recommended that loading the muscle using surface NMES with resistance training is considered a favorable rehabilitation approach to ameliorate muscle atrophy after SCI[24].
Moreover, because protein requires substantial energy (20 of BMR) to catabolize after ingestion, protein may have shifted substrate utilization from reliance on carbohydrates to fats as source of energy[25]. This shift may have contributed to the reductions observed in SAT, IMF, and total body fat. However, as noted earlier, percentage carbohydrates di were not different between phase I and phase II of the trail; suggesting that the case report consumed enough carbohydrates and utilized both carbohydrates and fats as source for energy.
The 2015-2020 Dietary Guidelines for Americans recommends 6-8 g of soluble fiber daily[26].Throughout the 16 wk trial, the participant consumed 7 g of soluble fiber per day. Consistently, the case report consumed an average of 3.8 and 4.1 more grams of soluble fiber than the cohort during phase I and II, respectively. Because fiber intake showed no changes over 16 wk, this may have played an indirect role in the changes observed in body weight and body composition. Fiber intake was shown to be associated with weight loss due to increased appetite control and slower digestion in abled-bodied individuals[27,28]. Additionally, a meta-analysis concluded that the risk of type II diabetes decreased by 6% per 2 g per day increment in fiber intake for men and women.
The current case report is purely a retrospective observational study, because we did not intentionally plan to manipulate participant’s dietary habits compared to the study cohort. We have also shown a snap-shot of body composition before and after intervention; body composition should have been measured at the end of phase I and before starting phase II. Direct comparisons in body composition parameters were also not performed between the case report and the study cohort. It is difficult based on the current observation to indicate that the changes in body composition are solely due to manipulation in dietary habits; Therefore, causality cannot be directly determined; the assertions made are purely speculative and further studies are warranted. We also did not measure levels of physical activity among our study cohort. During the course of the trial, increasing level of physical activity may have contributed to significant changes in body composition. However, we studied persons with motor complete SCI who are the lowest on the spectrum of physical activity. Despite the fact that clear instruction was given of not to engage in any routine exercise program, physical activity logs should have been collected to monitor free living activity during the course of the trial.
In conclusion, dietary manipulation of caloric intake and macronutrients (percentage fat and percentage protein) resulted in remarkable changes in body composition in a person with motor complete SCI. Reduction in caloric intake and TRT may positively serve to decrease both fat mass and VAT in the case report. The 8 wk dietary manipulation program was associated with remarkable weigh loss without losing the metabolically active lean tissue. Supplementation of TRT combined with high protein intake may have served as a protective factor to preserve both lean mass and BMR in the participant with SCI. Considering the retrospective nature of the case report, there are number of confounding factors that may have contributed to the findings and further interventional studies are warranted to confirm the current observation.
Reduced level of physical activity, high-fat diet and skeletal muscle atrophy are key factors that are likely to contribute to deleterious changes in body composition and metabolic following spinal cord injury (SCI). Reduced caloric intake with lowering percentage macronutrients of fat and increasing protein intake may likely to improve body composition parameters and decrease ectopic adiposity after SCI.
Currently, there is no standard of care of established evidence on how to improve body composition parameters and to reduce ectopic adiposity after SCI.
To highlight the necessary dietary adjustments as far as caloric and macronutrient intakes responsible for improving body composition and metabolic profile following participation in a 16 wk clinical trial of administering low-dose testosterone replacement therapy in a male with SCI.
We, retrospectively, tracked the dietary habits and body composition parameters in a 31-year-old male with motor-complete T5 SCI after administering low-dose testosterone replacement therapy (TRT) for 16 wk. Detailed body composition was evaluated via dual energy x-ray absorptiometry and magnetic resonance imaging. Participant was asked to turn in weekly 5 d dietary recalls to measure total energy intake, percentage carbohydrate, percentage fat, percentage protein, and total soluble fiber intake.
Lowering caloric intake by 25% and fat intake by 6.5% resulted in decreased body weight, total and regional body fat mass and ectopic adiposity. Both lean mass and BMR remained physiologically unchanged following the 16 wk intervention.
The current case report highlighted the significance of reducing caloric intake and manipulating macronutrients with TRT on the changes in total and regional body composition in a male with SCI.
The current case report may serve as supporting evidence for future clinical trial that may target manipulation of dietary intake with and without ergogenic aids similar to exercise and TRT to improve cardio-metabolic profile in persons with SCI.
We would like to thank Refka Khalil for help in data capturing and analysis. We thank the study participants for their time and effort. We would also like to thank Hunter Holmes McGuire Research Institute and Spinal Cord Injury Services and Disorders for providing the environment to conduct clinical human research trials. We appreciate the VAMC Radiology Service for using the magnet for research purposes.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elgafy H S-Editor: Zhang L L-Editor: Filipodia E-Editor: Qi LL
| 1. | Wong S, Kenssous N, Hillier C, Pollmer S, Jackson P, Lewis S, Saif M. Detecting malnutrition risk and obesity after spinal cord injury: a quality improvement project and systematic review. Eur J Clin Nutr. 2018;72:1555-1560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Gorgey AS, Gater DR. Regional and relative adiposity patterns in relation to carbohydrate and lipid metabolism in men with spinal cord injury. Appl Physiol Nutr Metab. 2011;36:107-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Abilmona SM, Gorgey AS. Associations of the trunk skeletal musculature and dietary intake to biomarkers of cardiometabolic health after spinal cord injury. Clin Physiol Funct Imaging. 2018;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Buchholz AC, McGillivray CF, Pencharz PB. Differences in resting metabolic rate between paraplegic and able-bodied subjects are explained by differences in body composition. Am J Clin Nutr. 2003;77:371-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 124] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Spungen AM, Wang J, Pierson RN, Bauman WA. Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol (1985). 2000;88:1310-1315. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 134] [Cited by in F6Publishing: 139] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Moore CD, Craven BC, Thabane L, Laing AC, Frank-Wilson AW, Kontulainen SA, Papaioannou A, Adachi JD, Giangregorio LM. Lower-extremity muscle atrophy and fat infiltration after chronic spinal cord injury. J Musculoskelet Neuronal Interact. 2015;15:32-41. [PubMed] [Cited in This Article: ] |
| 7. | Gorgey AS, Caudill C, Sistrun S, Khalil RE, Gill R, Castillo T, Lavis T, Gater DR. Frequency of Dietary Recalls, Nutritional Assessment, and Body Composition Assessment in Men With Chronic Spinal Cord Injury. Arch Phys Med Rehabil. 2015;96:1646-1653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Tomey KM, Chen DM, Wang X, Braunschweig CL. Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Arch Phys Med Rehabil. 2005;86:664-671. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Levine AM, Nash MS, Green BA, Shea JD, Aronica MJ. An examination of dietary intakes and nutritional status of chronic healthy spinal cord injured individuals. Paraplegia. 1992;30:880-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 56] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Bigford GE, Mendez AJ, Betancourt L, Burns-Drecq P, Backus D, Nash MS. A lifestyle intervention program for successfully addressing major cardiometabolic risks in persons with SCI: a three-subject case series. Spinal Cord Ser Cases. 2017;3:17007. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Nevitt M, Harris TB. Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study. Am J Clin Nutr. 2005;82:872-8; quiz 915-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 285] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 12. | Durga A, Sepahpanah F, Regozzi M, Hastings J, Crane DA. Prevalence of testosterone deficiency after spinal cord injury. PM R. 2011;3:929-932. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Nightingale TE, Moore P, Harman J, Khalil R, Gill RS, Castillo T, Adler RA, Gorgey AS. Body composition changes with testosterone replacement therapy following spinal cord injury and aging: A mini review. J Spinal Cord Med. 2018;41:624-636. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Abilmona SM, Sumrell RM, Gill RS, Adler RA, Gorgey AS. Serum testosterone levels may influence body composition and cardiometabolic health in men with spinal cord injury. Spinal Cord. 2019;57:229-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Bauman WA, Cirnigliaro CM, La Fountaine MF, Jensen AM, Wecht JM, Kirshblum SC, Spungen AM. A small-scale clinical trial to determine the safety and efficacy of testosterone replacement therapy in hypogonadal men with spinal cord injury. Horm Metab Res. 2011;43:574-579. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Gorgey AS, Khalil RE, Gill R, Gater DR, Lavis TD, Cardozo CP, Adler RA. Low-Dose Testosterone and Evoked Resistance Exercise after Spinal Cord Injury on Cardio-Metabolic Risk Factors: An Open-Label Randomized Clinical Trial. J Neurotrauma. 2019;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Gorgey AS, Dudley GA. Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord. 2007;45:304-309. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 269] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 18. | Gorgey AS, Cirnigliaro CM, Bauman WA, Adler RA. Estimates of the precision of regional and whole body composition by dual-energy x-ray absorptiometry in persons with chronic spinal cord injury. Spinal Cord. 2018;56:987-995. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Nightingale TE, Gorgey AS. Predicting Basal Metabolic Rate in Men with Motor Complete Spinal Cord Injury. Med Sci Sports Exerc. 2018;50:1305-1312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | Piekarski D, Potier P, Giannotti C. Study of the mode of action of some nitrodiphenyl ethers. Free Radic Res Commun. 1990;10:85-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 135] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Buchholz AC, Pencharz PB. Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care. 2004;7:635-639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 22. | Khalil RE, Gorgey AS, Janisko M, Dolbow DR, Moore JR, Gater DR. The role of nutrition in health status after spinal cord injury. Aging Dis. 2013;4:14-22. [PubMed] [Cited in This Article: ] |
| 23. | Academy of Nutrition and Dietetics. 2009 Spinal Cord Injury Evidence-Based Nutrition Practice Guidelines. Accessed on March 14th. 2019; Available from: https://www.andeal.org. [Cited in This Article: ] |
| 24. | Yarar-Fisher C, Polston KFL, Eraslan M, Henley KY, Kinikli GI, Bickel CS, Windham ST, McLain AB, Oster RA, Bamman MM. Paralytic and nonparalytic muscle adaptations to exercise training versus high-protein diet in individuals with long-standing spinal cord injury. J Appl Physiol (1985). 2018;125:64-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Stachowiak JC, Brodsky FM, Miller EA. A cost-benefit analysis of the physical mechanisms of membrane curvature. Nat Cell Biol. 2013;15:1019-1027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 157] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 26. | Yao B, Fang H, Xu W, Yan Y, Xu H, Liu Y, Mo M, Zhang H, Zhao Y. Dietary fiber intake and risk of type 2 diabetes: a dose-response analysis of prospective studies. Eur J Epidemiol. 2014;29:79-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 167] [Cited by in F6Publishing: 161] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 27. | Rebello C, Greenway FL, Dhurandhar NV. Functional foods to promote weight loss and satiety. Curr Opin Clin Nutr Metab Care. 2014;17:596-604. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Zhu Y, Hsu WH, Hollis JH. The impact of food viscosity on eating rate, subjective appetite, glycemic response and gastric emptying rate. PLoS One. 2013;8:e67482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |