Published online Jul 16, 2018. doi: 10.12998/wjcc.v6.i7.143
Peer-review started: February 28, 2018
First decision: March 15, 2018
Revised: March 23, 2018
Accepted: April 22, 2018
Article in press: April 22, 2018
Published online: July 16, 2018
Our paper describes the key surgical points of pediatric choledochocystectomy performed completely by Da Vinci robotic system. A choledochocystectomy was safely carried out for a girl at our hospital, and without any complication. Then systematic literature review was done to discuss the methods of intestine surgery and intestinal anastomosis, the use of 3rd robotic arm, the surgical safety and advantages comparing open and laparoscopic surgery. We systematically reviewed choledochocystectomy for children performed by robotic surgery. We included a total of eight domestic and foreign reports and included a total of 86 patients, whose average age was 6.3 (0.3-15.9) years; the male-to-female ratio was 1:3.5 (19:67). Seven patients experienced conversion to open surgery, and the surgery success rate was 91.9% (79/86). The average total operation time was 426 (180-520) min, the operation time on the machine was 302 (120-418) min, 11 cases used the number 3 arm, and the remaining mainly used the hitch-stitch technique to suspend the stomach wall and liver. Forty-seven patients underwent pull-through intestine and intestinal anastomosis, and 39 patients underwent complete robotic intestine surgery and intestinal anastomosis. The hospitalization time of robotic-assisted choledochocystectomy was 8.8 d. Eight patients had biliary fistula and were all cured by conservative treatment and continuous observation. One patient had anastomotic stenosis, and one patient had wound dehiscence, both cured by surgery. Choledochocystectomy for children performed by completely robotic surgery and Roux-en-Y hepaticojejunostomy is safe and feasible. The initial experience shows that this surgical approach has a clearer field than the traditional endoscopy, and its operation is more flexible, the surgery is more accurate, and the injury is smaller. With the advancement of technology and the accumulation of surgeons’ experience, robotic surgery may become a new trend in this surgical procedure.
Core tip: Our paper describes the key surgical points of pediatric choledochocystectomy performed completely by Da Vinci robotic system. A choledochocystectomy was carried out for a girl at our hospital, then systematic literature review was done to discuss the methods of intestine surgery and intestinal anastomosis, the use of 3rd robotic arm, the surgical safety and advantages comparing open and laparoscopic surgery.
- Citation: Wang XQ, Xu SJ, Wang Z, Xiao YH, Xu J, Wang ZD, Chen DX. Robotic-assisted surgery for pediatric choledochal cyst: Case report and literature review. World J Clin Cases 2018; 6(7): 143-149
- URL: https://www.wjgnet.com/2307-8960/full/v6/i7/143.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i7.143
Congenital choledochal cysts (CCs) are disease of cystic dilatations of the bile duct. Its incidence in European countries and in the United States is 5-15 cases per million people[1-5], while it is more common in Asian countries, with an incidence up to 1000 cases per million people[6-8]. The main treatment is the complete resection of the cyst, hepaticojejunostomy and Roux-en Y anastomosis[9]. Minimally invasive treatment of CCs in children is currently the mainstream of treatment at home and abroad, including laparoscope-assisted and robotic treatment methods.
In 2006, Woo et al[10] reported the first robotic laparoscope-assisted type I choledochocystectomy for a 5-year-old child patient in the world. Subsequently, there were related reports[11-15]. In 2013, Geyuan Huang et al[16] of the Queen Mary Hospital of the University of Hong Kong of China completed the first treatment of a case of CCs with a robotic surgical system in China. In 2015, Kim et al[17] reported 36 cases of children’s CCst treated by robotic surgery, the largest number so far. In 2016, Dr. Shaotao Tang first reported the treatment of three cases of CCs by robotic surgery in the mainland area[18].
In this paper, we report the application of the Da Vinci surgical system to treat one case of type IVa CCs completely with a robotic system. We also conduct a literature review, aiming at exploring the feasibility of adopting complete robotic surgery for the treatment of children’s CCs and summarizing the key points of using this technology.
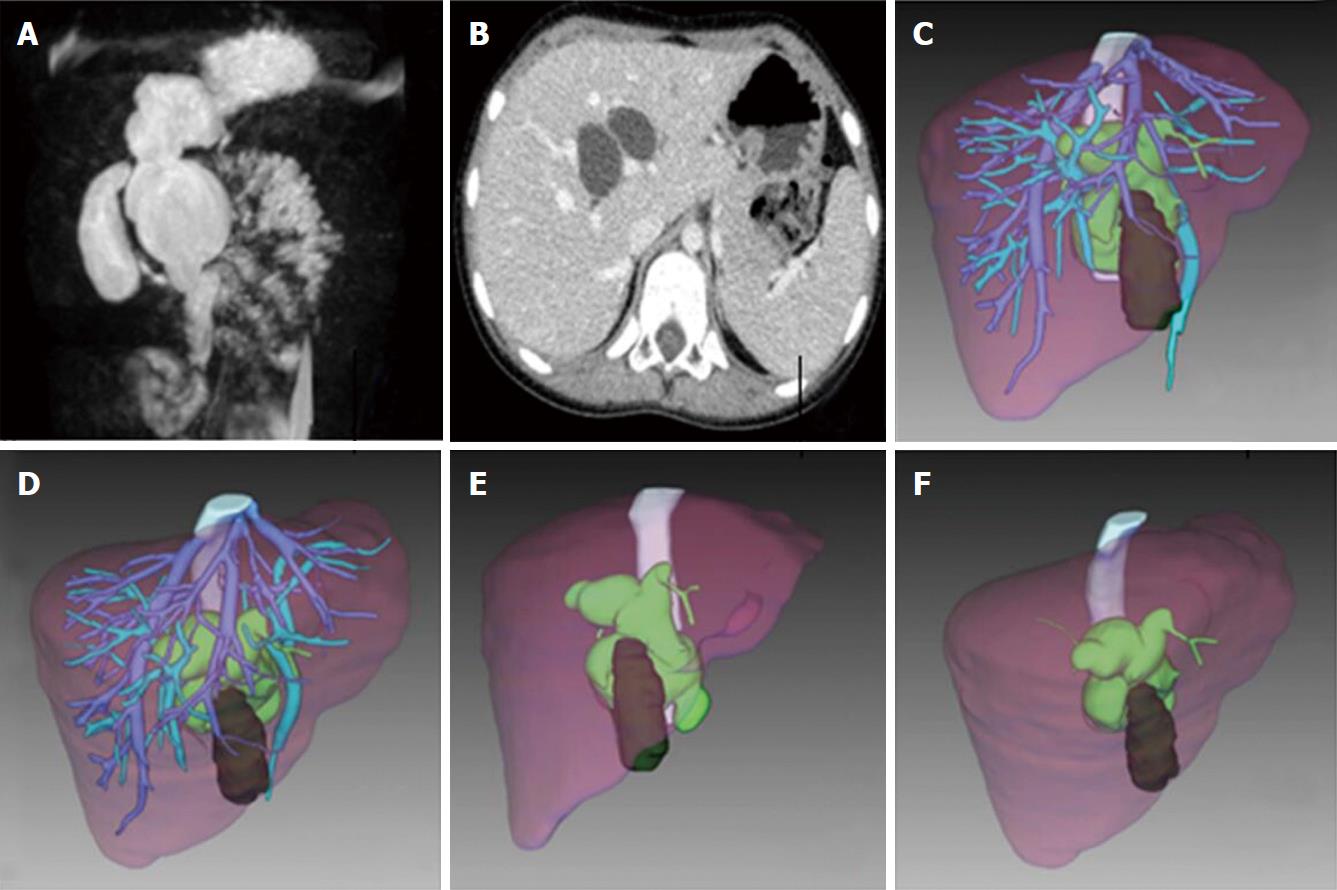
A 7-year-old female experienced abdominal pain without an obvious cause in May 2011, showing continuous dull pains, most of which could be self-relieved. Subsequently, the patient underwent imaging examination at our hospital, which indicated multiple intrahepatic and extrahepatic cystic dilatation of bile duct (Figure 1). It was clearly diagnosed as type IVa CCs. After the preoperative examinations, we decided to carry out robotic-assisted laparoscopic choledochocystectomy and biliary-intestinal anastomosis.
With the patient in the supine position, the operation bed was in the reverse Trendelenburg position. After the anesthesia was successful, the anesthesiologists conducted internal jugular vein intubation and radial artery catheterization and placed a gastric tube and urinary catheter. Direct trocar puncture was done on the abdominal wall between the umbilicus and pubic symphysis to establish pneumoperitoneum. The pressure was 12 cmH2O, and a 12-mm trocar and robotic lens were inserted.
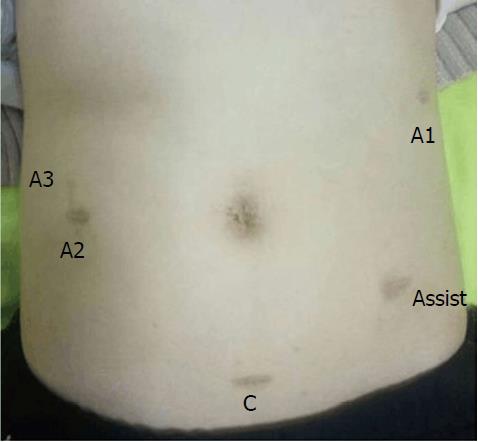
Being monitored under the lens, at about the level of umbilicus, the 8-mm-diameter trocars of arm 1 and arm 2 of the robotic instrument were inserted into the left and right abdomen, respectively, and the arm 3 trocar was inserted into the right upper abdomen at the level of the axillary line (Figure 2). A 12-mm auxiliary hole was created between arm 1 and the lens. The robotic arms were placed from the end of the head and were connected.
No significant ascites was detected in the abdominal cavity. The gallbladder volume was approximately 7.0 cm × 3.0 cm. The common bile duct was dilated with a diameter of 5.5 cm. Its surface showed hyperemia and edema. An electric hook was used to separate the adhesion between the gallbladder and liver. The gallbladder arteries were ligated, and the gallbladder neck was dissected all the way to the common hepatic duct. The adhesions between the outer serosal membrane of the choledochal cyst and the duodenum and the portal vein were separated. The common hepatic duct was cut transversely. The diameter of the common hepatic duct was approximately 3.2 cm. The left and right hepatic duct openings were visible at the proximal end, and the flow of bile was unobstructed. There was no obvious stenosis. The gallbladder and the choledochal cyst to be removed were turned upside down, the common bile duct was dissected till near the head of the pancreas, and the end of the cyst was significantly narrowed with a diameter of approximately 1 cm and was sutured twice.
A stapler (EC-60) was used to cut the jejunum transversely at 15 cm from the duodenojejunal flexure, and 35 cm of the proximal end towards the hilus was saved as ascending arm. After joining the jejunum and the ascending branch by three stitches, we used a stapler to perform end-to-side anastomosis between the ascending arm and the proximal jejunum. The 3-0 absorbable suture was used for full-thickness interrupted suture of the intestinal wall, which was reinforced by interrupted suture. The ascending arm of the distal jejunum was lifted from the front of the colon to the common hepatic duct location to perform anastomosis. A 4-0 absorbable suture was used for full-thickness continuous suture of the posterior wall. Then the anterior wall was sutured, and interrupted suturing was done for seromuscular layer for reinforcement.
Physiological saline was used for rinsing. One abdominal drainage tube was placed on the lateral posterior side of the gallbladder-intestine anastomosis, which came out of the body through the puncture hole of the arm 2 trocar and was connected to a negative-pressure drainage ball. The abdominal cavity was confirmed to have no active bleeding, and the devices and gauzes were all counted. No. 3 absorbable suture was used to suture the muscular layer at each trocar location, 4-0 absorbable suture was used for interrupted suturing of subcutaneous tissue. Biological fibrin glue was used to bond the edges of the skin, and the drainage tube was properly fixed. Tissue aid was applied to the wound.
The surgery went smoothly. The operation time was 420 min, of which the robot operation time was 370 min. The bleeding was approximately 100 mL. There was no perioperative blood transfusion. Two days after the operation, the gastric tube was removed, and fluid and semi-fluid food were given gradually. Two antibiotics were administered for 3 d. Seven days after operation the abdominal drainage tube was removed. The patient was discharged 9 d after the operation. No serious complications occurred. Routine pathological examination further confirmed the diagnosis of cystic dilatation of the common bile duct.
The Da Vinci Surgical System (Intuitive Surgical, Inc., Mountain View, CA, United States) was approved by the FDA in 2000 for clinical use and is currently the most widely used robotic surgical system. The Da Vinci system has a unique 3D high-definition and 10 × magnification imaging system, the separation process is more accurate, and the secondary injury can be effectively avoided. The simulation wrist with a shaking filtration function of the mechanical arm of the robot has a better dexterity and greater range of activities than the traditional laparoscopic instruments, making the anastomosis process easier and more sophisticated.
The Alonso-lej classification revised by Todani is the most widely used classification method of CCs. It divides bile duct cysts into five types. More than 90% of the bile duct cyst cases reported in the literature belong to types I and IVa (50% to 80% type I). Type IVa bile duct cysts are more common in adult patients, and it is the nodus of the current treatment. This bile duct dilatation patient has intrahepatic and extrahepatic bile duct dilatation, belonging to type IVa of Todani’s classification and type D2 of Jiahong Dong’s classification. Its treatment method is still controversial. After considering the safety of the surgery, we chose complete resection of the dilated extrahepatic bile duct and had a high-position anastomosis to the greatest extent possible. According to Jiahong Dong, this type of patient should undergo perihilar resection to remove the primary bile duct, and if necessary, biliary duct plasty can be performed, followed by biliary-intestinal anastomosis. To complete this type of surgery by robotic surgery requires the accumulation of case practice, and it has a higher technical requirement.
In most type IVa patients, it is more difficult to completely remove the cyst, and there is a greater chance of postoperative cholangioenterostomy stenosis. When a type IVa cyst involves the left or right hepatic duct or its secondary branches, the number of secondary and tertiary bile ducts that join the cyst is higher. The diameter of the bile duct is smaller, and if gallbladder-intestine anastomosis is done individually, not only is intraoperative anastomosis difficult, but the chance of having postoperative gallbladder-intestine anastomotic stenosis is also higher, which affects the prognosis. At this time, part of the cyst wall can be kept above the cyst, and the remaining cyst wall and the jejunum can undergo large-diameter gallbladder-intestine anastomosis to reduce the occurrence of postoperative anastomotic stenosis.
In recent years, reports on cases of CCs involving intrahepatic bile ducts and the resection of the involved liver while conducting choledochocystectomy are increasing[19,20]. For patients with type IVa CCs, simultaneous extrahepatic bile duct resection and partial liver resection has lower reoperation rates and stenosis rates in adults compared with children[21]. In the meantime, for adults, simultaneous liver resection can reduce the risk of postoperative canceration[22]. If hepatectomy is safe, simultaneous extrahepatic bile duct resection and partial hepatectomy may be considered. However, for child patients, considering the huge damage caused by liver resection, usually only choledochocystectomy is carried out[23]. Of course, this issue still needs in-depth research and discussion. For the type IVa and V patients with more diffuse intssrahepatic lesions and lesions involving the left and right liver, the treatment is difficult. The optimal treatment for such patients is liver transplantation.
We systematically reviewed choledochocystectomy for children performed by robotic surgery. A total of eight domestic and foreign reports were included. A total of 86 patients were included, with an average age of 6.3 (0.3-15.9) years, and the male-to-female ratio was 1:3.5 (19:67). Seven patients underwent conversion to open surgery, and the success rate of the surgeries was 91.9% (79/86). The average total operation time was 426 (180-520) min, the operation time on the machine was 302 (120-418) minutes, 11 cases used the number 3 arm, and the remaining mainly used the hitch-stitch technique to suspend the stomach wall and liver.
Forty-seven patients used pull-through intestine and intestinal anastomosis, and 39 patients underwent complete robotic intestinal surgery and intestinal anastomosis. The hospitalization time of robotic-assisted choledochocystectomy was 8.8 d.
The complications that had clear records in the reports were biliary fistula, anastomotic stenosis, and wound dehiscence. Eight patients had biliary fistula and were all cured by conservative treatment and continuous observation. One patient had anastomotic stenosis, and one patient had wound dehiscence, both of them cured by surgery.
Some 86.1% of patients with CCs have obvious symptoms, which are mainly abdominal pain (78%), vomiting (36%), jaundice (22%), and fever (22%)[19]. Their pathophysiological basis is pancreaticobiliary malunion. Abdominal ultrasound examination and imaging examination, such as CT, MRI, and MRCP, shows a significant expansion of the extrahepatic bile duct, which is of cystic or fusiform shape. Among children with congenital dilatation of the common bile duct, the main symptoms of those with cystic dilatation of the common bile duct are jaundice and abdominal mass, while the most common manifestation of patients with fusiform dilatation of the common bile duct is abdominal pain[20].
Surgical system Choledochocystectomy performed by a robot is one of the more challenging operations in the field of pediatric surgery. This is mainly because the child’s abdominal space is small, the exposure of the operation field is difficult and the distance between the operation centers of the two anastomoses is great. Therefore, each center has different choices for the child’s body position, the use of the No.3 mechanical arm, and in vivo/in vitro intestinal anastomosis. We used the reverse Trendelenburg supine position for this child patient undergoing robotic choledochocystectomy, and some centers suggest that the overall elevation of the child can achieve a better surgical field[14].
The key point of robotic choledochocystectomy is to expose the hilar region, which can be done by five main methods: (1) Hitch-stitch suspension technique[11]: 2-0 sutures are passed through the abdominal wall under the left and right ribs, respectively. The left suture suspends the distal end of the gallbladder, while the right suture suspends the round ligament of the liver near the edge of the liver. Then the suture passes through the abdominal wall. The sutures are pulled to sufficiently expose the hilus and then are fixed outside the body; (2) Liver retractor (Nathanson retractor)[15]: An incision is made on the right upper abdomen, and a liver retractor is inserted to fully expose the surgical region; (3) Internal suspension method[14]: This refers to the suture and suspension of the round ligament of the liver, the gallbladder, and the stomach wall on the abdominal wall; (4) Double auxiliary holes method: Meehan et al[11] reported that a 12-mm auxiliary hole was made on the left and a 5-mm auxiliary hole was made on the right; and (5) Three-arm method: The third robotic operation arm is inserted into the right upper abdomen[14,17].
The robotic operation method used at our center is that using three operation arms. The main role of the No. 3 robot arm is to pull the liver and stomach wall and to pull the intestine while performing intestine-intestine anastomosis to achieve a better tissue exposure. Our experience has shown that it is safe and feasible to use three robotic operation arms for children, and previous studies also reached the same conclusion. A child’s abdominal wall is relatively weak, and sometimes the trocar of the mechanical arm will be close to the target area. Under this situation, some centers use a suture to fix the trocar. Our experience shows that trocar fixation can be achieved without external fixation by adjusting the position of the trocar’s remote center. The rule is that, when inserting the trocar that is close to the operation region (< 10 cm), the remote center at least needs to reach the width indication line to prevent the device from frequently falling out during operation and to shorten the operation time. A distant trocar only needs to reach the proximal fine indication band.
In vitro anastomosis or in vivo anastomosis can be used for the intestine and intestinal anastomosis. The literature review included 86 patients: 47 underwent In vitro anastomosis, while 39 underwent in vivo anastomosis. In theory, the docking process by the robotic system is more difficult and time-consuming. In vitro jejunum–jejunum end-to-end anastomosis can be performed first, and then robotic separation and resection of the cyst can be done to shorten the operation time. Which anastomosis method is used mainly depends on the experience of the surgeon. In a study in Korea, we found that among the cases of robotic choledochocystectomy, 13 of the first 14 patients underwent in vitro anastomosis, while one underwent in vivo anastomosis. With the accumulation of experience, they used in vivo anastomosis for all of their next 36 cases. When compared with the patients who underwent in vitro anastomosis, the total operation time did not have a significant difference. This suggests that with the accumulation of experience, the use of in vivo anastomosis is feasible and effective.
By reviewing the literature and summarizing our experience, we are drawn to the following conclusions regarding robotic choledochocystectomy: (1) Body position should be in the supine position and adjusted to the reverse Trendelenburg position. Based on personal preferences, the surgeon should decide whether the body is lifted; (2) In vitro intestine-intestine anastomosis through the umbilical incision is a relatively safe and simple method; (3) Choose the appropriate method to fully expose the hilus, common bile duct, and intestine; and (4) Making full use of the third operation arm of the robot can improve surgical efficiency and reduce operation difficulty.
As an emerging method, robotic surgery provides undoubted technical advantages over conventional laparoscopy[24]. It has 3D imaging, tremor filter, and articulated instruments[25]. With this advanced equipment, robotic surgery is superior to conventional laparoscopic surgery due to its significant improvements in visibility and manipulation[26-28]. A systematic review demonstrated robotic vs laparoscopic Roux-en-Y gastric bypass in morbidly obese patients identified seven relevant studies of 1686 patients[29]. There was a significantly reduced incidence of anastomotic stricture in the robotic group (POR = 0.43; 95%CI: 0.19-0.98; P = 0.04). No significant difference between robotic and laparoscopic groups for anastomotic leak, post-operative complications, operative time, and length of hospital stay is found.
Robotic surgery also faces many challenges: (1) Cost is higher. For instance, an extra 20-30 thousand RMB is needed; (2) Currently, it is still controversial how old children need to be to undergo robotic-assisted surgery; (3) The tactile feedback needs to be improved. For beginners, making knots and tissue pulling are prone to excessive force, causing adverse consequences; and (4) Indications: if the surgical effect is similar, the surgical difficulty is not high, and the cosmetic effect is worse than that of laparoscopy, there is some controversy about using robotic surgery for this treatment (Table 1).
| No. | Ref. | Year | Cases number | Age | Male/female | Total OPT(min) | Robotic time (min) | 3rd arm | Roux limb | LOH (d) | Complications |
| 1 | Woo et al[10] | 2006 | 1 | 5 | 0/1 | 440 | 390 | Yes | Extracorporeal | 4 | No |
| 2 | Meehan et al[11] | 2007 | 2 | 5.5 (2-9) | 1/1 | 458 | 418 | Yes | Intracorporeal | 4 | No |
| 3 | Akaraviputh et al[12] | 2010 | 1 | 14 | 0/1 | 180 | 120 | Yes | Extracorporeal | 20 | Bile leakage |
| 4 | Chang et al[14] | 2012 | 14 | 5.3 | 2/12 | 570 | 324 | Yes No | Extracorporeal 13 Intracorporeal 1 | 9 | Conversion to open surgery 1, biliary fistula 1, stenosis 1 |
| 5 | Huang et al[16] | 2013 | 2 | 6 | 2/0 | 396 | NA | NA | Extracorporeal | NA | Conversion to open surgery 1 |
| 6 | Dawrant et al[13] and Alizai et al[15] | 2014 | 27 | 5.4 (0.3-15.9) | 7/20 | 479 | 302 | NA | Extracorporeal | 7 | Conversion to open surgery 5, wound dehiscence 1, bile leak |
| 7 | Kim et al[17] | 2015 | 36 | 4.8 | 6/30 | 520 | 300 | Yes | Intracorporeal | 9.2 | 5 |
Taken together, choledochocystectomy for children completely by robotic surgery and Roux-en-Y hepaticojejunostomy is safe and feasible. Our initial experience shows that this surgical approach has a clearer field than the traditional endoscopy, and its operation is more flexible, the surgery is more accurate, and the injury is smaller. With the advancement of technology and the accumulation of surgeons’ experience, robotic surgery may become a new trend in this surgical procedure.
A 7-year-old female experienced abdominal pain without an obvious cause which could be self-relieved. The patient underwent imaging examination at our hospital, which indicated multiple intrahepatic and extrahepatic cystic dilatation of bile duct. It was diagnosed as type IVa congenital choledochal cysts (CCs).
It was clearly diagnosed as type IVa CCs.
The patient underwent imaging examination at our hospital, which indicated multiple intrahepatic and extrahepatic cystic dilatation of bile duct.
Patient underwent an imaging examination at our hospital, which indicated multiple intrahepatic and extrahepatic cystic dilatation of bile duct.
The pathological examination confirmed the diagnosis of cystic dilatation of the common bile duct.
We carried out robotic-assisted laparoscopic choledochocystectomy and biliary-intestinal anastomosis after the preoperative examinations.
The first robotic laparoscope-assisted type I choledochocystectomy for a 5-year-old child patient in the world was reported in 2006. Subsequently, there were some related reports fellows. The Queen Mary Hospital of the University of Hong Kong in China completed the first treatment of a case of CCs with a robotic surgical system in 2013. 36 cases of children’s CCs treated by robotic surgery were reported in 2015, the largest number so far. Dr. Shaotao Tang first reported the treatment of three cases of CCs by robotic surgery in the mainland area in 2016.
CCs are disease of cystic dilatations of the bile duct. Its incidence in European countries and United States is 5-15 cases per million people. It is more common in Asian countries with an incidence of 1000 cases per million people.
Choledochocystectomy for children completely by robotic surgery is safe and feasible. Our initial experience shows that this surgical approach has a clearer field than traditional endoscopy, and a more flexible operation. The surgery is more accurate and the injury is smaller. Robotic surgery may become a new trend in this surgical procedure with the advancement of technology and the accumulation of surgeons’ experience.
We want sincerely to express our cordial thanks to EDDA technology company, providing IQQA software for liver 3D reconstruction.
CARE Checklist (2013) statement: This report follows the guidelines of the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Czubkowski P, Faerch K, Noshiro H, Sis B S- Editor: Wang XJ L- Editor: A E- Editor: Tan WW
| 1. | Olbourne NA. Choledochal cysts. A review of the cystic anomalies of the biliary tree. Ann R Coll Surg Engl. 1975;56:26-32. [PubMed] [Cited in This Article: ] |
| 2. | Lenriot JP, Gigot JF, Ségol P, Fagniez PL, Fingerhut A, Adloff M. Bile duct cysts in adults: a multi-institutional retrospective study. French Associations for Surgical Research. Ann Surg. 1998;228:159-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 82] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Howell CG, Templeton JM, Weiner S, Glassman M, Betts JM, Witzleben CL. Antenatal diagnosis and early surgery for choledochal cyst. J Pediatr Surg. 1983;18:387-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 67] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | O'Neill JA Jr. Choledochal cyst. Curr Probl Surg. 1992;29:361-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 83] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts: lessons from a 20 year experience. Arch Dis Child. 1995;73:528-531. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 96] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Kim HJ, Kim MH, Lee SK, Seo DW, Kim YT, Lee DK, Song SY, Roe IH, Kim JH, Chung JB. Normal structure, variations, and anomalies of the pancreaticobiliary ducts of Koreans: a nationwide cooperative prospective study. Gastrointest Endosc. 2002;55:889-896. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg. 1980;140:653-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 321] [Cited by in F6Publishing: 262] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Miyano T, Yamataka A. Choledochal cysts. Curr Opin Pediatr. 1997;9:283-288. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 97] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Ishibashi H, Shimada M, Kamisawa T, Fujii H, Hamada Y, Kubota M, Urushihara N, Endo I, Nio M, Taguchi T, Ando H; Japanese Study Group on Congenital Biliary Dilatation (JSCBD). Japanese clinical practice guidelines for congenital biliary dilatation. J Hepatobiliary Pancreat Sci. 2017;24:1-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 10. | Woo R, Le D, Albanese CT, Kim SS. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoendosc Adv Surg Tech A. 2006;16:179-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Meehan JJ, Elliott S, Sandler A. The robotic approach to complex hepatobiliary anomalies in children: preliminary report. J Pediatr Surg. 2007;42:2110-2114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Akaraviputh T, Trakarnsanga A, Suksamanapun N. Robot-assisted complete excision of choledochal cyst type I, hepaticojejunostomy and extracorporeal Roux-en-y anastomosis: a case report and review literature. World J Surg Oncol. 2010;8:87. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Dawrant MJ, Najmaldin AS, Alizai NK. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children less than 10 kg. J Pediatr Surg. 2010;45:2364-2368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Chang EY, Hong YJ, Chang HK, Oh JT, Han SJ. Lessons and tips from the experience of pediatric robotic choledochal cyst resection. J Laparoendosc Adv Surg Tech A. 2012;22:609-614. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Alizai NK, Dawrant MJ, Najmaldin AS. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr Surg Int. 2014;30:291-294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Wong KY, Lan CL, Liu X, Zhong H, Chen Q, Tan G. Da Vinci robotic system for pediatric surgery: Report of first 20 cases. Chinese Journal of Minimally Invasive Surgery. 2013;13:4-8. [Cited in This Article: ] |
| 17. | Kim NY, Chang EY, Hong YJ, Park S, Kim HY, Bai SJ, Han SJ. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J. 2015;56:737-743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Zhang Q, Cao G, Tang S. Da Vinci Robotic System for choledochal cysts in children. Journal of Clinical Pediatric Surgery. 2016;15:137-139. [Cited in This Article: ] |
| 19. | Kawarada Y, Das BC, Tabata M, Isaji S. Surgical treatment of type IV choledochal cysts. J Hepatobiliary Pancreat Surg. 2009;16:684-687. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Pal K, Singh VP, Mitra DK. Partial hepatectomy and total cyst excision is curative for localized type IV-a biliary duct cysts - report of four cases and review of management. Eur J Pediatr Surg. 2009;19:148-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Zheng X, Gu W, Xia H, Huang X, Liang B, Yang T, Yang S, Zeng J, Dong J. Surgical treatment of type IV-A choledochal cyst in a single institution: children vs. adults. J Pediatr Surg. 2013;48:2061-2066. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | He XD, Wang L, Liu W, Liu Q, Qu Q, Li BL, Hong T. The risk of carcinogenesis in congenital choledochal cyst patients: an analysis of 214 cases. Ann Hepatol. 2014;13:819-826. [PubMed] [Cited in This Article: ] |
| 23. | Kamisawa T, Ando H, Suyama M, Shimada M, Morine Y, Shimada H; Working Committee of Clinical Practice Guidelines for Pancreaticobiliary Maljunction; Japanese Study Group on Pancreaticobiliary Maljunction. Japanese clinical practice guidelines for pancreaticobiliary maljunction. J Gastroenterol. 2012;47:731-759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 24. | Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, Caravaglios G. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777-784. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 749] [Cited by in F6Publishing: 691] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 25. | Sodergren MH, Darzi A. Robotic cancer surgery. Br J Surg. 2013;100:3-4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Herron DM, Marohn M; SAGES-MIRA Robotic Surgery Consensus Group. A consensus document on robotic surgery. Surg Endosc. 2008;22:313-325; discussion 311-312. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 258] [Cited by in F6Publishing: 234] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 27. | Liao G, Chen J, Ren C, Li R, Du S, Xie G, Deng H, Yang K, Yuan Y. Robotic versus open gastrectomy for gastric cancer: a meta-analysis. PLoS One. 2013;8:e81946. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Yang GZ, Kerr K, Darzi A. A special issue on selected papers from the 5th Hamlyn Symposium on Medical Robotics, 2012. J Robot Surg. 2013;7:215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Markar SR, Karthikesalingam AP, Venkat-Ramen V, Kinross J, Ziprin P. Robotic vs. laparoscopic Roux-en-Y gastric bypass in morbidly obese patients: systematic review and pooled analysis. Int J Med Robot. 2011;7:393-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |