Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1990
Peer-review started: January 25, 2024
First decision: February 2, 2024
Revised: February 7, 2024
Accepted: March 15, 2024
Article in press: March 15, 2024
Published online: April 16, 2024
When an anorectal foreign body is found, its composition and shape should be evaluated, and a timely and effective treatment plan should be developed based on the patient's symptoms to avoid serious complications such as intestinal perforation caused by displacement of the foreign body.
A 54-year-old male was admitted to our outpatient clinic on June 3, 2023, due to a rectal foreign body that had been embedded for more than 24 h. The patient reported using a glass electrode tube to assist in the recovery of prolapsed hemorrhoids, however, the electrode tube was inadvertently inserted into the anus and could not be removed by the patient. During hospitalization, the patient underwent surgery, and the foreign body was dragged into the rectum with the aid of colonoscopy. The anus was dilated with a comb-type pulling hook and an anal fistula pulling hook to widen the anus and remove the foreign body, and the local anal symptoms were then relieved with topical drugs. The patient was allowed to eat and drink, and an entire abdominal Computed tomography (CT) and colonoscopy were reviewed 3 d after surgery. CT revealed no foreign body residue and colonoscopy showed no metal or other residues in the colon and rectum, and no apparent intestinal tract damage.
The timeliness and rationality of the surgical and therapeutic options for this patient were based on a literature review of the clinical signs and conceivable conditions in such cases. The type, material and the potential risks of rectal foreign bodies should be considered.
Core Tip: There are various reasons for the embedding of rectal foreign bodies. Depending on the type and shape of the embedded foreign body, timely and appropriate therapeutic measures to avoid intestinal damage caused by the foreign body are the key to effective treatment. We report the case of a patient with an impacted rectal foreign body for more than 24 h. As the embedded foreign body in this patient was a glass tube with metal needles at the end, removal of the foreign body was carried out in conjunction with gastrointestinal endoscopy.
- Citation: Zhou PF, Lu JG, Zhang JD, Wang JW. Colonoscopy-assisted removal of an impaction foreign body at the rectosigmoid junction: A case report. World J Clin Cases 2024; 12(11): 1990-1995
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1990.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1990
Depending on the entry route, foreign bodies can be classified as oral, anal, or endogenous in the gastrointestinal tract[1]. Localized injuries to the gastrointestinal tract caused by foreign bodies most frequently occur in the physiological corners or narrow portions of the gastrointestinal tract and are closely linked to the material, size and sharp edges of the foreign body. The two most prevalent areas are the ileocecal and sigmoid colon[2]. There are numerous sources of intestinal foreign bodies, including, but not limited to, masturbators, fruits, vegetables and glass. Various treatment approaches are required, depending on the composition of the foreign body. A foreign body consisting of soft material, smooth edges, and a small volume can be considered for removal through the anus; fruits and vegetables that are fragile may be extracted via the anus or following decomposition of a larger foreign body[3]. Due to the large size or fragility of glass products, such as wine bottles, these can easily cause damage to the intestinal wall, resulting in more serious complications. Therefore, multiple factors should be considered, including imaging examinations, to ensure patient safety[4].
A 54-year-old male was admitted to our hospital with the chief complaint of "rectal foreign body impaction for more than 24 h".
Rectal foreign body impaction for more than 24 h, was accompanied by difficulty in defecation, low stool volume, bloody stools, and a small amount of red blood discharged from the anus.
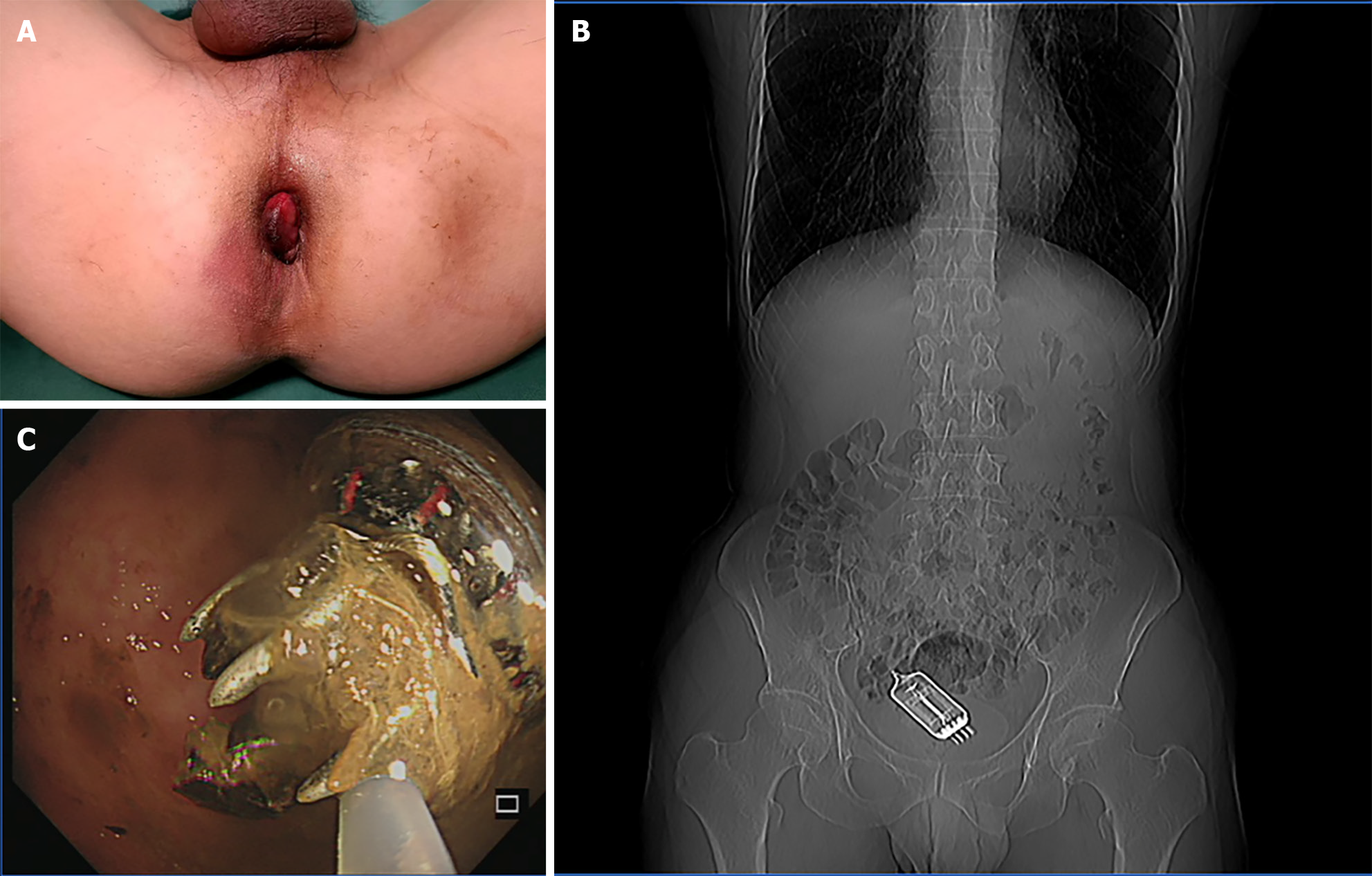
The patient reported that 24 h previously, due to prolapsed hemorrhoids (Figure 1A), he used an electrode tube for assisted reduction and inadvertently inserted the electrode tube into the anus, which could not be removed. He then used vascular forceps to clamp it, which could not be removed either. Moreover, according to the results of computed tomography (CT) in another hospital (not reported), the foreign body had reached the sigmoid colon, and the patient was unable to remove it following oral lactulose and enemas.
The patient denied any family history of disease.
On physical examination, his vital signs were as follows: Temperature: 36.8 °C, pulse: 75 bpm, respiration: 15 breaths/min, blood pressure: 120/80 mmHg. The patient was conscious and cooperative. Pain associated with lower abdominal pressure, rebound pain, muscle tension, and mobile turbid sounds were negative.
Laboratory tests on admission showed the following: White blood cells: 8.23 109/L, hemoglobin: 136 g/L, platelets: 207 109/L, and C-reactive protein: 26.71 ng/L.
A CT of the entire abdomen (Figure 1B) revealed an elliptical, cylindrical, metal-dense foreign body in the rectum measuring approximately 3 cm in diameter and 5.8 cm in length.
The final diagnosis in the patient was foreign body impaction at the rectosigmoid junction.
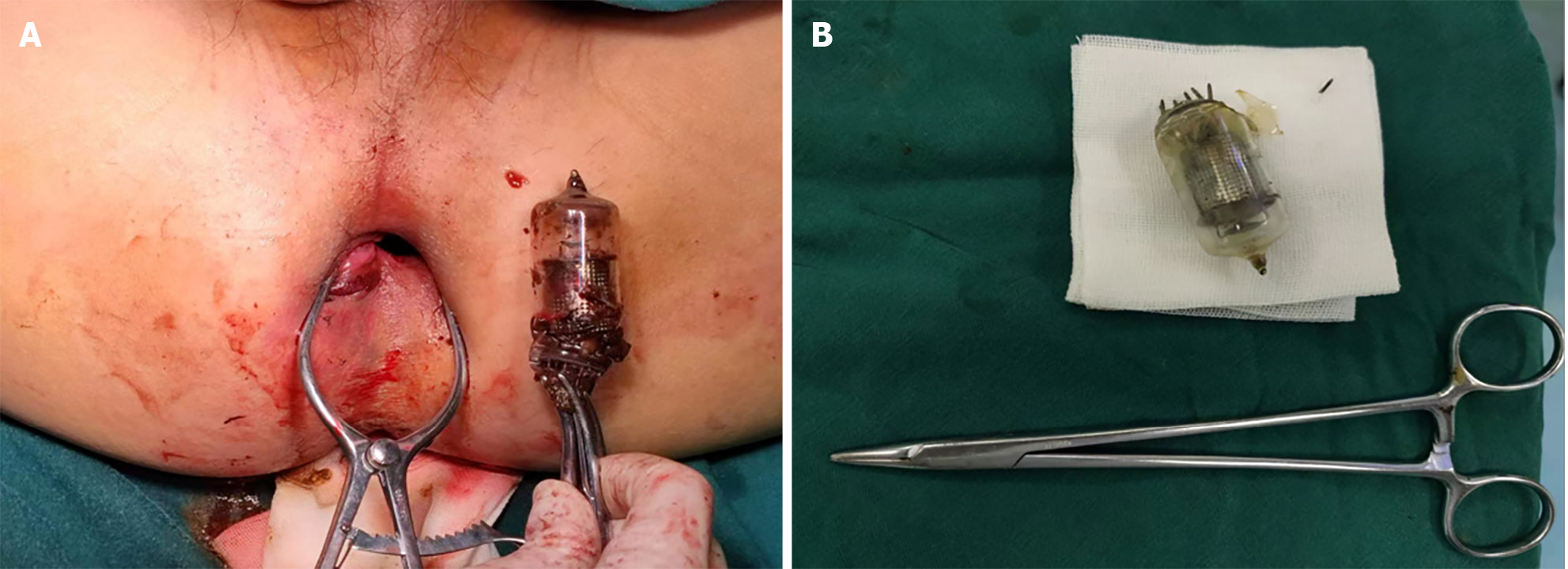
Rectal foreign body removal was performed under subarachnoid block anesthesia in the operating room. After anesthesia induction, colonoscopy-assisted removal of the foreign body was attempted as finger examination and surgical instruments were unable to reach the foreign body, and gastrointestinal endoscopy revealed that the foreign body had shifted position and was located at the recto sigmoid junction (Figure 1C). The foreign body was characterized by a glass cylinder with metal spikes at the bottom (Figure 2A), and attempts to remove it using a foreign body net pocket during colonoscopy were unsuccessful. After using a ring lasso device and other aids, the foreign body was dragged to the anal canal. After expansion of the anus using comb-type hooks and anal fistula hooks, finger expansion was performed. Subsequently, curved vascular pliers were used to clamp the bottom of the foreign body, which contained metal needles, to facilitate removal of the object from the anus (Figure 2B).
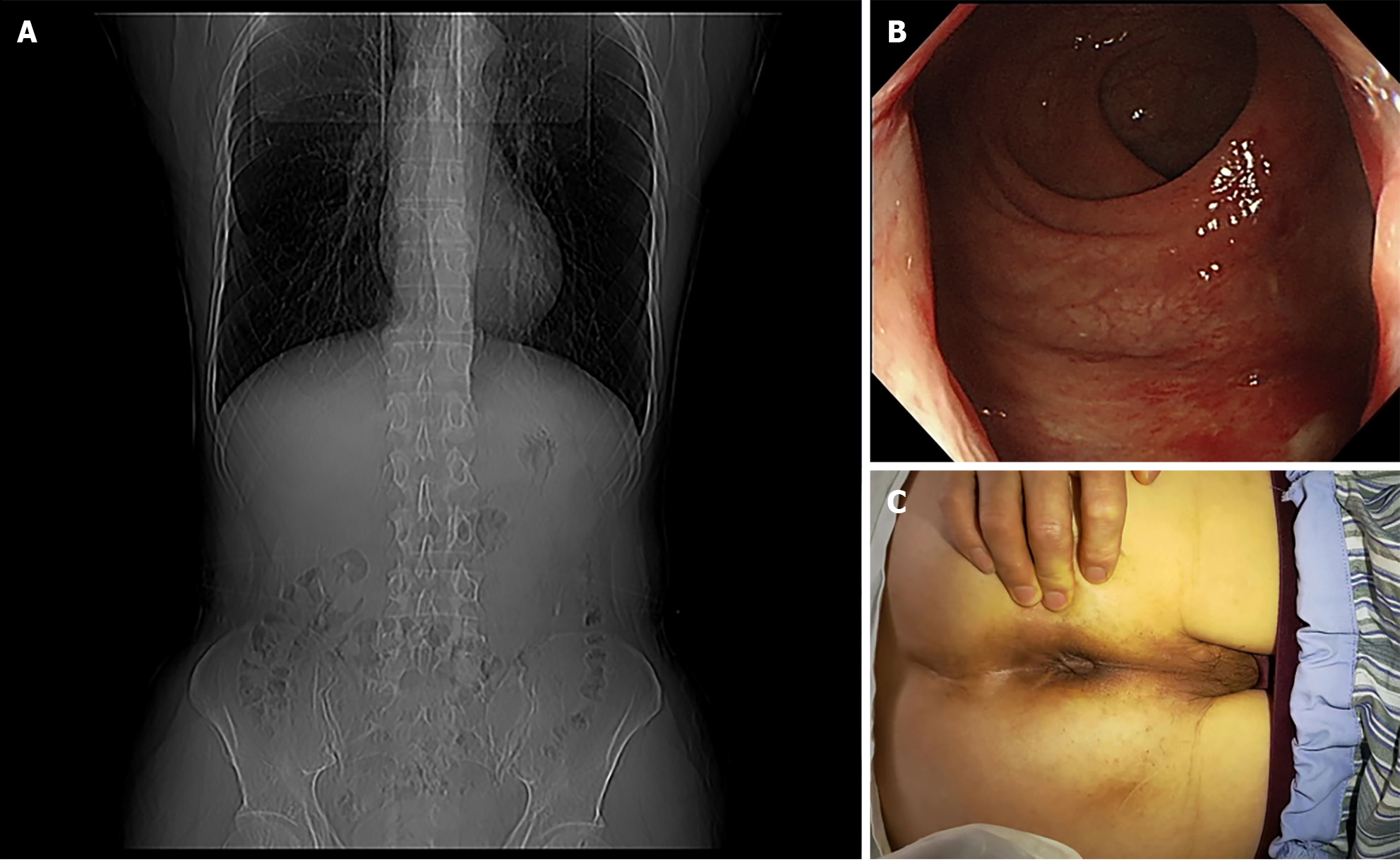
The patient was allowed to eat and drink, and an entire abdominal CT (Figure 3A) and colonoscopy (Figure 3B) were reviewed 3 d after surgery. The CT revealed no foreign body residue, and colonoscopy showed no metal or other residues in the colon and rectum, and no apparent intestinal tract damage. 3 d after surgery, the symptoms of internal prolapsed hemorrhoids disappeared (Figure 3C). And this work has been reported in line with the Surgical case report criteria[5].
The incidence of rectal foreign bodies is approximately 15 per 10000000 individuals[6]. Approximately 20% of rectal foreign bodies are initially masked by different complaints, such as pain, hemorrhage, or constipation, and are undetected until additional inquiries are made regarding the cause of the condition[7]. For example, in the case reported by Husain et al[8], the patient mainly presented with abdominal pain, and it was only discovered by chest CT that a perforation of the large intestine had been caused by a fishbone. Unlike Raja Husain's case where foreign bodies entered through the mouth, in this case, the foreign body entered through the anus, providing us with a basis for diagnosis and treatment. Rectal foreign bodies are an urgent and challenging issue for emergency physicians and anorectal surgeons. Patients may be admitted to the hospital and report abdominal discomfort to their attending physicians. Moreover, there is a tendency to conceal the cause of abdominal pain, and the presence of abdominal pain due to a rectal foreign body is given less consideration by physicians. Often, bowel function is preserved despite the patient's abdominal discomfort and inability to defecate, which is one of the reasons why some physicians consider it an intestinal obstruction[8]. Rectal foreign bodies may be caused by sexual gratification, mental illness, physical assault, or surgical procedures[9]. The foreign body location is not limited to the rectum; however, in severe cases, it can result in tissue or organ injury, with complications including mucosal lacerations, foreign body migration to areas adjacent to the bowel, intestinal obstruction, perforation, peritonitis, and septicemia[10]. Yildiz et al[10] analyzed 30 patients with foreign bodies and found that 90% of patients complained of perianal pain, while 70% complained of abdominal pain. Consequently, the patient, in this instance, was hospitalized and fully informed of the patient's right to information prior to surgery, including the risks of the surgical process. The case reported by Simbila et al[11] was a male patient who inserted a lubricated plastic detergent bottle into the anus for sexual satisfaction, causing a 10 cm tear and perforation from the rectum to the sigmoid colon. Therefore, the patient underwent colostomy. In our case, during the treatment process, we adopted timely and effective treatment measures, which combined imaging, digestive endoscopy, and anorectal surgery, to select the most appropriate treatment and resolve the foreign body implantation issue.
Rectal foreign bodies and their effects on localized colorectal tissue necessitate systematic evaluation to develop treatment plans. In order to provid a more rational approach, the specific patient's condition in conjunction with a comprehensive physical and digital examination along with abdominal imaging, such as X-rays, and CT scans should be considered, to aid in the assessment and localization of the foreign body, as well as ancillary investigations to determine whether it is possible to attempt manual grasping of the object or endoscopic removal[12]. According to the literature[13], the success rate of removing foreign bodies at the bedside and in the emergency room is 16%-75%. Repeated attempts to remove foreign objects can lead to pain and severe involuntary intestinal spasms, which is one of the reasons for removal failure[14]. In this case, the patient used oral lactose and enemas, but failed to remove the foreign body, which resulted in its movement upward through the anus, and it eventually stopped at the junction of the rectum and sigmoid colon. If physical examination or imaging reveals peritonitis or perforation, surgical intervention should be considered immediately[15]. According to reports, 67% of rectal foreign body injuries do not penetrate the entire length of the rectal wall and thus do not necessitate surgical intervention. When the entire rectal wall is damaged, surgical intervention becomes more difficult, and peritoneal involvement may exacerbate the condition[16]. To minimize the complexity of removing a rectal foreign body, it is important to consider the shape, size, and composition of the object. Depending on the characteristics of the foreign body, methods such as sigmoidoscopy, endoscopy, or Foley catheters can be considered[17].
In this case, the embedded foreign body was composed of glass with spiny protrusions, and the location was too high for bedside removal. Therefore, the patient agreed to undergo colonoscopy. Simultaneously, due to the specificity of the embedded foreign body, for industrial diodes, glass products, first and foremost, have the risk of breaking, and once broken, will cause damage to the patient's intestinal lumen, not only increasing the difficulty of the operation but also placing the patient's life in jeopardy. In addition, due to the uncertainty of whether the diode's interior and exterior contain heavy metals and other uncertain materials, and whether it will cause toxicity, there is also a degree of surgical uncertainty; therefore, timely and effective removal of the foreign body is essential. The drawback in this case is that we did not have a more suitable tool to remove the foreign body, which caused damage to the glass when paired with a colonoscope hook. This poses a hidden danger in this type of surgery. However, subsequent observations revealed that this did not lead to other concurrent symptoms. Due to the timely management of this patient, the foreign body was successfully removed. Therefore, in the future, it is necessary to have a suitable surgical plan and surgical tool when dealing with similar clinical cases. The foreign body embedded in the rectum, in this case, was composed of glass, which is easily damaged. Consequently, violent removal should not be conducted during the surgical process to avoid glass breakage, which may injure the intestine.
We thank our colleagues for assistance in reviewing this manuscript. We would especially like to thank Dr. Shi Bei and his assistants at the Endoscopy Center for all their help.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Grawish ME, Egypt S-Editor: Liu H L-Editor: A P-Editor: Yu HG
| 1. | Coskun A, Erkan N, Yakan S, Yıldirim M, Cengiz F. Management of rectal foreign bodies. World J Emerg Surg. 2013;8:11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Gash KJ, Suradkar K, Kiran RP. Rectal trauma injuries: outcomes from the U.S. National Trauma Data Bank. Tech Coloproctol. 2018;22:847-855. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Goldberg JE, Steele SR. Rectal foreign bodies. Surg Clin North Am. 2010;90:173-184, Table of Contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Lodhia J, Msuya D, Chilonga K, Makanga D. Successful Transabdominal Removal of Penetrating Iron Rod in the Rectum: A Case Report. East Afr Health Res J. 2021;5:137-141. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 5. | Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA; Collaborators. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg. 2023;109:1136-1140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 674] [Article Influence: 674.0] [Reference Citation Analysis (0)] |
| 6. | Cawich SO, Thomas DA, Mohammed F, Bobb NJ, Williams D, Naraynsingh V. A Management Algorithm for Retained Rectal Foreign Bodies. Am J Mens Health. 2017;11:684-692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Ploner M, Gardetto A, Ploner F, Scharl M, Shoap S, Bäcker HC. Foreign rectal body - Systematic review and meta-analysis. Acta Gastroenterol Belg. 2020;83:61-65. [PubMed] [Cited in This Article: ] |
| 8. | Husain R, Alghamdi DA, Ghzoi FA, AlArafah SK, Bahammam MA, Al Duhileb M. Conservative management of fish bone-induced large bowel perforation: Case report. Int J Surg Case Rep. 2022;95:107157. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 9. | Caliskan C, Makay O, Firat O, Can Karaca A, Akgun E, Korkut MA. Foreign bodies in the rectum: an analysis of 30 patients. Surg Today. 2011;41:795-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Yildiz SY, Kendirci M, Akbulut S, Ciftci A, Turgut HT, Hengirmen S. Colorectal emergencies associated with penetrating or retained foreign bodies. World J Emerg Surg. 2013;8:25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Simbila AN, Suphian A, Ngowi NJ, Mfinanga RJ, Kilindimo S, Sawe HR. Colon perforation by foreign body insertion for sexual gratification: a case report. Pan Afr Med J. 2021;40:188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 12. | Pinto A, Miele V, Pinto F, Mizio VD, Panico MR, Muzj C, Romano L. Rectal foreign bodies: imaging assessment and medicolegal aspects. Semin Ultrasound CT MR. 2015;36:88-93. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Clarke DL, Buccimazza I, Anderson FA, Thomson SR. Colorectal foreign bodies. Colorectal Dis. 2005;7:98-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Huang WC, Jiang JK, Wang HS, Yang SH, Chen WS, Lin TC, Lin JK. Retained rectal foreign bodies. J Chin Med Assoc. 2003;66:607-612. [PubMed] [Cited in This Article: ] |
| 15. | Koornstra JJ, Weersma RK. Management of rectal foreign bodies: description of a new technique and clinical practice guidelines. World J Gastroenterol. 2008;14:4403-4406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 52] [Cited by in F6Publishing: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Schellenberg M, Brown CVR, Trust MD, Sharpe JP, Musonza T, Holcomb J, Bui E, Bruns B, Hopper HA, Truitt MS, Burlew CC, Inaba K, Sava J, Vanhorn J, Eastridge B, Cross AM, Vasak R, Vercuysse G, Curtis EE, Haan J, Coimbra R, Bohan P, Gale S, Bendix PG; AAST Contemporary Management of Rectal Injuries Study Group. Rectal Injury After Foreign Body Insertion: Secondary Analysis From the AAST Contemporary Management of Rectal Injuries Study Group. J Surg Res. 2020;247:541-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Lefcourt T, Ku A, Issagholian L, Neeki AS, Retamozo M, Dong F, Neeki MM. Novel Bedside Utilization of Foley Catheter in the Emergent Removal of Colorectal Foreign Body: A Case Report and Literature Review. Cureus. 2021;13:e20217. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |