Published online Jan 6, 2024. doi: 10.12998/wjcc.v12.i1.210
Peer-review started: October 31, 2023
First decision: November 9, 2023
Revised: November 22, 2023
Accepted: December 15, 2023
Article in press: December 15, 2023
Published online: January 6, 2024
Intestinal malrotation is a congenital defect of embryonic development caused by various teratogenic factors. In this condition, the intestinal tube, along with the superior mesenteric artery serving as the axis for the counterclockwise movement, is incomplete or abnormally rotated due to incomplete attachment of the mesentery and abnormal intestinal tube position. Such a case is usually asymp
An elderly male patient was admitted to the hospital due to gastric cancer. An abdominal computed tomography (CT) scan with contrast revealed that the ascending and descending colon were parallel on the right side of the abdominal cavity, while the sigmoid colon extended into the right iliac fossa, allowing the diagnosis of congenital midgut malrotation. Following thorough preoperative preparation, the patient underwent laparoscopic radical gastrectomy to treat his gastric cancer. Intraoperatively, an exploration of the abdominal cavity uncovered the absence of the transverse colon. The distal colon at the hepatic flexure, along with the ascending colon, extended into the right iliac fossa, where it continued as the sigmoid colon. As planned, the laparoscopic radical gastrectomy was perform
Asymptomatic intestinal malrotation is best detected by CT, requiring no treatment but possibly interfering with the treatment of other diseases.
Core Tip: Intestinal malrotation is a congenital defect that often goes unnoticed, lacks clinical symptoms, and can complicate the management of other abdominal conditions. Surgeons must recognize the potential presence of intestinal malrotation to adjust their approach effectively during abdominal surgery.
- Citation: Jia XH, Kong S, Gao XX, Cong BC, Zheng CN. Intestinal malrotation complicated with gastric cancer: A case report. World J Clin Cases 2024; 12(1): 210-216
- URL: https://www.wjgnet.com/2307-8960/full/v12/i1/210.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i1.210
Intestinal malrotation is a malformation of the digestive tract resulting from the abnormal counterclockwise rotation of the midgut around the axis of the superior mesenteric artery during embryonic development. Genetic factors, intrauterine developmental abnormalities, and adverse environmental conditions may disrupt the normal rotation of the midgut. This results in positional variations of the intestinal tube and abnormalities in mesenteric attachment[1]. Previous studies on intestinal malrotation typically described cases where the jejunum and ileum are located on the right side of the abdominal cavity while the colon is on the left side. This paper presents a case characterized by the absence of the transverse colon, the presence of the right-sided descending and sigmoid colon, and the coexistence of a malignant tumor in the gastric antrum. Such a combination is exceedingly rare in the context of intestinal rotation cases.
A 70-year-old male patient, who was diagnosed with gastric cancer 4 d ago, was admitted to the hospital with a chief complaint of epigastric pain for 3 mo.
The patient presented with abdominal pain, requiring gastroscopy. The pathology revealed adenocarcinoma in the gastric antrum, prompting the patient to seek surgical intervention at the hospital.
The patient underwent urolithotomy > 60 years ago.
He has no family history of related diseases or any other hereditary conditions.
The abdomen appeared flat without tenderness, rebound pain, or muscle tension. The tympanic sound was heard on percussion, and there were no signs of displaced fluid or turbidity. Bowel sounds were observed at a rate of 3-5 beats per minute.
All laboratory tests were within normal limits.
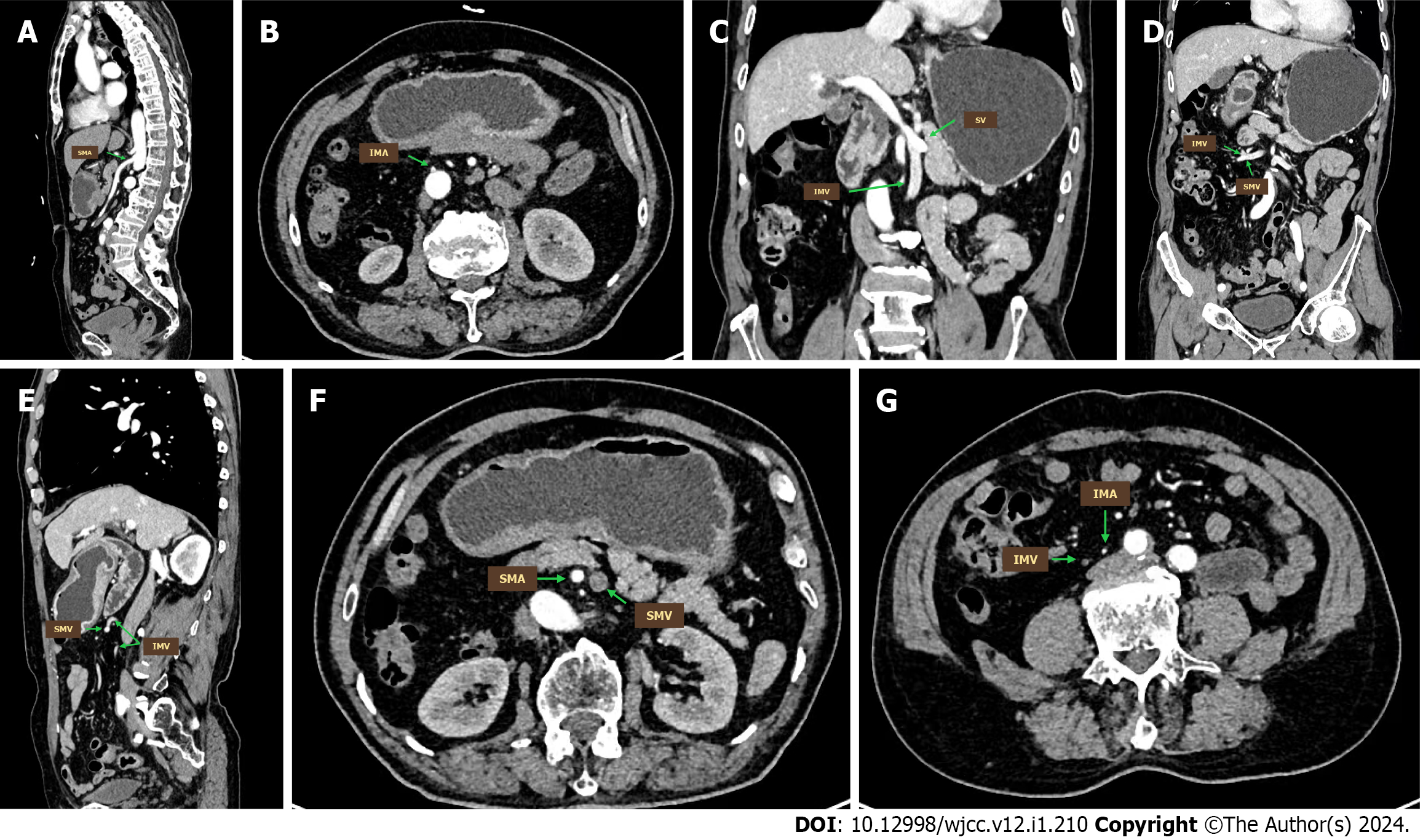
Abdominal computed tomography (CT) with contrast showed gastric antrum cancer and perigastric lymph node metastasis. As shown in Figure 1, the distal colon at the hepatic flexure was accompanied by the ascending colon in the right iliac fossa and continued as the sigmoid colon. The jejuno-ileum was located mainly on the left side of the abdomen. The superior mesenteric artery originated from the abdominal aorta at the level of the first lumbar vertebra (Figure 2A), supplying most of the jejunoileum on the left and the terminal ileum, the ascending colon, and part of the descending colon on the right. The abdominal aorta branched into the inferior mesenteric artery inferiorly to the right at the level of the second lumbar vertebra to supply a portion of the descending colon, the sigmoid colon, and a portion of the rectum (Figure 2B).
Regarding the venous course, the splenic vein joined the superior mesenteric vein in the portal vein from the left at the level of the first lumbar vertebra (Figure 2C). The inferior mesenteric vein joined the superior mesenteric vein on the right side at the level of the third and fourth lumbar vertebrae (Figure 2D and E). As a result of mesenteric malrotation, the position of superior and inferior mesenteric vessels was altered (Figure 2F and G).
The patient was thus diagnosed with a malignant tumor of the gastric sinus and intestinal malrotation.
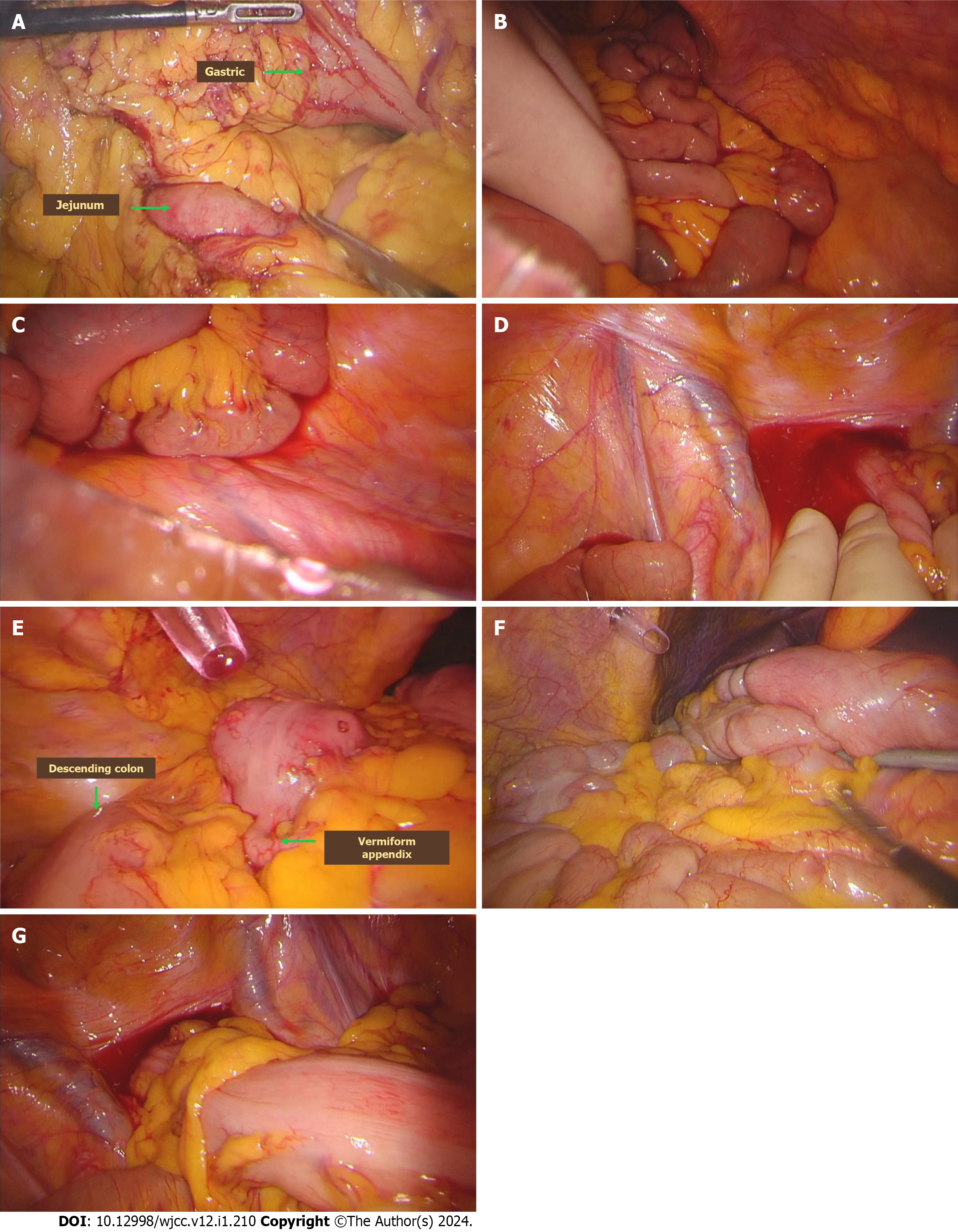
As shown in Figure 3, laparoscopic radical gastrectomy was performed as planned without addressing the issue of intestinal malrotation.
The patient was discharged after seven days of postoperative hospitalization with satisfactory recovery.
Intestinal malrotation is a congenital defect of embryonic development. Normally, from the 6th wk of embryonic development, the midgut loop rotates 90° counterclockwise on the axis of the superior mesenteric artery, turning the structures from a sagittal to a horizontal position. In the 10th wk, the intestinal collaterals return to the abdominal cavity from the umbilical cavity and continue to rotate counterclockwise by 180°, with the cephalic branch shifting to the left and the caudal branch shifting to the right, positioning the jejunum and ileum in the middle of the abdominal cavity. The cecum protrudes initially under the liver and then descends to the right iliac fossa as the ascending colon forms. The caudal segment of the descending colon moves to the midline to form the sigmoid colon. Abnormalities in any of the above-mentioned processes can lead to the malposition of the bowel and mesenteric vessels[2].
In this case, only the ascending colon had normal alignment. The transverse colon was absent, the distal and ascending colon traveled to the right iliac fossa and continued as the sigmoid colon. Hence, the entire colon was located on the right side of the abdominal cavity, which might be caused by the return of the head branch of the mesenteric collaterals to the abdominal cavity in the 10th wk of embryonic development. Thus, the posterior bowel was not pushed to the left side but instead was pushed to the right side to form a right-sided descending and sigmoid colon. The rotation of the ascending colon formed by the caudal branch of the midgut was basically normal; therefore, the ascending and descending colon converged directly in the hepatic flexure, and the transverse colon was absent, an extremely rare case not reported in the literature.
Intestinal malrotation can manifest at any age, with abdominal pain and vomiting being the most prevalent clinical symptoms, occurring in approximately 50% of patients during initial presentation[3]. In infants and children, symptoms tend to be more severe in the early stages, facilitating prompt diagnosis and treatment. Conversely, adults may expe
Diagnosing intestinal malrotation can be accomplished through various methods, including imaging of the entire digestive tract with barium, barium enema of the colon, abdominal CT, and mesenteric angiography. Among these methods, abdominal CT offers certain advantages. It not only reveals the distribution of the intestinal tract and the perfusion of the intestinal wall in multiple planes and dimensions but also allows for an assessment of the anatomy, such as the proximity of the intestinal tract and its mesentery to neighboring organs. Some studies suggested that abdominal CT is the preferred diagnostic method for suspected intestinal malrotation in adults[5,6]. Specifically, the presence of the whirl-like pattern and the transposition of the superior mesenteric artery and vein on abdominal CT indicate intestinal malrotation[7].
Xiong et al[8] classified intestinal malrotation into ten categories based on positional variations of three common anatomical landmarks (duodenum, jejunum, and cecum) observed on CT images. However, the current case did not align with any of these established categories. The Ladd procedure is the established treatment for symptomatic patients with midgut malrotation. It can be performed either through open or laparoscopic surgery and is beneficial for the majority of patients[9]. However, the necessity of surgical treatment for asymptomatic patients remains controversial. Choi et al[10] conducted a review studying 177 patients over 35 years, suggesting that asymptomatic patients face a low risk of adverse events and do not require specific treatment. In contrast, some scholars argue that all patients diagnosed with intestinal malrotation should undergo surgical treatment, irrespective of whether they have symptoms[11].
The patient in this case was admitted to the hospital due to gastric cancer. Both preoperative CT and intraoperative inspection identified congenital intestinal malrotation. As the patient’s colonic deformity remained asymptomatic, laparoscopic radical gastrectomy was performed as planned. However, the absence of the transverse colon and gastrocolic ligament presented challenges during the operation, particularly in the dissection of the greater curvature of the stomach and the identification and ligation of the gastroepiploic vessels. In summary, asymptomatic intestinal malrotation does not require clinical intervention. However, its associated anatomical variations can impact other surgical procedures. Therefore, conducting preoperative CT scan and other relevant examinations to identify these variations in advance is crucial for ensuring a successful surgical outcome.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kotelevets SM, Russia; Yang H, China S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Haak BW, Bodewitz ST, Kuijper CF, de Widt-Levert LM. Intestinal malrotation and volvulus in adult life. Int J Surg Case Rep. 2014;5:259-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Grand RJ, Watkins JB, Tortu FM. Development of the Human Gastrointestinal Tract: A Review. Gastroenterology. 1976;70:790-810. [DOI] [Cited in This Article: ] |
| 3. | Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery. 2011;149:386-393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 107] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Anand U, Kumar R, Priyadarshi RN, Kumar B, Kumar S, Singh VP. Comparative study of intestinal malrotation in infant, children, and adult in a tertiary care center in India. Indian J Gastroenterol. 2018;37:545-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM. Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg. 2008;206:658-663. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Kotobi H, Tan V, Lefèvre J, Duramé F, Audry G, Parc Y. Total midgut volvulus in adults with intestinal malrotation. Report of eleven patients. J Visc Surg. 2017;154:175-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Neville JJ, Sharma E, Al-Muzrakchi A, Sheth H. Congenital intestinal malrotation presenting in octogenarians: a report of two cases. Ann R Coll Surg Engl. 2020;102:e12-e14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Xiong Z, Shen Y, Morelli JN, Li Z, Hu X, Hu D. CT facilitates improved diagnosis of adult intestinal malrotation: a 7-year retrospective study based on 332 cases. Insights Imaging. 2021;12:58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Fu T, Tong WD, He YJ, Wen YY, Luo DL, Liu BH. Surgical management of intestinal malrotation in adults. World J Surg. 2007;31:1797-1803. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Choi M, Borenstein SH, Hornberger L, Langer JC. Heterotaxia syndrome: the role of screening for intestinal rotation abnormalities. Arch Dis Child. 2005;90:813-815. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Cheikhelard A, De Lagausie P, Garel C, Maintenant J, Vuillard E, Blot P, Aigrain Y. Situs inversus and bowel malrotation: contribution of prenatal diagnosis and laparoscopy. J Pediatr Surg. 2000;35:1217-1219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |