Copyright
©The Author(s) 2023.
World J Clin Cases. Jul 6, 2023; 11(19): 4713-4722
Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4713
Published online Jul 6, 2023. doi: 10.12998/wjcc.v11.i19.4713
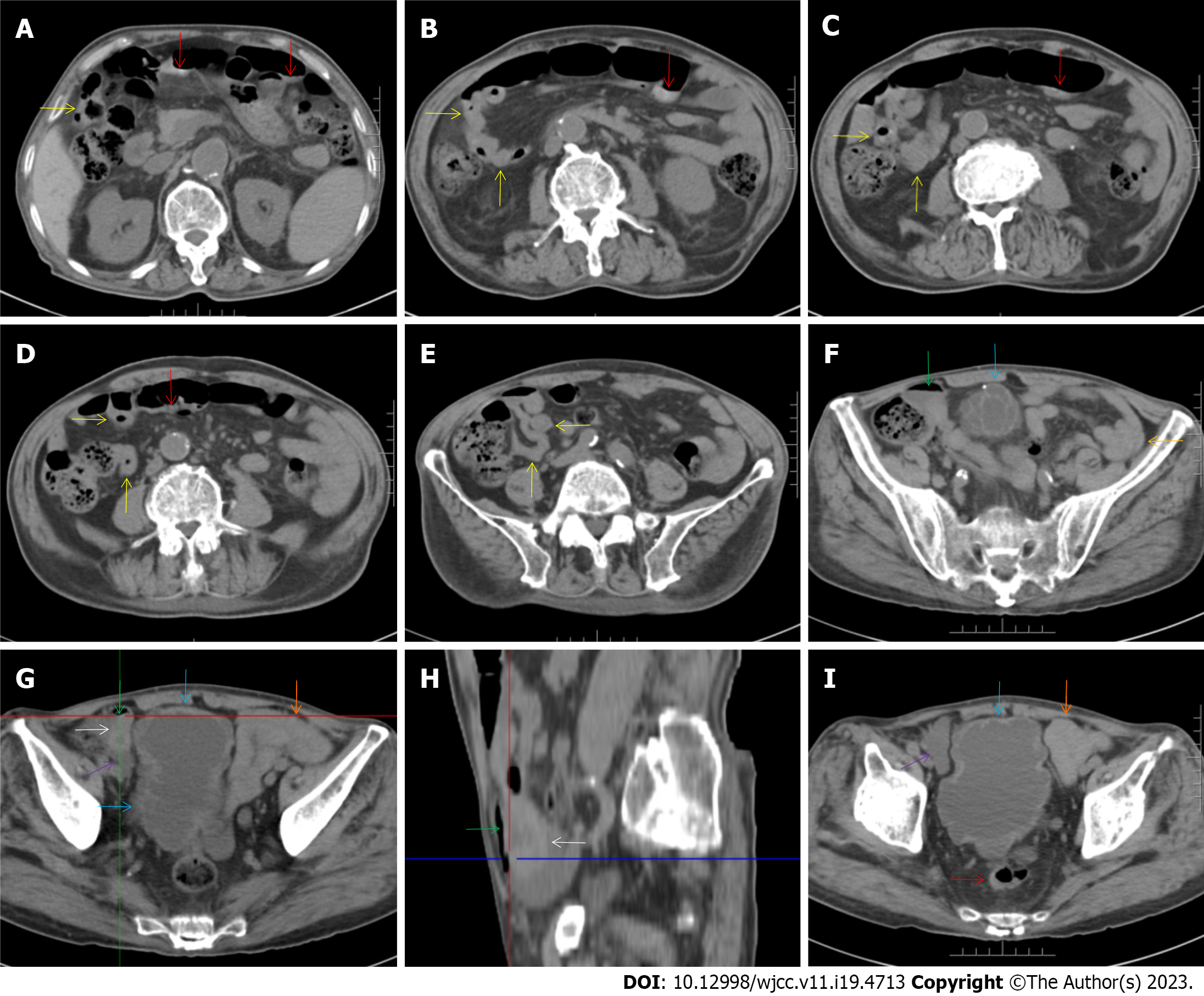
Figure 3 Abdominal computed tomography during aplastic crisis.
A-E: The wall of the distal ileum was hypertrophically thickened and adhered, and the lumen of the terminal ileum was collapsed (yellow arrow). The lumen of the proximal small intestine was filled with liquid, with several gas—liquid levels. Hypertrophic lesions were also present in several segments of the colon (red arrows), and the lumen of the colon was dilated. In other segments of the colon, the wall showed fibrotic thickening. Notably, panabdominal silt-like fat proliferation led to widening of the bowel loop, forming the so-called “creeping fat sign” and indicating the presence of active chronic gut inflammatory conditions in the small intestine; F-I: In the right iliac fossa, there was an effusive lesion (purple arrow), indicative of peritoneal involvement. A gas—liquid level was present in the distal ileum (green arrows), proximal to which the ileal wall showed hypertrophic thickening (white arrows). The wall of the bladder also showed hypertrophic thickening, with an exudative lesion outside of the hypertrophic bladder wall (blue arrows). An adhered bowel loop was present in the proximal ileum (orange arrows), with the fibrotic thickening of the peritoneum forming the so-called “abdominal cocoon”. These imaging features, together with the imaging features on chest computed tomography, suggested a diagnosis of tuberculosis infection involving the gastrointestinal tract, peritoneum and urinary tract.
- Citation: Sun XY, Yang XD, Xu J, Xiu NN, Ju B, Zhao XC. Tuberculosis-induced aplastic crisis and atypical lymphocyte expansion in advanced myelodysplastic syndrome: A case report and review of literature. World J Clin Cases 2023; 11(19): 4713-4722
- URL: https://www.wjgnet.com/2307-8960/full/v11/i19/4713.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i19.4713