Published online Jan 6, 2023. doi: 10.12998/wjcc.v11.i1.116
Peer-review started: September 23, 2022
First decision: November 11, 2022
Revised: November 24, 2022
Accepted: December 21, 2022
Article in press: December 21, 2022
Published online: January 6, 2023
Although the number of patients who need central venous ports for permanent vascular access is increasing, there is still no “gold standard” for the implantation technique.
To identify the implantation technique that should be favored.
Two hundred central venous port-implanted patients in a tertiary hospital were retrospectively evaluated. Patients were assigned into two groups according to the access method. The first group comprised patients whose jugular veins were used, and the second group comprised patients whose subclavian veins were used. Groups were evaluated regarding age, sex, application side, primary diagnosis, active follow-up period in the hospital, chemotherapy agents administered, number of complications, and the Clavien-Dindo severity score. The distribution of the variables was tested with the Kolmogorov-Smirnov test and the Mann-Whitney U test. The χ2 test was used to analyze the variables.
There was no statistically significant difference between the groups regarding age, sex, side, number of chemotherapy drugs, and duration of port usage (P > 0.05). Only 2 patients in group 1 had complications, whereas in group 2 we observed 19 patients with complications (P < 0.05). No port occlusion was found in group 1, but the catheters of 4 patients were occluded in group 2. One port was infected in group 1 compared to three infected ports in group 2. Two port ruptures, two pneumothorax, one revision due to a mechanical problem, one tachyarrhythmia during implantation, and four suture line problems were also recorded in group 2 patients. We also showed that it would be sufficient to evaluate and wash ports once every 2 mo.
Our results robustly confirm that the jugular vein route is safer than the subclavian vein approach for central venous port implantation.
Core Tip: A total of 200 consecutive patients who had undergone central venous port implantation were assigned to two groups according to the access method: Jugular or subclavian veins. Our results firmly showed that the port occlusion rate was higher in the subclavian group. The jugular vein approach was also safer regarding port infections, fractures and pneumothorax risk. Contrary to the literature, our study also advocates a longer 2-mo interval for port care and washing. Our results set forth that the jugular vein route is safer than the subclavian vein for central venous port implantation.
- Citation: Erdemir A, Rasa HK. Impact of central venous port implantation method and access choice on outcomes. World J Clin Cases 2023; 11(1): 116-126
- URL: https://www.wjgnet.com/2307-8960/full/v11/i1/116.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i1.116
The number of patients needing permanent and safe vascular access is gradually increasing. Central venous ports are frequently used devices to meet this requirement, and the number of patients in whom ports are implanted is rising[1]. Venous ports, the use of which has begun for systemic treatment of cancer patients, are currently used for various purposes, including parenteral nutrition, stem cell transplantation, apheresis, and pain therapy. Ports enable the administration of all parenteral medical treatments safely and comfortably for patients with vascular access problems. Venous ports may also improve the quality of life of patients who need frequent blood transfusions[2]. The system is composed of a reservoir and a cannula. While one end of the cannula is placed within a major venous structure, the other is connected to the reservoir that is placed subcutaneously through a sealing ring. Hence, we have a closed system located subcutaneously that enables us to reach a major vascular structure. Although there are different techniques for implantation, percutaneous methods and the jugular or subclavian vein routes are the most commonly preferred approaches and the procedure can be performed safely and efficiently under ultrasonographic guidance[3,4]. In a meta-analysis comparing these two leading options, it was shown that there was no difference between the two in terms of catheter-related infection and thrombotic events[5]. It was observed that catheter dislocation and malfunction occurred more frequently in the subclavian route, but there was no difference between the groups regarding port fracture. Ultimately, this meta-analysis, which involved 12 studies and 3905 patients, indicated that the internal jugular vein is a safer route than the subclavian vein and that significant mechanical problems such as dislocation and malfunction are less common with it.
In this study, we retrospectively evaluated 200 patients with venous ports implanted through the jugular vein or subclavian vein. Besides the demographic characteristics of patients, the main focus of this study was to compare the complication risks of these methods to determine the method of choice for central venous port implantation.
Two hundred central venous port-implanted patients were retrospectively evaluated. All procedures were performed by two experienced senior surgeons of the General Surgery Department, and patients were assigned to two groups according to the access method. Group 1 comprised patients whose jugular veins were used, and group 2 comprised patients whose subclavian veins were used.
Groups were evaluated regarding age, sex, application side, primary diagnosis, active follow-up period in the hospital, chemotherapy agents administered, number of complications, and the Clavien-Dindo severity score. Patients were hospitalized in the same-day surgery unit. Procedures were performed in the operating room under local anesthesia and sedation. We used a single-channel silicone 7F port catheter (PolistTM 3000 Series Mini Ports; Vygon Ltd, Wiltshire, United Kingdom).
Group 1: The jugular vein was visualized by ultrasonography and compressed to confirm the location and absence of a thrombus. After an ultrasonography-guided vein puncture, the guidewire was advanced to the atriocaval area. The position was confirmed by fluoroscopy, and then the sheath and the guide were advanced over the guidewire. After it was ascertained that the guide and the sheath were in the vessel, the sheath was advanced. Then, the guide and the guidewire were withdrawn. The catheter advanced through the sheath, and the sheath was removed. To place the port in the subcutaneous space, we made a 2-cm transverse incision at the anterior chest wall and prepared the cavity with electrocautery dissection. The rigid wire of the set was used to connect the tip of the catheter to the port. It was then inserted through the cavity and advanced from a subcutaneous tunnel to the puncture site. The catheter, which was attached to the end of the rigid wire, was pulled into the cavity through this subcutaneous tunnel. The position of the port and the distal end of the catheter was confirmed by fluoroscopy. After those controls, the proximal end of the catheter was shortened and attached to the venous port. After the attachment, the port was placed into the pre-prepared space and fixed with interrupted sutures. Subcutaneous tissues were approximated with interrupted sutures, and the skin was closed with subcuticular sutures.
Group 2: The subclavian vein puncture was performed from the one-third medial part of the clavicle by targeting the jugular notch under the same circumstances. All the stages after the puncture were completed in the same manner as in group 1.
Follow-up: Patients were followed-up at the same-day surgery unit for at least 2 h. Within this period, education for venous port care and terms of use were also repeated. At a convenient time, patients were discharged to be followed up at the outpatient clinic. According to our clinical protocol, each patient’s venous port is evaluated and washed with 1000 U heparin every 2 mo.
The descriptive statistics were given as mean, standard deviation, median, minimum, maximum, frequency, and ratio values. The distribution of the variables was tested with the Kolmogorov-Smirnov test. The Mann-Whitney U test was used to analyze the quantitative independent variables, and the χ2 test was used to analyze the qualitative independent variables. The analyses were performed using the SPSS 27.0 program (IBM Corp., Armonk, NY, United States).
A total of 200 consecutive patients who had undergone central venous port implantations were evaluated in our study (Table 1).
| Characteristic | Parameters | n (%) |
| Age | Min-max: 20-84 | 200 (100) |
| Median: 62 | ||
| mean ± SD: 59.6 ± 12.1 | ||
| Duration of port use in mo | Min-max: 0-93 | 200 (100) |
| Median: 8 | ||
| mean ± SD: 13.5 ± 15.7 | ||
| Sex | Female | 99 (49.5) |
| Male | 101 (50.5) | |
| Side | Right | 186 (93.0) |
| Left | 14 (7.0) | |
| Number of chemotherapeutic drug(s) | 1 | 87 (43.5) |
| 2 | 83 (41.5) | |
| 3 | 30 (15.0) | |
| Complication | Present | 20 (10) |
| Absent | 180 (90) | |
| Clavien-Dindo severity classification | 0-I | 179 (89.5) |
| II | 7 (3.5) | |
| III | 14 (7.0) |
Group 1 included 57 male and 43 female patients; a total of 56 were international and came from abroad for health tourism. The right jugular vein was preferred in 91 of these patients. The gastrointestinal system was the most common site of primary cancer, followed by the pancreaticobiliary system and the breast (Table 2). In this group, single-agent chemotherapy protocols were used the most. The mean duration of follow-up was calculated to be 12.3 mo.
| Primary diagnosis | n (%) |
| Gastrointestinal system cancers | 115 (57.5) |
| Breast cancers | 28 (14.0) |
| Pancreaticobiliary system cancers | 26 (13.0) |
| Head and neck cancers | 11 (5.0) |
| Gynecologic cancers | 9 (4.5) |
| Soft tissue sarcomas | 4 (2.0) |
| Lung cancers | 3 (1.5) |
| Lymphomas | 2 (1.0) |
| Renal cell cancer | 1 (0.5) |
| Adenocarcinoma of unknown origin | 1 (0.5) |
Group 2 included 56 female and 44 male patients; a total of 53 were international and came from abroad for health tourism. The right subclavian vein was preferred in 95 patients. The gastrointestinal system was the most common site of primary cancer, followed by the breast and pancreaticobiliary systems. Single-agent chemotherapy protocols were used in 41 patients, two chemotherapy agents were used in 41 patients, and three agents were used in 18 patients. The mean duration of follow-up was calculated to be 14.6 mo. There was no statistically significant difference between group 1 and group 2 patients regarding age, sex, side, number of drugs used for chemotherapy, or duration of port usage (P > 0.05) (Table 3).
| Parameters | Group 1 | Group 2 | P value |
| Age, mean ± SD (median) | 58.2 ± 11.3 (61.0) | 60.9 ± 12.7 (63.5) | 0.0601 |
| Port use duration in mo, mean ± SD (median) | 12.3 ± 9.9 (9.5) | 14.7 ± 19.8 (8.0) | 0.3551 |
| Sex | 0.0662 | ||
| Female | 43 (43) | 56 (56) | |
| Male | 57 (57) | 44 (44) | |
| Side | 0.2682 | ||
| Right | 91 (91) | 95 (95) | |
| Left | 9 (9) | 5 (5) | |
| Number of the chemotherapy drug(s) | 0.4732 | ||
| 1 | 46 (46) | 41 (41) | |
| 2 | 42 (42) | 41 (41) | |
| 3 | 12 (12) | 18 (18) | |
| Complications | 0.0002 | ||
| Present | 2 (2) | 18 (18) | |
| Absent | 98 (98) | 82 (82) | |
| Clavien-Dindo complication severity classification | 0.0002 | ||
| 0-I | 98 (98) | 81 (81) | |
| II | 1 (1) | 6 (6) | |
| III | 1 (1) | 13 (13) |
Two complications had developed in group 1 patients in whom the jugular vein was used. According to the Clavien-Dindo classification, one of the complications was category 2 and the other one was category 3b. Nineteen complications had developed in group 2 patients in whom the subclavian vein was used. According to the Clavien-Dindo classification, six complications were category 2, two were category 3a, and eleven were category 3b. When the complication rates and the severity of those complications according to the Clavien-Dindo classification were compared, group 2 was found to have a higher rate of complications, and those complications were also found to be more severe when compared with group 1 patients (P < 0.05) (Table 3).
Despite zero occlusion in group 1, four catheters were occluded in group 2 patients. While 1 patient’s problem was solved by pressurized heparin wash, the ports had to be removed and replaced in 3 patients because of this occlusion. The patient whose problem was solved by pressurized heparin wash was on single-agent chemotherapy because of head and neck cancer. Two of the three patients whose ports were replaced had primary breast cancer, and the last patient had head and neck cancer. One patient was on a single agent, but the other two were on three-agent chemotherapy protocols. The rate of port occlusion was found to be higher in group 2 than in group 1.
In group 1, the port had to be removed due to an infection in 1 patient. Candida albicans was identified on the culture from the patient’s port. The patient was on single-agent chemotherapy due to pancreatic cancer. An infection developed in 3 patients in group 2. One of these infections was a superficial surgical site infection, successfully treated by local therapy; thus, the port could be salvaged. Two patients required the removal and replacement of the ports. Enterobacter aerogenes was identified from both catheter cultures. Both patients were on three-agent chemotherapy protocols, one for breast cancer and the other for head and neck cancer. The infection rate was found to be higher in group 2 than in group 1.
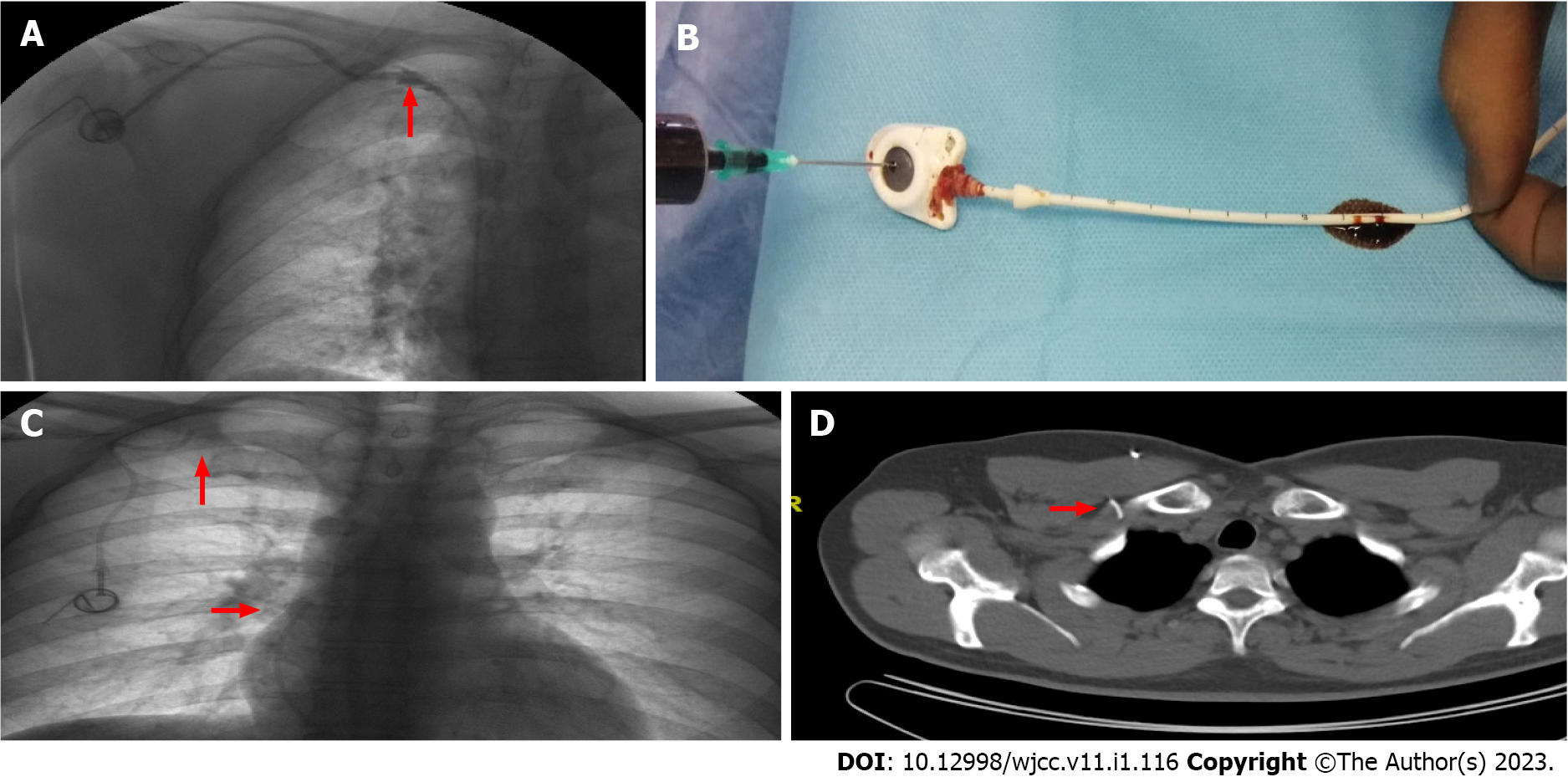
Catheter rupture was observed in 2 patients, and the central venous ports had been implanted via the subclavian vein. A linear breakage was identified in 1 patient and a complete separation in the other patient. The first patient, a 61-year-old woman, was treated with an alkaloid containing single-agent chemotherapy for primary breast cancer. The port was implanted through the right subclavian vein. The intravascular and extravascular catheter angle was above 60 degrees. In the 78th mo of her treatment, the patient experienced sharp pain in her shoulder after drug administration through her venous port. Due to this pain, her venous port was evaluated by fluoroscopy. Contrast extravasation corresponding to the subclavicular area was identified (Figure 1A). The port was removed, and a new port was implanted through the right jugular vein. In the ex situ examination, a linear breakage of approximately 2 cm was observed 9 cm distal to the port-catheter attachment point (Figure 1B). The projection of this point was predicted to be at the one-third proximal part of the clavicle, just between the clavicle and the first rib.
The other patient was a 46-year-old male on a single-agent chemotherapy protocol for colon cancer. After an uneventful treatment period through his venous port for more than 29 mo, the fluid administered through the venous port caused shoulder pain, and we could not pool blood from the port. The radiological evaluation indicated a complete breakage at a point compatible with the one-third distal part of the clavicle. The distal end of the catheter was found to be free floating in the atrium (Figure 1C). The port entrance was between the clavicle and the first rib (Figure 1D). On the next day, the interventional radiology team removed the broken distal end with an angiographic intervention. The port and the proximal part of the catheter were also extirpated, and a new central venous port was implanted through the left subclavian vein. To note, the catheter angle of this patient was also above 60 degrees.
Pneumothorax is another crucial complication of venous port implantation. No pneumothorax was identified in group 1 patients. However, in group 2 patients, a total pneumothorax requiring chest tube placement and a partial pneumothorax that improved with conservative treatment were identified.
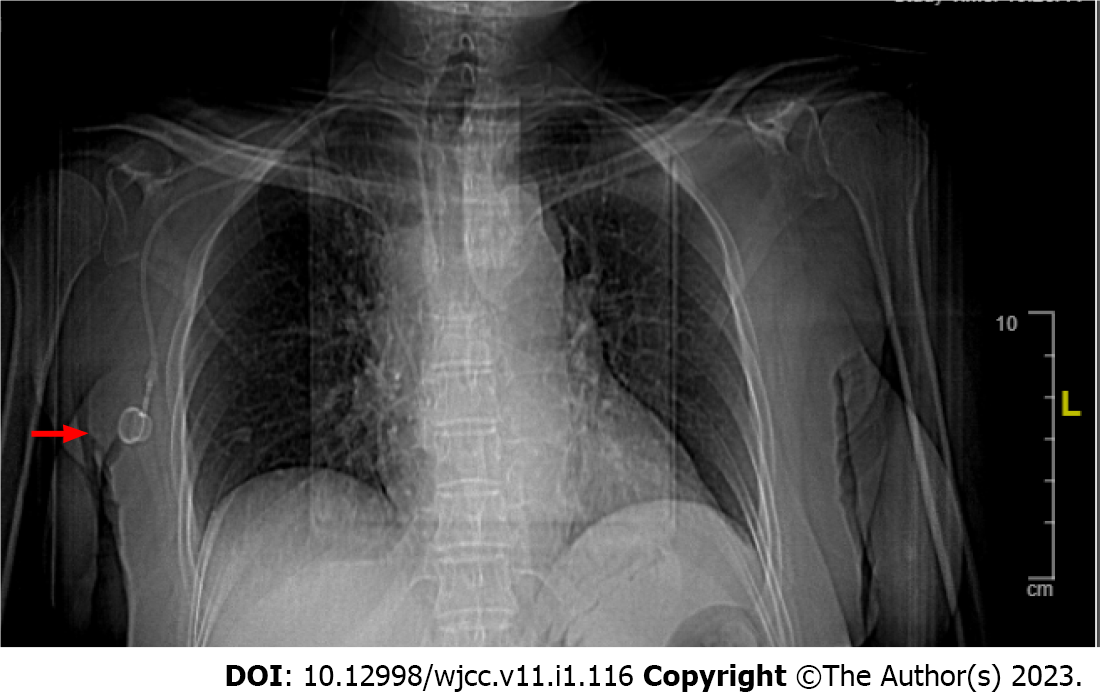
We could not puncture the port in one of the group 2 patients, and the radiological investigation revealed that the posterior, broad-based part of the port had been turned down (Figure 2). The upturned port was salvaged with revision.
Arrhythmia is another frequent complication of port implantation and developed in 1 patient. This rapid ventricular response tachyarrhythmia persisted despite the withdrawal of the guidewire. Furthermore, the rhythm recovered with vagal stimulation and antiarrhythmic therapy.
We observed suture line problems in 4 patients in group 2. In those patients, skin and subcutaneous tissue overlying the port lost their integrity. When the treatment details of these patients were reviewed, we noticed that 2 patients had received bevacizumab for lung and colon cancers. In 3 patients, the port catheters were removed and replaced with new ports. However, in 1 patient we created a new space to place the port; thus, we managed to salvage the port.
We can use central venous ports for a long period if appropriate precautions are taken during punctures and a care plan is sustained. Venous ports have an average lifespan of 2000 punctures; mechanical problems, such as occlusion, are the most frequent complications encountered. To reduce the risk of occlusion and prolong the lifetime of the ports, they should be regularly washed with heparinized solutions.
Kefeli et al[6] reported that rinsing the venous ports with 1000 U of heparin every 4-6 wk is a safe, easy, inexpensive, and effective way to prolong their usage time. Palese et al[7] evaluated the impact of rinsing frequency on port occlusion rates and compared 4 wk with 8 wk intervals, and no significant difference was found. As fewer punctures may mean a reduced risk of infection, the authors claimed that it is adequate and safe to wash ports every 8 wk. Kuo et al[8] even proposed less frequent intervals. They claimed that washing the port once every 3 mo could reduce the risk of infection and prevent heparin-related adverse events, thus enabling a safer process and port care.
At another center where port washings are performed with normal saline, it was reported that washing the ports at 3 mo intervals did not increase port complications, especially occlusion. Therefore, 3 mo could be an excellent alternative to 4 wk for port care[9]. In our study, no occlusion problem occurred in group 1 patients, but in group 2, where the subclavian vein was used, the port systems had been occluded in 4 patients. In 3 of these patients, the ports had to be removed. Besides this comparison, the absence of recorded occlusion problems was noted as a significant finding in 100 consecutive patients in group 1 in whom the jugular vein was used and ports were washed every 2 mo. Alongside robustly supporting the jugular vein approach and discordance with the abovementioned suggestions, our results also advocate a longer 2-mo interval for port care and washing.
Cancer patients are apt to develop thrombosis. In the meta-analysis of Wu et al[5], it is stated that flushing with heparinized fluid is the primary method applied in the prevention of catheter thrombosis. In patients with thrombosis, it may be necessary to remove the port if conservative methods are unsuccessful at resolving the condition. In our study, no patient experienced obstruction in the jugular ports; in contrast, obstruction due to thrombosis was detected in 4 patients in whom the subclavian route was used. One of these was opened by pressure washing with heparin; in the other 3 patients, the port was removed because the thrombosis could not be opened with conservative treatment.
Another important reason for untimely port removal is venous port and catheter infection. Those infections were reported as high as 5.6%-8% in centers with a well-established surgical site infection surveillance program[10,11]. In our study, one venous port had to be removed due to infection in group 1, and Candida albicans was identified at the port culture. In group 2, we recorded three port infections, and two of those ports were extirpated. Enterobacter aerogenes was isolated in both cultures. Group 2 was found to have a higher rate of port infection. It was concluded that the jugular vein approach was also safe in port infections, with a lower risk of mechanical problems.
Ai et al[12] evaluated port catheter fractures implanted through internal jugular veins. In 12 patients catheter fractures were identified at the entrance of the internal jugular vein, in 2 patients at the lower end of the catheter, and in 1 patient at the attachment point. Occupation, age, and duration of port usage were reported to be risk factors in port fracture. In this study, the angles of the fractured/ruptured ports were found to be above 60. In our study, port ruptures were determined in 2 patients whose venous ports were both implanted through the subclavian vein. Complete separation was observed in one rupture and a linear breakage in the other. When we reviewed the published series, most patients were asymptomatic, unlike our patients who had symptoms. Moreover, ruptures could be incidentally identified in radiological investigations. In a limited number of patients, nonspecific findings such as pain around the port, low flow blood return, and pale red blood color were stated. However, we also have consistent findings with the current literature. The ruptures developed in elderly patients in whom the ports had been used for a long period, and both of the patient’s catheter angles were above 60. Thus, we believe that in addition to pinch-off syndrome[13], we must also consider this angle to prevent ruptures. In our study, there was no recorded rupture in the jugular vein group, and we consider this finding significant.
Another significant complication of venous port implantation is pneumothorax resulting from the pleura rupture during the intervention. This complication, with an incidence of 0.5%-2.0%, prolongs the duration of hospital stay and may cause severe morbidities and even mortality[14]. It has been reported that venous port implantation through the subclavian vein increases the risk of pneumothorax while using the jugular vein under ultrasound guidance reduces the risk[15]. In line with this knowledge, no pneumothorax was recorded in group 1 patients whose venous ports were implanted through the jugular vein, but 2 patients had pneumothorax in group 2. One of those patients had a total pneumothorax necessitating a chest tube insertion. The other had partial pneumothorax, which resolved with conservative follow-up. These results concluded that using the jugular vein was also safer in terms of pneumothorax risk.
Venous ports implanted in thick subcutaneous tissue in obese patients or breast tissue in female patients may present a challenge, but an inability to use them is rare. We had only 1 patient with this problem and were obliged to revise it. The guidewire or catheter may irritate the endocardium during the port implantation and induce cardiac arrhythmia. This situation does not cause a severe problem. It is usually resolved by the withdrawal of the guidewire or catheter but on rare occasions may lead to life-threatening blocks and even asystole[16,17]. The guidewire should not be advanced more than 18 cm, and the tip of the catheter should be placed 1 to 3 cm behind the junction of the right atrium and the superior vena cava. Rhythm monitorization with electrocardiography during the whole procedure is also essential[18,19]. In our study, arrhythmia continued despite the withdrawal of the guidewire and could only be corrected by vagal stimulation and antiarrhythmic therapy.
Suture line dehiscence and loss of the integrity of the skin overlying the ports are other problems that can be observed at follow-up. Besides poor surgical technique, comorbidities and impaired wound healing due to systemic chemotherapy may increase this risk. Nutritional problems and dystrophic changes in the subcutaneous tissues may also increase this risk. This complication may necessitate surgical intervention and even replacement in the exposed ports. We also know that patients on bevacizumab, a monoclonal antibody that inhibits vascular endothelial growth factor, have an increased risk of surgical site (skin and subcutaneous tissue) complications[20,21].
For this reason, we prefer to delay bevacizumab therapy for at least 14 d after the port implantation. We were always reluctant to implant ports at previous radiotherapy or mastectomy sites to prevent wound healing problems. We prepared skin flaps of the port cavities that were not too thin and paid strict attention to having a tensionless suture line. Despite those precautions, skin and subcutaneous tissue integrity overlying the ports was impaired in 4 patients in group 2. In 3 patients, the ports had to be replaced. To note, 2 patients were on bevacizumab therapy.
International patients constitute approximately half of our cohort, and some of those patients did not have an opportunity to comply with the follow-up appointments. This follow-up challenge is a significant limitation of our study. Some complications were rare, and thereby statistical comparisons between the groups with such a limited number of patients could not be made. We consider this another limitation. Despite those limitations, our results show that the jugular vein route is safer than the subclavian vein for central venous port implantation. Some of the complications observed more often in the subclavian group compared with the jugular vein approach may be severe enough to require additional treatments.
Our study’s results also solidly support that it would be sufficient to evaluate, control, and wash the central venous ports once every 2 mo. We believe that future studies with many patients and longer follow-ups will validate those results, and the jugular vein approach will be considered the standard technique for central venous port implantation.
We showed that the internal jugular vein route for central port implantation is a feasible and safe option. Our study’s results support that it would be sufficient to evaluate, control, and wash the central venous ports once every 2 mo.
Although the number of patients who need central venous ports for permanent vascular access is increasing, there is still no “gold standard” for implantation technique.
With this retrospective study, we aimed to analyze the outcomes and adverse events in patients with a central venous port to identify the method that should be favored.
The main objective of our study was to compare the two common procedures for central venous port implantation and decide on the best option by analyzing the adverse events and complications.
In our study, electronic hospital records of 200 central venous port-implanted patients were retrospectively evaluated. Patients were assigned to two groups according to the access method: The jugular vein and the subclavian vein. Groups were evaluated by age, sex, application side, primary diagnosis, active follow-up period in the hospital, chemotherapy agents administered, number of complications, and the Clavien-Dindo severity score.
There was no statistically significant difference between groups regarding age, sex, side, number of drugs used for chemotherapy, or duration of port usage (P > 0.05). When the complication rates and the severity of those complications according to the Clavien-Dindo classification were compared, the subclavian vein group was found to have a higher rate of complications, and those complications were also found to be more severe when compared with the jugular vein group (P < 0.05). Parameters like catheter occlusion, infection, and catheter rupture were all higher in the subclavian vein group. We also recorded pneumothorax, mechanical problems like upturned port, and arrhythmia.
Of 200 consecutive patients who had undergone central venous port implantations through the jugular or subclavian vein were evaluated. There was no statistically significant difference between these two approaches regarding age, sex, side, number of drugs used for chemotherapy, or duration of port usage. The subclavian vein group was found to have a higher rate of complications, and those complications were also found to be more severe when compared with the jugular vein group. Because of these results, we concluded that the jugular vein approach is a feasible and safe option for port implantation and must be preferred to the subclavian vein approach.
We believe that future studies with many patients and longer follow-ups will validate these results, and the jugular vein approach will be considered the standard technique for central venous port implantation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ding WW, China; Lei XH, China; Mao X, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. 1982;92:706-712. [PubMed] [Cited in This Article: ] |
| 2. | Uğur Ö, Akdeniz Kudubeş A, Arslan D, Küçükkurt H, Öztürk G. İmplante port kateter sistemi bulunan kanserli hastaların portu günlük yaşamda kullanım davranışları ve etkileyen faktörlerin incelenmesi. Turkiye Klinikleri J Nurs Sci. 2016;8:204-212. [DOI] [Cited in This Article: ] |
| 3. | Plumhans C, Mahnken AH, Ocklenburg C, Keil S, Behrendt FF, Günther RW, Schoth F. Jugular versus subclavian totally implantable access ports: catheter position, complications and intrainterventional pain perception. Eur J Radiol. 2011;79:338-342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Schiffer CA, Mangu PB, Wade JC, Camp-Sorrell D, Cope DG, El-Rayes BF, Gorman M, Ligibel J, Mansfield P, Levine M. Central venous catheter care for the patient with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2013;31:1357-1370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 215] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 5. | Wu S, Huang J, Jiang Z, Huang Z, Ouyang H, Deng L, Lin W, Guo J, Zeng W. Internal jugular vein versus subclavian vein as the percutaneous insertion site for totally implantable venous access devices: a meta-analysis of comparative studies. BMC Cancer. 2016;16:747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Kefeli U, Dane F, Yumuk PF, Karamanoglu A, Iyikesici S, Basaran G, Turhal NS. Prolonged interval in prophylactic heparin flushing for maintenance of subcutaneous implanted port care in patients with cancer. Eur J Cancer Care (Engl). 2009;18:191-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Palese A, Baldassar D, Rupil A, Bonanni G, Capellari Maria T, Contessi D, De Crignis L, Vidoni A, Piller Roner S, Zanini A. Maintaining patency in totally implantable venous access devices (TIVAD): a time-to-event analysis of different lock irrigation intervals. Eur J Oncol Nurs. 2014;18:66-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Kuo YS, Schwartz B, Santiago J, Anderson PS, Fields AL, Goldberg GL. How often should a port-A-cath be flushed? Cancer Invest. 2005;23:582-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Solinas G, Platini F, Trivellato M, Rigo C, Alabiso O, Galetto AS. Port in oncology practice: 3-monthly locking with normal saline for catheter maintenance, a preliminary report. J Vasc Access. 2017;18:325-327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Lebeaux D, Larroque B, Gellen-Dautremer J, Leflon-Guibout V, Dreyer C, Bialek S, Froissart A, Hentic O, Tessier C, Ruimy R, Pelletier AL, Crestani B, Fournier M, Papo T, Barry B, Zarrouk V, Fantin B. Clinical outcome after a totally implantable venous access port-related infection in cancer patients: a prospective study and review of the literature. Medicine (Baltimore). 2012;91:309-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Lebeaux D, Fernández-Hidalgo N, Chauhan A, Lee S, Ghigo JM, Almirante B, Beloin C. Management of infections related to totally implantable venous-access ports: challenges and perspectives. Lancet Infect Dis. 2014;14:146-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Ai N, Li L, Yin F, Li Z, Geng C, Yang G. Analysis of risk factors for implantable venous access port catheter fracture with internal jugular vein. Ann Palliat Med. 2020;9:30-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Hinke DH, Zandt-Stastny DA, Goodman LR, Quebbeman EJ, Krzywda EA, Andris DA. Pinch-off syndrome: a complication of implantable subclavian venous access devices. Radiology. 1990;177:353-356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 202] [Cited by in F6Publishing: 208] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 14. | Orci LA, Meier RP, Morel P, Staszewicz W, Toso C. Systematic review and meta-analysis of percutaneous subclavian vein puncture versus surgical venous cutdown for the insertion of a totally implantable venous access device. Br J Surg. 2014;101:8-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Brass P, Hellmich M, Kolodziej L, Schick G, Smith AF. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev. 2015;1:CD006962. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 67] [Cited by in F6Publishing: 122] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 16. | Chhabra L, Spodick DH. Complete heart block--an underappreciated serious complication of central venous catheter placement. J Electrocardiol. 2012;45:790-792. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Nazinitsky A, Covington M, Littmann L. Sinus arrest and asystole caused by a peripherally inserted central catheter. Ann Noninvasive Electrocardiol. 2014;19:391-394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Unnikrishnan D, Idris N, Varshneya N. Complete heart block during central venous catheter placement in a patient with pre-existing left bundle branch block. Br J Anaesth. 2003;91:747-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Andrews RT, Bova DA, Venbrux AC. How much guidewire is too much? Crit Care Med. 2000;28:138-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Zawacki WJ, Walker TG, DeVasher E, Halpern EF, Waltman AC, Wicky ST, Ryan DP, Kalva SP. Wound dehiscence or failure to heal following venous access port placement in patients receiving bevacizumab therapy. J Vasc Interv Radiol. 2009;20:624-7; quiz 571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Erinjeri JP, Fong AJ, Kemeny NE, Brown KT, Getrajdman GI, Solomon SB. Timing of administration of bevacizumab chemotherapy affects wound healing after chest wall port placement. Cancer. 2011;117:1296-1301. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |