Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11111
Peer-review started: June 4, 2022
First decision: July 29, 2022
Revised: July 29, 2022
Accepted: September 20, 2022
Article in press: September 20, 2022
Published online: October 26, 2022
Spontaneous bilateral femur neck fracture is a rare entity in the general popu
A 17-year-old immobile, developmentally delayed male with the sequelae of cerebral palsy fractured both femoral necks during a grand mal epileptic seizure. He had been treated with valproic acid as an antiseizure medication for about 10 years; otherwise, he had no history of drug use. The laboratory analysis was normal except a marked vitamin D deficiency. Closed reduction and osteosynthesis with percutaneous cannulated screws were performed. Solid union was observed at 6 mo, and rapid postoperative rehabilitation was started.
A femoral neck fracture may occur in a person with epilepsy presenting with hip pain in the emergency department.
Core Tip: Spontaneous bilateral femoral neck fracture is a very rare entity and may develop in association with metabolic diseases, bone diseases, high-energy traumas, and epileptic seizures. It should be predicted that complications such as nonunion, loss of reduction, and avascular necrosis may develop secondary to these fractures, which are theoretically considered to be associated with metabolic diseases.
- Citation: Senocak E. Spontaneous bilateral femur neck fracture secondary to grand mal seizure: A case report. World J Clin Cases 2022; 10(30): 11111-11115
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11111.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11111
Femoral neck fractures in young patients account for approximately 3% of all femoral neck fractures and are usually secondary to high-energy trauma[1,2]. Spontaneous bilateral femoral neck fracture is very rare and may occur in association with metabolic or bone diseases, high-energy trauma, and epileptic seizures[3]. Complications of these fractures include nonunion, loss of reduction, and avascular necrosis, which are potentially associated with metabolic diseases. Early anatomical reduction, fixation, and rehabilitation are the primary goals. Spontaneous bilateral femoral neck fractures have been rarely reported[4,5].
A 17-year-old developmentally delayed immobile male with epilepsy as a sequela of cerebral palsy was brought to the emergency service due to pain in both hips after a sudden generalized tonic-clonic seizure 3 d previously.
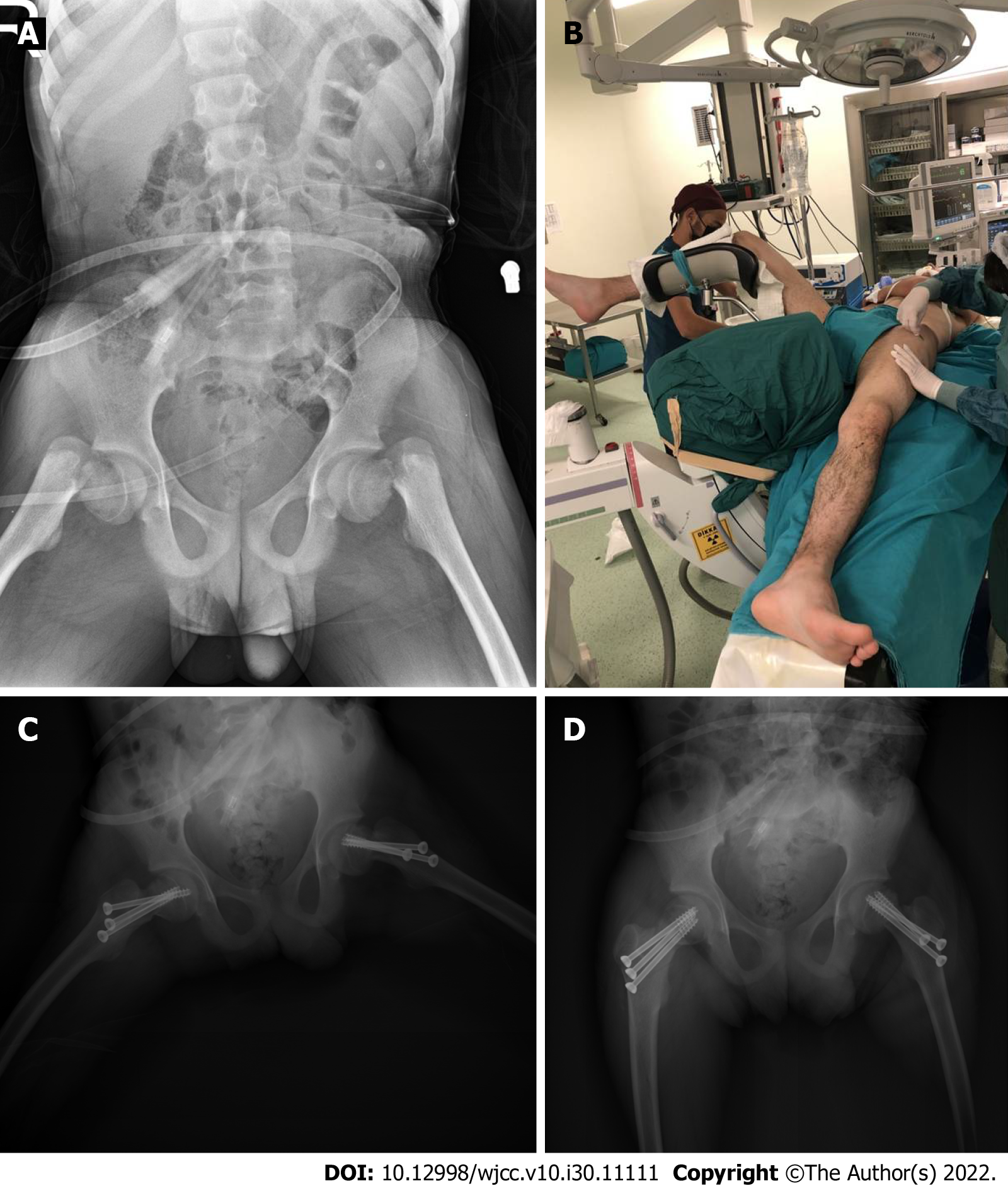
The patient had pain in both hips after a sudden generalized tonic-clonic seizure 3 d previously, as reported by his family (Figure 1).
The patient had epilepsy as a sequela of cerebral palsy, and he had been treated with the antiseizure medication valproic acid for 10 years.
The patient had no history of drug use other than valproic acid.
On physical examination, both lower extremities were in external rotation and there was pain and tenderness with movement.
The patient’s vitamin D level was relatively low (9 nmol/L), because he lacked sun exposure due to immobility (Table 1).
| Value | Referans value | |
| Ca | 9.9 nmol/L | 8.6 nmol/L-10.2 nmol/L |
| ALP | 91 nmol/L | 46 nmol/L-116 nmol/L |
| P | 4.3 nmol/L | 2.4 nmol/L-5.1 nmol/L |
| PTH | 45 nmol/L | 38 nmol/L-78 nmol/L |
| 25-OH D VİT | 9 nmol/L | 20 nmol/L-60 nmol/L |
| Mg | 2.1 nmol/L | 1.6 nmol/L-2.6 nmol/L |
The patient had bilateral femur subcapital Garden type 4 fracture as revealed by a direct pelvis anteroposterior radiograph (Figure 1A).
The patient was diagnosed as having bilateral Garden type 4 femur neck fracture secondary to a grand mal seizure.
Both hips were reduced anatomically and fixed with three 6.5-mm titanium cannulated screws. The hip joint capsules were not opened during surgery. Acceptable reduction and fixation were confirmed in the anteroposterior and lateral planes in the postoperative radiographs (Figure 1C and D).
A rapid rehabilitation program was initiated to prevent hip stiffness in the patient, who was normally immobile. After a neurology consultation, the antiseizure treatment was revised due to the potential osteoporotic effect of valproic acid. Maintenance treatment was started with phenytoin, which is a less osteolytic agent. Since his hormone levels were normal according to an endocrinology consultation, only vitamin D replacement therapy was started (Table 1).
We present a 17-year-old immobile patient who took antiseizure medication and fractured both femoral necks during an epileptic seizure. Spontaneous bilateral femoral neck fractures are extremely rare. All reported cases were secondary to high-energy trauma, epileptic seizures, electric shock, and bone metabolism disorders[4,6,7]. Several cases of bilateral femoral neck fracture secondary to epileptic seizures have been reported[8-10]. It is thought that the rigid shear force between the femoral shaft and neck, together with the sudden muscle contractions secondary to the seizure, cause the fractures[11]. Our case suggested that the femoral neck fractures resulted from the strong tonic-clonic contractions that occurred despite the use of antiseizure medication. However, we think that the long-term use of valproic acid exacerbated the fractures by decreasing bone mineral density. Our patient’s immobility promoted fracture development due to the associated decrease in bone quality.
Bilateral femoral neck fractures treated by total hip replacement have been reported in elderly patients[12,13]. Another study reported closed reduction and percutaneous screw fixation in a 30-year-old patient with bilateral femoral neck fractures after a hypoglycemic attack[14]. A 24-year-old Turkish patient with bilateral femoral neck fractures and osteopenia on postoperative bone densitometry was treated with closed reduction and percutaneous cannulated screws[5].
Since our patient was immobile, used antiseizure drugs, and had sequelae of cerebral palsy, we deemed it appropriate to perform closed reduction with three percutaneous cannulated screws after considering the patient’s condition, as it is the least invasive rigid fixation and also protects the bone. The risk of avascular necrosis in femoral neck fractures is 12%-40% in Garden type 3-4 displaced fractures[15]. Our patient was brought to our clinic 3 d after the fracture and treated quickly. Callus formation was seen 6 mo postoperatively and there was no avascular necrosis. With regular rehabilitation, there were no problems with the hip movements.
As antiseizure medication may decrease bone density, bone densitometry should be performed regularly in cases with long-term use of these drugs. Although the fixation method varies by patient age and activity level, bone-sparing surgery is preferred in young patients. Patients with epilepsy who have dislocated shoulders should also be evaluated for femoral neck fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: TOTBID, No. 2323.
Specialty type: Orthopedics
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Beran RG, Australia; Liu J, United States S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Robinson CM, Court-Brown CM, McQueen MM, Christie J. Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res. 1995;238-246. [PubMed] [Cited in This Article: ] |
| 2. | Askin SR, Bryan R. Femoral neck fractures in young adults. Clin Orthop Relat Res. 1976;114:259-264. [DOI] [Cited in This Article: ] |
| 3. | Kalaci A, Yanat AN, Sevinç TT, Doğramaci Y. Insufficiency fractures of both femoral necks in a young adult caused by osteoporosis: a case report. Arch Orthop Trauma Surg. 2008;128:865-868. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Haronian E, Silver JW, Mesa J. Simultaneous bilateral femoral neck fracture and greater tuberosity shoulder fracture resulting from seizure. Orthopedics. 2002;25:757-758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Cagırmaz T, Yapici C, Orak MM, Guler O. Bilateral femoral neck fractures after an epileptic attack: A case report. Int J Surg Case Rep. 2015;6C:107-110. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Yoon BH, Kwon MS. Atraumatic Bilateral Fracture of the Femoral Neck in Young Male Patient with Suspected Osteomalacia. J Bone Metab. 2017;24:197-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Nekkanti S, C V, Js ST, R R, Raj S. An unusual case of simultaneous bilateral neck of femur fracture following electrocution injury-A case report and review of literature. J Orthop Case Rep. 2016;6:70-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 8. | Rahman MM, Awada A. Bilateral simultaneous hip fractures secondary to an epileptic seizure. Saudi Med J. 2003;24:1261-1263. [PubMed] [Cited in This Article: ] |
| 9. | Pappademos PC, Hamilton WG. Bilateral displaced femoral neck fractures after myoclonic seizure treated with bilateral total hip arthroplasties. Am J Orthop (Belle Mead NJ). 2009;38:88-89. [PubMed] [Cited in This Article: ] |
| 10. | Grimaldi M, Vouaillat H, Tonetti J, Merloz P. Simultaneous bilateral femoral neck fractures secondary to epileptic seizures: treatment by bilateral total hip arthroplasty. Orthop Traumatol Surg Res. 2009;95:555-557. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Finelli PF, Cardi JK. Seizure as a cause of fracture. Neurology. 1989;39:858-860. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 82] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Sood A, Rao C, Holloway I. Bilateral femoral neck fractures in an adult male following minimal trauma after a simple mechanical fall: a case report. Cases J. 2009;2:92. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | McGoldrick NP, Dodds MK, Green C, Synnott K. Management of simultaneous bilateral neck of femur fractures in an elderly patient. Geriatr Orthop Surg Rehabil. 2013;4:71-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | M Shah H, Grover A, Gadi D, Sudarshan K. Bilateral neck femur fracture following a generalized seizure- a rare case report. Arch Bone Jt Surg. 2014;2:255-257. [PubMed] [Cited in This Article: ] |
| 15. | Kawasaki M, Hasegawa Y, Sakano S, Sugiyama H, Tajima T, Iwasada S, Iwata H. Prediction of osteonecrosis by magnetic resonance imaging after femoral neck fractures. Clin Orthop Relat Res. 2001;157-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |