Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11037
Peer-review started: May 21, 2022
First decision: June 27, 2022
Revised: July 7, 2022
Accepted: September 6, 2022
Article in press: September 6, 2022
Published online: October 26, 2022
Alimentary tract duplication (ATD) is a rare congenital anomaly. Thus, a case of ATD with a complete colonic duplication isolated in the abdominal cavity with a fistula and multiple malformations is very distinctive. These characteristics show the variability of this disease and explain why it tends to be challenging to dia
A 25-year-old woman with a history of a fistula opening in her right hip since birth presented with the irregular discharge of foul fluid from the fistula and intermittent abdominal pain. Contrast-enhanced computed tomography and magnetic resonance imaging findings revealed a duplicated tube isolated in her abdominal pelvic cavity along with a pelvic malformation and double ureter. Right foot radiographic examination showed pes cavus. During surgery, the tube appeared to be an almost complete colonic structure and was verified to be con
ATD may be a differential diagnosis in sinus tract cases. Laparoscopy combined with open surgery is a viable treatment option.
Core Tip: This report is an uncommon case even among the rare alimentary tract duplication (ATD) cases. An entire colonic duplication without any connection to the digestive system was isolated in the abdomen pelvic. The presence of chronic sinus and several abnormalities appearing in a single case is extremely unique. There is little understanding of this disease with no consensus on the diagnosis and treatment. Additionally, the variable clinical features often lead to misdiagnosis. Here we present a successful diagnosis and treatment approach to improve the knowledge for the care of ATD cases.
- Citation: Cai X, Bi JT, Zheng ZX, Liu YQ. Complete colonic duplication presenting as hip fistula in an adult with pelvic malformation: A case report. World J Clin Cases 2022; 10(30): 11037-11043
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11037.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11037
Alimentary tract duplication (ATD) is a rare congenital anomaly characterized by a local cyst or a section of a tube-like intestine. In most cases, the duplicated tract is connected with an area of the normal digestive system[1,2]. The malformation has been reported to occur anywhere along the gastrointestinal tract from the mouth to the anus. According to clinical data, the ileum is the most common site, accounting for approximately 80% of cases. However, colonic duplication is unusual, accounting for approximately 6%–7% of cases. To the best of our knowledge, there are no previous reports or research on cases involving a body fistula combined with a pelvic malformation[3,4]. This disease usually manifests as abdominal pain, distension, hematochezia, constipation, obstruction, perforation, and even intestinal twisting. Given that more than 80% of patients can undergo treatment before the age of 2 years, adult cases are rare[4,5].
We report a case of colonic duplication presenting as a hip fistula in a 25-year-old woman with pelvic malformation. This is also a rare presentation of ATD and to our knowledge, has never been reported in the literature. To help improve medical care for ATD, the case presented here includes detailed patient history, diagnostic information, and details of treatment.
A 25-year-old woman with a fistula opening in her right hip since birth presented with intermittent pain in her abdomen for 3 years.
The patient complained of irregular dirty stool-like fluid discharge from the fistula and a pronounced limp while walking since she was a child. Additionally, scar tissue was found next to the fistula, which was a recurrent infection and abscess that had occurred and healed in the past. In addition, she had newly started experiencing intermittent abdominal pain frequently for the last 3 years without special signs, such as hematochezia, which was relieved by conservative treatment by oral or intravenous administration of antibiotics.
No local medical institutions were able to provide radical treatment to the patient owing to the complexity and high risk of complications of the disease. Severe acute abdominal pain was treated with intravenous antibiotics in the emergency department. Unfortunately, the patient cannot provide more detailed information concerning these treatments.
The patient was of a yellow race and worked as a radiology technician in a local medical institution her height and weight were 155 cm and 43 kg, respectively. During adolescence, the menstrual cycle of the patient was irregular, and the bleeding lasted longer than normal. She experienced occasional constipation and had no history of trauma or surgery. She had no history of hypertension, coronary artery disease, diabetes, or any other chronic and infectious disease. No family history was identified.
The fistula appeared as a neoplasm located in her right hip nearby (approximately 5 cm) to a scar with round features (Figure 1A). A belly bulge on the right abdomen could be observed in the supine position. Abdominal palpation revealed a tubular structure. There was no tenderness, rebound tenderness, or tension.
Routine blood tests, such as blood routine examination, renal and liver function, electrolyte, coagulation function, and tumor markers did not reveal any abnormalities except mild anemia (90 g/L, 115–150 g/L). Given the patient’s history of the menstrual disorder and her compressed uterus and ovary, the serum levels of sex hormones were also evaluated and were found to be within the normal range.
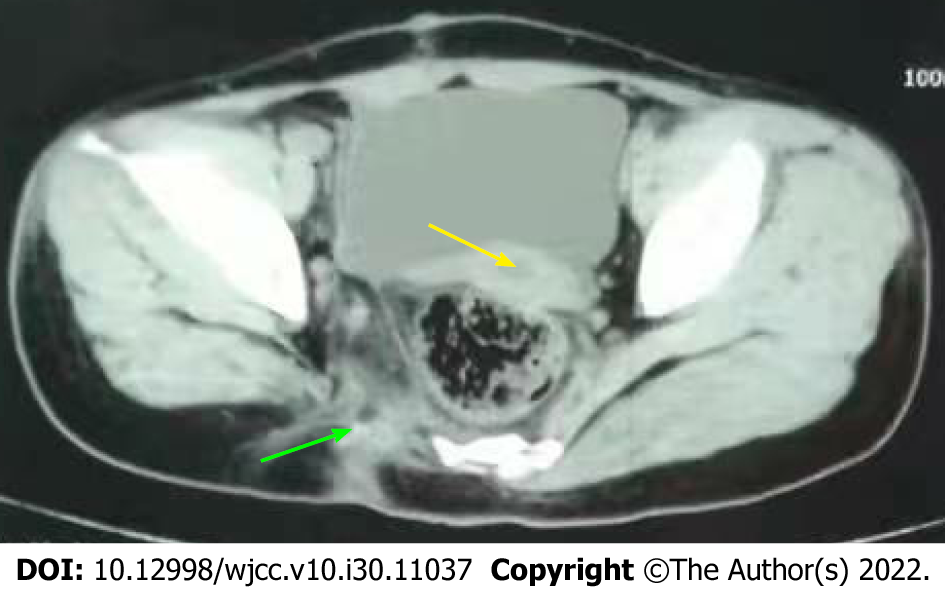
Combined contrast-enhanced computed tomography (CT) with contrast epistolography revealed a large, dilated lumen structure with a large number of stored feces in the abdominal pelvic cavity (Figure 1B). The organs around the duplicated tract were compressed and the fistula, which connected with the distal tubular structure, was clearly shown by contrast enhancement (Figure 1C). It is possible that there was another sinus tract connecting to the proximal tubular structure with the recurrent infection area on the hip. Both CT and magnetic resonance imaging revealed abnormal morphology of the sacrum and absence of bone structures (Figure 1D). Ultrasonography showed that the uterus and ovary had normal morphologies. A double ureter and renal pelvic on the right side could be observed using contrast-enhanced CT. The right foot radiograph showed a pes cavus (Figure 1E). The co
A multidisciplinary conference was convened to clarify the diagnosis, make a treatment plan, and assess surgical risks and prognosis, especially concerning her reproductive system. Hence, the departments involved were general surgery, urology, spine surgery, obstetrics-gynecology, anesthesiology, and intensive care unit. Based on the investigation and discussion, they achieved a consensus that the final diagnosis was ATD, a special type of tubular colonic duplication with multiple anatomical abnor
A laparoscopic exploration and duplicated tract resection surgery were performed under general anesthesia. We located the double ureter and fully free the duplicated tract in the abdominal pelvic cavity under laparoscopic view. Thereafter, the patient’s operative position was changed to right supine. Methylene blue solution was injected into the duplicated tract from the right hip fistula to guide the extent of excision. This method is also commonly used in pilonidal sinus surgery cases[6,7]. After the closure of the fistula with sutures, a shuttle shape incision was made to remove the tract from the skin of the pelvic cavity along the blue-staining wall that bordered the fistula and normal tissue (Figure 2A). Finally, the tract met the fistula and the pelvis, and the entire duplicated tract was removed from the abdominal cavity through a rectus abdominal incision (Figure 2B). A tough non-absorbable stitch was used to close the defect left by the removed tract in the pelvic floor muscle layer.
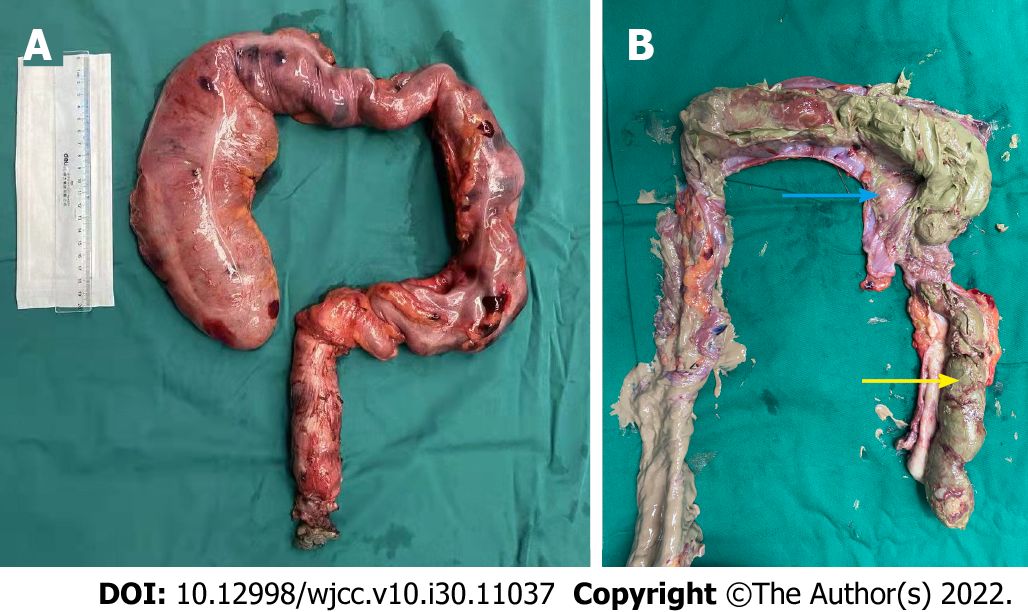
The duplicated track was the length of the colonic tube in the retroperitoneal space of the right abdominal cavity and was covered by a sac-like peritoneal structure. We found the duplication of the ureter from the right kidney crossing the sac (Figure 2C and D). The blood supply was from an artery branching from the aortaventralis, between the inferior mesenteric artery and the cross of the iliac vessels. Distally, the tract eventually entered into the muscular layer of the pelvic floor and terminated as a hip fistula, while proximally the tract had a blind side that had a clear border around its tissue and no connection with the body surface. The surgical specimen was a large luminal structure that appeared like a whole section of the colon (Figure 3A). After opening the lumen, a large amount of fecal slag-like secretion and a substantial portion of the tract components were found (Figure 3B).
Pathology showed that duplicated tract was well-structured; the serosa, muscular, and mucous layers were similar to that of the intestinal canal. Upon hematoxylin and eosin staining, the mucous layer exhibited chronic inflammation with a large number of leukomonocytes (Figure 4A). The sinus tract was covered by squamous cells and intestinal mucosa and was infiltrated by lymphocytes (Figure 4B).
The patient had an uneventful recovery without short-term complications. At the 8-mo follow-up visit after surgery, the patient was still doing well. There was no pelvic floor hernia observed on the abdominal pelvic CT findings (Figure 5).
ATD is an exceedingly rare congenital deformity. Thus far, despite several theories and hypotheses, there is no clear pathogenesis. Attempts have been made to categorize it based on morphology and source of the duplicated tube. However, there has never been a consensus that could provide a definition, classification, and mechanism to describe the main characteristics of this disease in literature[8-10]. Therefore, we could not definitively diagnose this case as ATD.
This case was unique as the duplicated tube contained an entire anatomical structure resembling the colon. Additionally, there were no connections between the normal digestive tract and the duplicated tube. We also could not identify any double tube or Y-shaped tube as observed in a previously reported case[1]. In our case, the duplicated tract was located in the right retroperitoneal space as a separate entity from the abdominal cavity. Therefore, it is difficult to place this into any previous classification. Based on the patient’s history, we suspected that the sinus tract in the right hip may have formed along with the duplicated tube in the abdominal pelvic cavity, which may have led to abnormalities of the ipsilateral pelvis. However, the observed pes cavus could not be explained as a consequence of this process, and could not find any link between these two. We also hypothesized that the duplicated colonic tube and sinus tract may be another complete colorectum and anus. However, there were no structures, such as sphincters, found in the sinus tract during operation or any record of functions, such as contraction and diastole in the patient’s history. The development of the duplicated tract, in this case, is definitely worth further investigation and conclusion.
ATD is usually accompanied by digestive system symptoms, such as abdominal pain, distention, diarrhea, constipation, hematochezia, obstruction, and even volvulus[4]. As a result, in most cases, it is detected and treated early, usually in childhood. A distinctive feature of our case was that the patient did not present with any digestive symptoms in her childhood as there was no connection between the normal bowel and the duplication. The only early presentation was related to the hip fistula with discharge. Colonoscopy and barium radiography, the examinations of choice for this disease, were unrevealing[11]. As a result, the diagnosis and treatment for alimentary tract malformation were delayed. Therefore, in our opinion, for patients with sinus tracts not caused by trauma or nosocomial damage, ATD must be considered a differential diagnosis. Considering that the fistula and neoplasm may be hip bursitis or commonly infected sinus tract can easily lead to missing further inspection and delayed treatment. In most cases, an ultrasound examination may help detect the problem and exclude most differential diagnoses[12]. Additionally, diagnosis also requires multiple modes of examination and multidisciplinary involvement. It is difficult to appreciate the whole anatomical structure of the duplicated tube through routine imaging, including gastro-and-enteroscopy, which also provides a negative result. Thus, an exploratory laparotomy must be conducted.
Undoubtedly, based on both the literature and specialist’s opinion, surgery remains the only option for a cure and should be performed within a limited period, because of the malignant potential of the duplicated tube[13,14]. Owing to the tract traversing the peritoneal reflection to the pelvic floor, we used laparoscopic devices to operate. Laparoscopy combined with open surgery can be performed under a clear and magnified field of vision, which can help identify and detect abnormal structures, such as the double ureter in this patient (Figure 2C), and can ultimately protect the normal tissue. Moreover, the instruments have an advantage over open surgery in deep and narrow spaces such as the pelvic floor. Finally, only a small incision is required to remove the pathological specimens. Because of these advantages, in the last decade, an increasing number of cases have reported the application of laparoscopy in the treatment of this disease[15,16]. For outcomes of treatment, there was no definitive result and high-level evidence to indicate that the laparoscopy involved in the surgery is a better choice, even in colon cancer[4]. However, compared to open operation, a smaller incision was an obvious advantage. The potential risk of pelvic floor hernia was also discussed, as the surgery cannot improve or reconstruct the abnormal morphology of the sacrum. However, during the operation, we found that the muscular strength in the pelvic floor was normal. Additionally, the defect had already been closed by a non-absorbable suture (2-0 prolene) following the fistula removal. Therefore, the prophylactic mesh was not considered in this case. Long-term follow-up still requires constant evaluation, especially for pregnancy. According to the above results, we can adjust the treatment strategy.
In ATD, adult cases always have a long history. Additionally, cases tend to be complex, each with unique features. This also contributes to the uncertainty of treatment. Therefore, the development of a treatment strategy should be thorough and meticulous. Multi-disciplinary consultation and careful diagnosis are essential for treatment. As in this case, surgical laparoscopy is recommended as part of the treatment.
We thank the patient and the members of our team.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Augustin G, Croatia; Corvino A, Italy S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063-1080. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 316] [Cited by in F6Publishing: 268] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Ricciardolo AA, Iaquinta T, Tarantini A, Sforza N, Mosca D, Serra F, Cabry F, Gelmini R. A rare case of acute abdomen in the adult: The intestinal duplication cyst. case report and review of the literature. Ann Med Surg (Lond). 2019;40:18-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Siamionava Y, Varabei A, Makhmudov A. Transverse colon duplication with chronic constipation in adult. BMJ Case Rep. 2019;12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Liu R, Adler DG. Duplication cysts: Diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound. 2014;3:152-160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 110] [Cited by in F6Publishing: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 5. | Kekez T, Augustin G, Hrstic I, Smud D, Majerovic M, Jelincic Z, Kinda E. Colonic duplication in an adult who presented with chronic constipation attributed to hypothyroidism. World J Gastroenterol. 2008;14:644-646. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 6. | Idiz UO, Aysan E, Firat D, Bozkurt S, Buyukpinarbasili N, Muslumanoglu M. Safety and/or effectiveness of methylene blue-guided pilonidal sinus surgery. Int J Clin Exp Med. 2014;7:927-931. [PubMed] [Cited in This Article: ] |
| 7. | Strevinas A, Reid AJ, McGrouther DA. Sinus tract identification by Methylene Blue gel. J Plast Reconstr Aesthet Surg. 2013;66:e297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | McPherson AG, Trapnell JE, Airth GR. Duplication of the colon. Br J Surg. 1969;56:138-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Paulson EC, Mahmoud NN. Sigmoid colon duplication cysts. Am Surg. 2008;74:250-252. [PubMed] [Cited in This Article: ] |
| 10. | Banchini F, Delfanti R, Begnini E, Tripodi MC, Capelli P. Duplication of the transverse colon in an adult: case report and review. World J Gastroenterol. 2013;19:586-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 13] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Jimenez SG, Oliver MR, Stokes KB, Morreau PN, Chow CW. Case report: Colonic duplication: a rare cause of obstruction. J Gastroenterol Hepatol. 1999;14:889-892. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Corvino A, Corvino F, Tafuri D, Catalano O. Usefulness of dynamic ultrasound in the diagnosis of epigastric herniation of the stomach. Ultrasound. 2022;30:162-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 13. | Ademuyiwa AO, Bode CO, Adesanya OA, Elebute OA. Duplication cyst of ascending colon presenting as an ileal volvulus in a child: a case report and review of literature. Afr J Paediatr Surg. 2012;9:237-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kang M, An J, Chung DH, Cho HY. Adenocarcinoma arising in a colonic duplication cyst: a case report and review of the literature. Korean J Pathol. 2014;48:62-65. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Patiño Mayer J, Bettolli M. Alimentary tract duplications in newborns and children: diagnostic aspects and the role of laparoscopic treatment. World J Gastroenterol. 2014;20:14263-14271. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 56] [Cited by in F6Publishing: 45] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 16. | Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010;34:2026-2040. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |