Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.10967
Peer-review started: March 14, 2022
First decision: June 16, 2022
Revised: July 6, 2022
Accepted: September 16, 2022
Article in press: September 16, 2022
Published online: October 26, 2022
Many systematic reviews have focused on assessing the effect of body mass index (BMI) on the outcomes and complications associated with total hip arthroplasty (THA) and total knee arthroplasty (TKA), but primarily dealt with obesity compared to normal weight (NW). None of these reviews attempted to assess the effect of low BMI or underweight (UW) compared to NW in patients undergoing THA or TKA.
This review aims to compare specific operative outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, deep vein thrombosis, etc. along with re-hospitalization and reoperation rates between UW and NW patients undergoing THA, TKA or both.
An electronic search was performed in PubMed, Scopus, Excerpta Medica database (EMBASE), Web of Science (WoS), and Cochrane Central Register of Controlled Trials (CENTRAL) along with a manual search. The quality of the studies was assessed using the Newcastle-Ottawa scale for cohort studies. The data were subjected to both qualitative and quantitative analysis.
Thirteen retrospective and five prospective cohort studies were included. The quality of included studies was assessed to be good to fair. The length of hospital stay after TKA or THA was found to be significantly higher for UW patients when compared to NW patients, with a mean difference: 0.39 95%CI: [0.06, 0.72], P = 0.02 (in days). Studies presenting both THA and TKA together as total joint arthroplasty showed an increased incidence of mortality in patients treated with THA or TKA alone, Odds ratio: 4.18 95%CI: [2.88, 6.07]. A higher incidence of post-ope
UW patients undergoing THA or TKA had a higher incidence of post-operative complications and were associated with a higher readmission rate. Moreover, UW patients were associated with an increased incidence of mortality in the studies that reported THA and TKA together.
Core Tip: Many systematic reviews have focused on assessing the effect of body mass index (BMI) on the outcomes and complications associated with total hip arthroplasty (THA) and total knee arthroplasty (TKA), but primarily dealt with obesity compared to normal weight (NW) patients. None of these reviews attempted to assess the effect of low BMI or underweight (UW) compared to NW in patients undergoing THA or TKA. The present analysis found that UW patients undergoing THA or TKA had with a higher incidence of post-operative complications and were associated with a higher readmission rate.
- Citation: Ma YP, Shen Q. Impact of being underweight on peri-operative and post-operative outcomes of total knee or hip arthroplasty: A meta-analysis. World J Clin Cases 2022; 10(30): 10967-10983
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/10967.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.10967
Body mass index (BMI) plays a pivotal role in predicting the outcomes and associated complications after total hip arthroplasty (THA) and total knee arthroplasty (TKA)[1]. BMI in the population is mainly divided into 5 categories: Underweight (score of < 18.5); normal weight (18.5-24.9); overweight (25-29.9); obese (30-34.9) and morbidly obese (> 40). This score is defined by weight in kilograms per square meter of height[2].
Extreme values of BMI are regarded as a risk factor for various systemic diseases such as diabetes, cardiovascular diseases, pulmonary diseases, dementia, and notable osteoarthritis in the elderly[3]. Obesity has already been proved to be associated with poor clinical outcomes, and lower success rates in patients undergoing total joint arthroplasty (TJA)[4,5]. Obese patients present with a higher incidence of infection, and complications compared to normal weight (NW) individuals[6]. However, the results were conflicting. Despite this negative relation between obesity and the success of THA or TKA, some studies established that no difference was observed between obese and non-obese patients in terms of clinical outcomes, survival rate, and complications[7-9].
Underweight (UW) patients suffer from poor nutrition, anemia, vitamin deficiencies, and most importantly osteoporosis due to calcium and vitamin D deficiency. Osteoporosis is a major risk factor for patients with osteoarthritis requiring THA or TKA. The understanding of prognosis post-THA or TKA in UW patients is less studied and not clearly understood. The literature which focused on evaluating the effect of BMI also showed the outcomes of UW patients undergoing arthroplasty. It was interesting to note that UW patients may also lead to poor post-operative outcomes, including increased rates of post-operative infection, transfusion, cardiovascular events, and renal complications[10,11]. UW patients have also been shown to potentially delay mobilization, increase length of stay and hospital expenditures[12,13]. However, the evidence is scarce, and very few studies directly attempted to assess the effect of UW compared to NW individuals.
Many systematic reviews have focused on assessing the effect of BMI on the outcomes and complications associated with TJA[14-17], but primarily dealt with obesity compared to NW. None of the reviews attempted to assess the effect of low BMI or UW in patients undergoing THA or TKA. The risk of UW patients undergoing TJA is debatable and no substantial evidence has been put forth. This is the first review to compare operative and post-operative complications between UW and NW patients undergoing THA or TKA. The objective of this review is to compare the specific operative outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, deep vein thrombosis (DVT), etc. along with rehospitalization and reoperation rates between UW and NW patients undergoing THA, TKA or both.
This systematic review and meta-analysis were performed according to the preferred reporting items for systematic review and meta-analysis (PRISMA) guidelines[18]. The protocol for conducting this review was predefined and employed to conduct the systematic review efficiently in a smooth manner. Ethics approval was not required for this review.
What is the impact of UW compared to NW on operative outcomes, rehospitalization and reoperation rates, and post-operative complications in patients undergoing THA or TKA?
The following PICO strategy was employed to formulate the research question and search strategy to identify eligible articles: Patients (P): Patients undergoing THA or TKA; Exposure (E): UW patients with BMI < 18.5 kg/m2; Comparison (C): NW patients with BMI between 18.5-24.9 kg/m2; Outcome (O): Operation duration (in min), length of hospital stay (in days), and post-operative complications such as mortality, infections, DVT, pulmonary embolism, genito-urinary complications, dislocation/ subluxation, fracture along with rehospitalization and reoperation rates expressed as a proportion (event/total); Study design (S): All observational studies comparing outcomes of UW vs NW patients undergoing THA or TKA or TJA.
A comprehensive search strategy was developed to identify the relevant articles to answer the question. An electronic search was performed in PubMed, Scopus, Excerpta Medica database (EMBASE), Web of Science (WoS), and Cochrane Central Register of Controlled Trials (CENTRAL). The search strategy was framed using the following relevant keywords: underweight; "low body mass index"; malnourished; "Total knee arthroplasty"; "Total joint arthroplasty"; "Total hip arthroplasty"; mortality; complications; rehospitalization; readmissions; “length of hospital stay”. The details of the search strategy are provided in Table 1. No limits or restrictions were applied to the electronic search. The last electronic search was carried out in June 2021. An additional manual search was also carried out in peer-reviewed relevant journals such as the Journal of Orthopedics; Journal of Arthroplasty; Journal of Orthopedic Surgery and Research; and Journal of Knee Surgery, Sports Traumatology, and Arthroscopy. The reference list of previously conducted relevant systematic reviews and other relevant studies were screened for possible inclusion of eligible articles. The identified reports along with electronic search results were imported into a citation manager (ENDNOTE) in order to discard duplicates obtained from multiple databases.
| Database | Search strategy | Results |
| PubMed | ((((“Under-weight”) OR (Low body mass index)) OR (malnourished)) AND (((("total knee arthroplasty"[All Fields]) OR ("total hip arthroplasty"[All Fields])) OR ("total joint arthroplasty"[All Fields])) OR ("total knee replacement"[All Fields]))) AND (((((mortality) OR (complications)) OR (readmissions)) OR (rehospitalization)) OR (length of hospital stay)) | 243 |
| CENTRAL | #1 Underweight | 25 |
| #2 Low body mass index | ||
| #3 Malnourished | ||
| #4 #1 OR #2 OR #3 | ||
| #5 MeSH descriptor: [Arthroplasty, Replacement, Knee] explode all trees | ||
| #6 MeSH descriptor: [Arthroplasty, Replacement, Hip] explode all trees | ||
| #7 MeSH descriptor: [Arthroplasty, Replacement] explode all trees | ||
| #8 #5 OR #6 OR #7 | ||
| #9 #4 AND #8 | ||
| EMBASE | ((((“Under-weight”) OR (Low body mass index)) OR (malnourished)) AND (((("total knee arthroplasty"[All Fields]) OR ("total hip arthroplasty"[All Fields])) OR ("total joint arthroplasty"[All Fields])) OR ("total knee replacement"[All Fields]))) AND (((((mortality) OR (complications)) OR (readmissions)) OR (rehospitalization)) OR (length of hospital stay)) | 67 |
| WoS | TS=(“under-weight” OR "low body mass index" OR malnourished ) AND TS=("Total knee arthroplasty" OR " Total joint arthroplasty" OR "Total hip arthroplasty") AND TS=(mortality OR complications OR rehospitalization OR readmissions OR “length of hospital stay” ) | 110 |
| SCOPUS | ALL (“under-weight” OR "low body mass index" OR malnourished) AND ALL ("Total knee arthroplasty" OR " Total joint arthroplasty" OR "Total hip arthroplasty") AND ALL (mortality OR complications OR rehospitalization OR re-admissions OR “length of hospital stay”) | 261 |
The reports were screened by two independent reviewers based on the below-mentioned inclusion and exclusion criteria:
Inclusion criteria: All studies comparing outcomes of UW vs NW patients undergoing THA or TKA or TJA. Studies reporting outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, DVT, pulmonary embolism, genito-urinary complications, dislocation/subluxation, fracture along with rehospitalization and reoperation rates. Studies attaining a minimum score of 7 assessed using the Newcastle-Ottawa scale (NOS) of quality assessment were included.
Exclusion criteria: Studies published in other than the English language. Studies not reporting relevant outcomes. Studies recruiting patients with other systemic diseases, and immune-compromised patients. Studies with a score less than 7 assessed using the NOS of quality assessment were excluded.
Data extraction was performed by two independent reviewers (YM, and QS) using an Excel spreadsheet. The demographic characteristics and details of outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, DVT, pulmonary embolism, genito-urinary complications, dislocation/subluxation, fracture along with rehospitalization and reoperation rates were extracted. The authors were contacted by email for clarification on missing data or unclear information.
The extracted data were subjected to both qualitative and quantitative analysis. The outcomes which could not be combined for quantitative analysis were summarized. The continuous data of the extracted outcomes were expressed as mean and standard deviation. The dichotomous outcomes were expressed as an absolute number of events, ratio, and proportion. The outcome effect was calculated between UW and NW patients as the mean difference for continuous outcomes and odds ratio for dichotomous outcomes. The quantitative data were subjected to meta-analysis using RevMan v 5.4 software. The meta-analysis was carried out only if two or more studies with similar outcomes were available. A P value < 0.05 for assessing the outcome effect was considered significant. A random effect model was chosen if the included studies presented a varied population. The heterogeneity among the studies was assessed using I2 statistics. The heterogeneity was considered low if the I2 value was found to be < 40%, moderate for a value of 40%-70%, and high for a value more than 70%. The studies presented the data on THA or TKA alone and reported both THA and TKA data together. Hence, a sub-group analysis was carried out based on the type of joint arthroplasty reported. For outcomes such as mortality, a sub-group analysis was carried out based on the time frame.
The methodological quality of included studies was assessed by two independent reviewers using the NOS. The NOS consists of eight items grouped into three categories, namely: selection, comparability, and outcome. A scoring system, ranging from zero to nine stars, was used to classify the quality of the study being reviewed. Each included study received the following categorical scores representing its quality: good (three or four scores in the selection domain AND one or two scores in the comparability domain AND two or three scores in the outcome domain), fair (two scores in selection domain AND one or two scores in comparability domain AND two or three scores in outcome domain) or poor (zero or one score in selection domain OR zero score in comparability domain OR zero or one score in outcome domain).
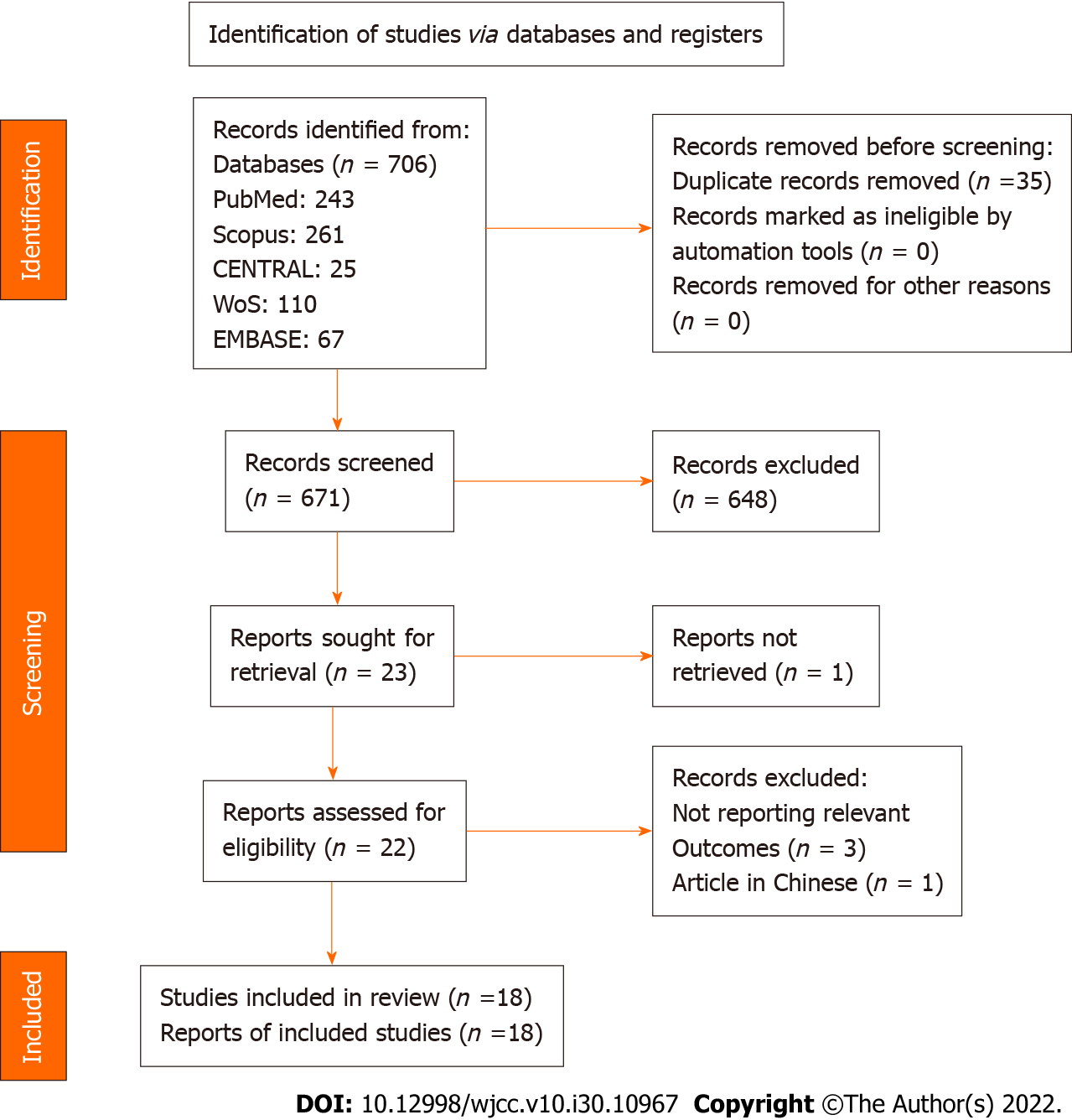
A total of eighteen studies[10,11,19-34] were included in this review. Twenty-two eligible studies[4,35-37] were screened from a pool of 671 records identified from both electronic and manual searches, purely based on title and abstract. The inclusion and exclusion criteria were strictly applied to carry out the full-text assessment of eligible studies. Finally, eighteen studies were deemed inclusive after satisfying the pre-defined criteria. The complete study selection process is described in Figure 1, and the detailed search strategy employed in all databases is provided in Table 1.
Thirteen retrospective cohort studies[10,11,19-23,25,26,28,29,31,33] and five prospective cohort studies[24,27,30,32,34] were included. The studies included a total of 1136506 subjects undergoing TKA or THA with a mean age of 65.32 years. The subjects comprised 469387 males and 667119 females. Out of these recruited subjects undergoing TKA or THA, 213028 subjects were NW individuals with a BMI between 18.5 and 24.9, and only 10785 subjects were UW individuals with a BMI < 18.5. Sixteen studies[10,19,21-34] assessed the outcomes for THA and nine studies[11,19,20,23,26,28,30,31,33] for TKA. Only seven studies[19,23,26,28,30,31,33] presented data with both THA and TKA. The demographic characteristics of the included studies are provided in Table 2. The quality of studies assessed using NOS was found to be good to fair quality. Details of the Newcastle-Ottawa scoring criteria according to domains were well presented and are shown in Table 3.
| Ref. | Type of study | Total participants | Age (mean) | Follow up time | Gender (F/M) | Treatment | Groups | Number of participants per group |
| Hartford et al[20], 2020 | Retrospective | 1774 | 67.08 | 3 mo | 1078/696 | THA | Underweight | 13 |
| Normal | 463 | |||||||
| Katakam et al[18], 2021 | Retrospective | 4802 | 65.9 | 2 yr | 2698/2104 | THA and TKA | Underweight2 | 85 |
| Normal | 821 | |||||||
| Kwon et al[19], 2020 | Retrospective | 118 | 70.75 | 2 yr | 118/0 | TKA | Underweight | 41 |
| Normal | 77 | |||||||
| Sloan et al[22], 2019 | Retrospective | 378775 | 65.7 | 1 mo | 224912/153863 | THA and TKA | Underweight | 1846 |
| Normal | 51130 | |||||||
| Hung et al[24], 2019 | Retrospective | 1565 | 54.46 | 1 mo | 830/735 | THA | Underweight | 56 |
| Normal | 697 | |||||||
| Sayed-Noor et al[23], 2019 | Prospective | 83146 | 69 | 2 yr (90 d mortality) | 47210/35936 | THA | Underweight | 579 |
| Normal | 25718 | |||||||
| Woo et al[21], 2019 | Retrospective | 3672 | 78.06 | 1 yr | 2620/1007 | THA | Underweight | 332 |
| Normal | 750 | |||||||
| Dowsey et al[27], 2018 | Retrospective | 172767 | 67.65 | 5 yr | 104742/68024 | THA and TKA | TKA + Underweight | 268 |
| TKA + Normal | 13261 | |||||||
| THA +Underweight | 492 | |||||||
| THA + Normal | 13226 | |||||||
| Shohat et al[25], 2018 | Retrospective | 18173 | 61.33 | 3 mo | 9986/8187 | THA and TKA | Underweight | 96 |
| Normal | 3266 | |||||||
| Zusmanovich et al[9], 2018 | Retrospective | 840 | 72.05 | 1 mo | 660/180 | THA | Underweight | 301 |
| Normal | 539 | |||||||
| Mouchti et al[26], 2018 | Prospective | 415598 | 67.75 | 3 mo | 246780/168818 | THA | Underweight | 3588 |
| Normal | 86336 | |||||||
| Manrique et al[10], 2017 | Retrospective | 108 | 69.7 | 3.8 yr | 93/24 | TKA | Underweight | 27 |
| Normal | 81 | |||||||
| Anoushiravani et al[30], 2016 | Retrospective | 4864 | 70.54 | NA | 4064/800 | THA and TKA | THA + Underweight1 | 1762 |
| THA + Normal | 1787 | |||||||
| TKA + Underweight | 670 | |||||||
| TKA + Normal | 645 | |||||||
| Husted et al[29], 2016 | Prospective | 13730 | NR | 3 mo | NR | THA and TKA | TKA + Underweight | 29 |
| TKA + Normal | 1250 | |||||||
| THA + Underweight | 77 | |||||||
| THA + Normal | 2396 | |||||||
| Shaparin et al[28], 2016 | Retrospective | 880 | 61.33 | 1 mo | 541/339 | THA | Underweight | 17 |
| Normal | 168 | |||||||
| Zhao et al[31], 2014 | Prospective | 236 | 36.5 | NA | 34/202 | THA | Underweight | 91 |
| Normal | 145 | |||||||
| Thornqvist et al[32], 2014 | Retrospective | 34744 | 70.6 | 1 mo | 20438/14306 | THA and TKA | Underweight | 353 |
| Normal | 9859 | |||||||
| Zhang et al[33], 2012 | Prospective | 714 | 62.17 | 5-20 yr | 315/399 | THA | Underweight | 62 |
| Normal | 413 |
| Ref. | Selection | Comparability | Outcome | Total | |||||
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest | Basis of the design or analysis | Assessment of outcome | Follow-up long enough for outcomes | Adequate follow up | ||
| Hartford et al[20], 2020 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Katakam et al[18], 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Kwon et al[19], 2020 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Sloan et al[22], 2019 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Hung et al[24], 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Sayed-Noor et al[23], 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Woo et al[21], 2019 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Dowsey et al[27], 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Shohat et al[25], 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Zusmanovich et al[9], 2018 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Mouchti et al[26], 2018 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Manrique et al[10], 2017 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Anoushiravani et al[30], 2016 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Husted et al[29], 2016 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Shaparin et al[28], 2016 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Zhao et al[31], 2014 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
| Thornqvist et al[32], 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Zhang et al[33], 2012 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
Operation duration (in min): The operation duration between UW (n = 2102) and NW (n = 55701) patients undergoing THA or TKA, was found to be not significantly different with MD: 1.66 95%CI: [-1.89, 5.21], P = 0.36. A subgroup analysis was carried out based on the type of procedure to analyze the heterogeneity (I2 = 75%). No difference in the result was observed in patients undergoing THA MD: 0.73 95%CI: [-3.31, 4.77]. P = 0.72 and TJA MD: 2.54 95%CI: [-3.59, 8.66], P = 0.42 (Figure 2).
Length of hospital stay (in days): The length of hospital stay after arthroplasty was found to be significantly higher for UW patients (n = 4555), when compared to NW patients (n = 58890). MD: 0.39 95%CI: [0.06, 0.72], P = 0.02, I2 = 81%.
The subgroup analysis showed no significant differences between UW and NW patients undergoing THA or TKA. However, in patients undergoing both THA and TKA, the length of hospital stay was found to be significantly higher for UW patients (n = 2207) MD: 0.76 95%CI: [0.43, 1.09], P < 0.0001. Low heterogeneity was also observed with an I2 value of 31% (Figure 3).
30-90-day readmission rate: No significant difference in readmission rate was observed between UW and NW patients undergoing THA or TKA with OR: 1.42 95%CI: [0.71, 2.87], P = 0.32; I2 = 36%. No subgroup differences were observed. UW patients (n = 408) undergoing THA presented with an increased OR: 1.75 95%CI: [0.58, 5.27], P = 0.32, I2 = 49% (not significant) of 30-90 d readmission compared to NW patients (Figure 4).
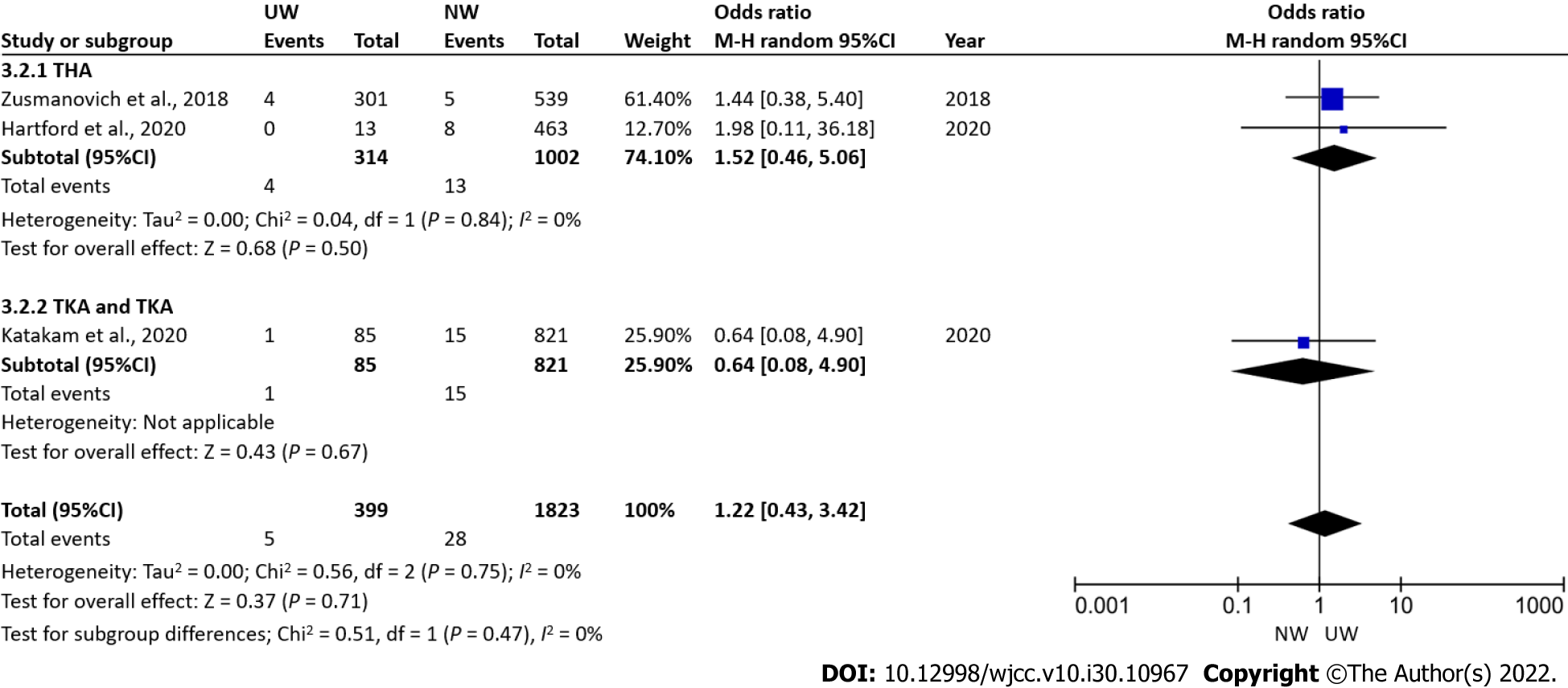
Re-operation rate: No significant difference in reoperation rate was observed between UW and NW patients undergoing THA with OR: 1.22 95%CI: [0.43, 3.42], P = 0.71; I2 = 0%. No subgroup differences were observed (Figure 5).
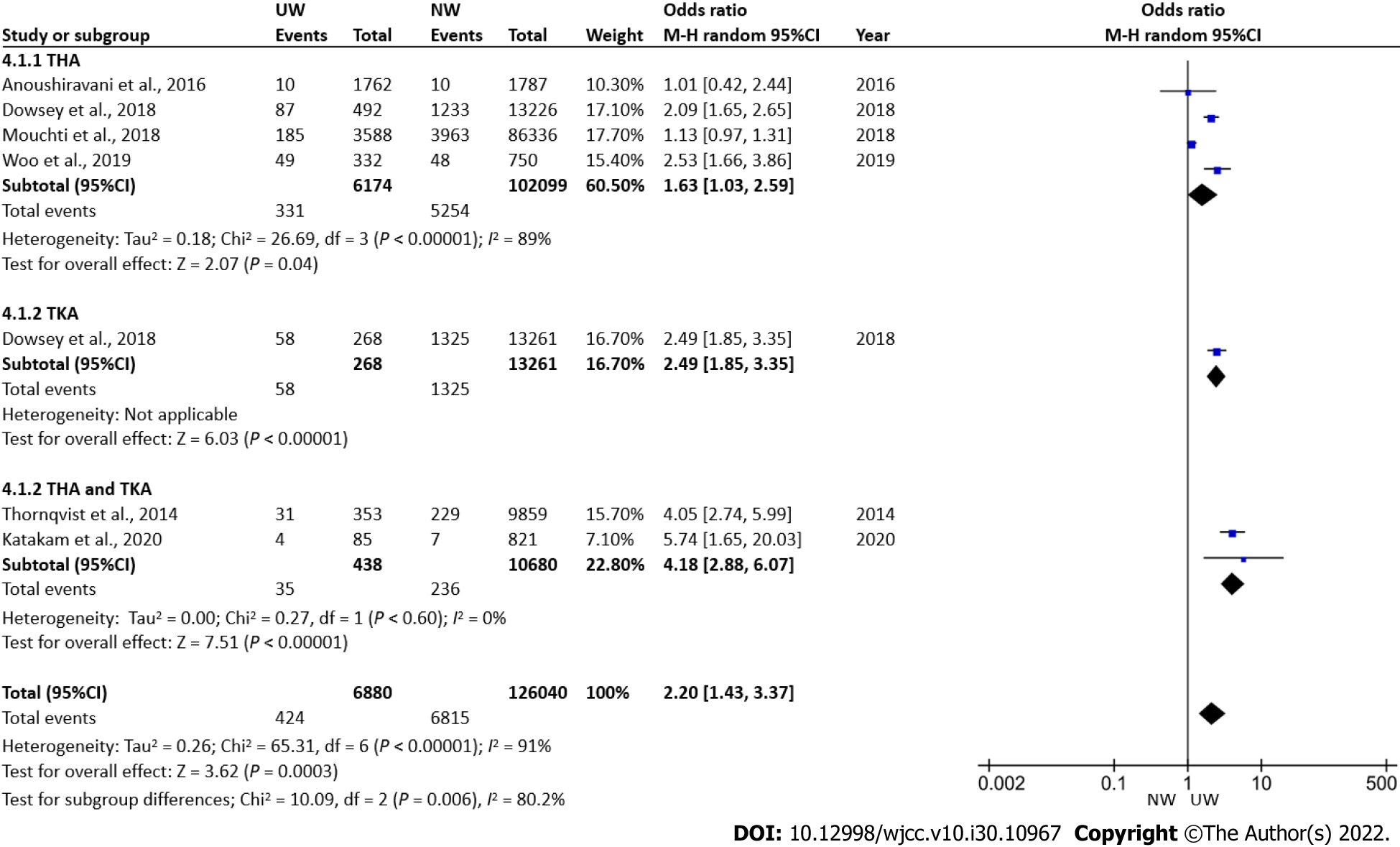
Post-operative mortality: UW patients (n = 6880) had higher odds of post-operative mortality than NW patients (126040) with OR: 2.20 95%CI: [1.43, 3.37], P = 0.0003. However, a high heterogeneity with an I2 value of 91% was observed. Following subgroup analysis, it was found that studies reporting THA and TKA together showed an increased incidence of mortality in UW patients (n = 438) OR: 4.18 95%CI: [2.88, 6.07], P < 0.0001 with I2 = 0%. Although not significant, the incidence of post-operative mortality was less likely to be observed in UW patients, compared to NW patients (Figure 6).
A subgroup analysis carried out based on timeframe showed higher 31-365 d mortality in UW patients with OR: 2.35 95%CI: [1.31, 3.54], P < 0.0001, I2 = 29%, than NW patients (Supplementary Figure 1).
Post-operative infection: No significant difference in the incidence of post-operative infection was observed between UW (n = 2955) and NW patients (n = 8261) undergoing THA or TKA with OR: 0.68 95%CI: [0.20, 16.29], P = 0.54; I2 = 51%. No subgroup differences were observed (Figure 7). The incidence of post-operative infection was lower (not significant) in UW patients, compared to NW patients.
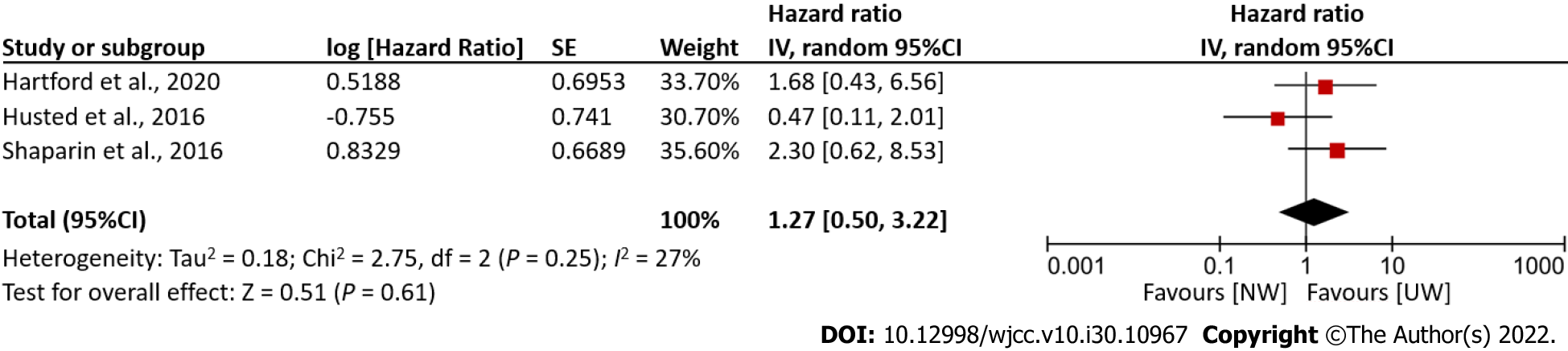
Total complications: No significant difference in hazard ratios computing total complications was observed between UW and NW patients. The incidence of total or overall complications observed between the two groups of patients undergoing arthroplasty was similar with HR: 1.27 95%CI: [0.50, 3.22], P = 0.61, I2 = 27% (Figure 8).
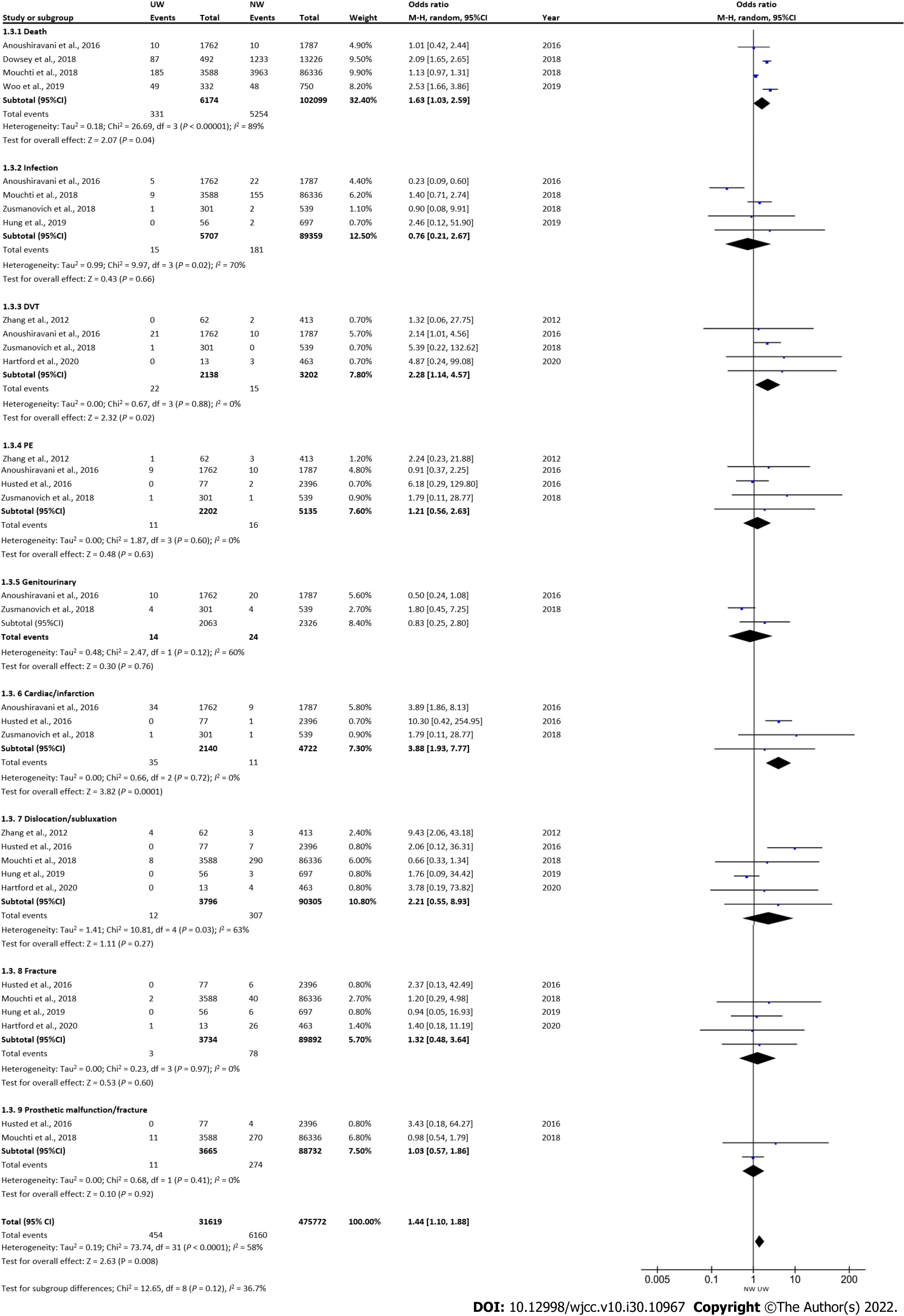
Post-operative complications in patients undergoing THA: UW patients (n = 31619) showed higher odds for the incidence of post-operative complications with OR: 1.44 95%CI: [1.10, 1.88], P = 0.008, I2 = 58%, in patients undergoing THA. Subsequently, a significantly higher incidence of DVT and cardiac infarction among the post-operative complications were observed in UW patients undergoing THA (Figure 9).
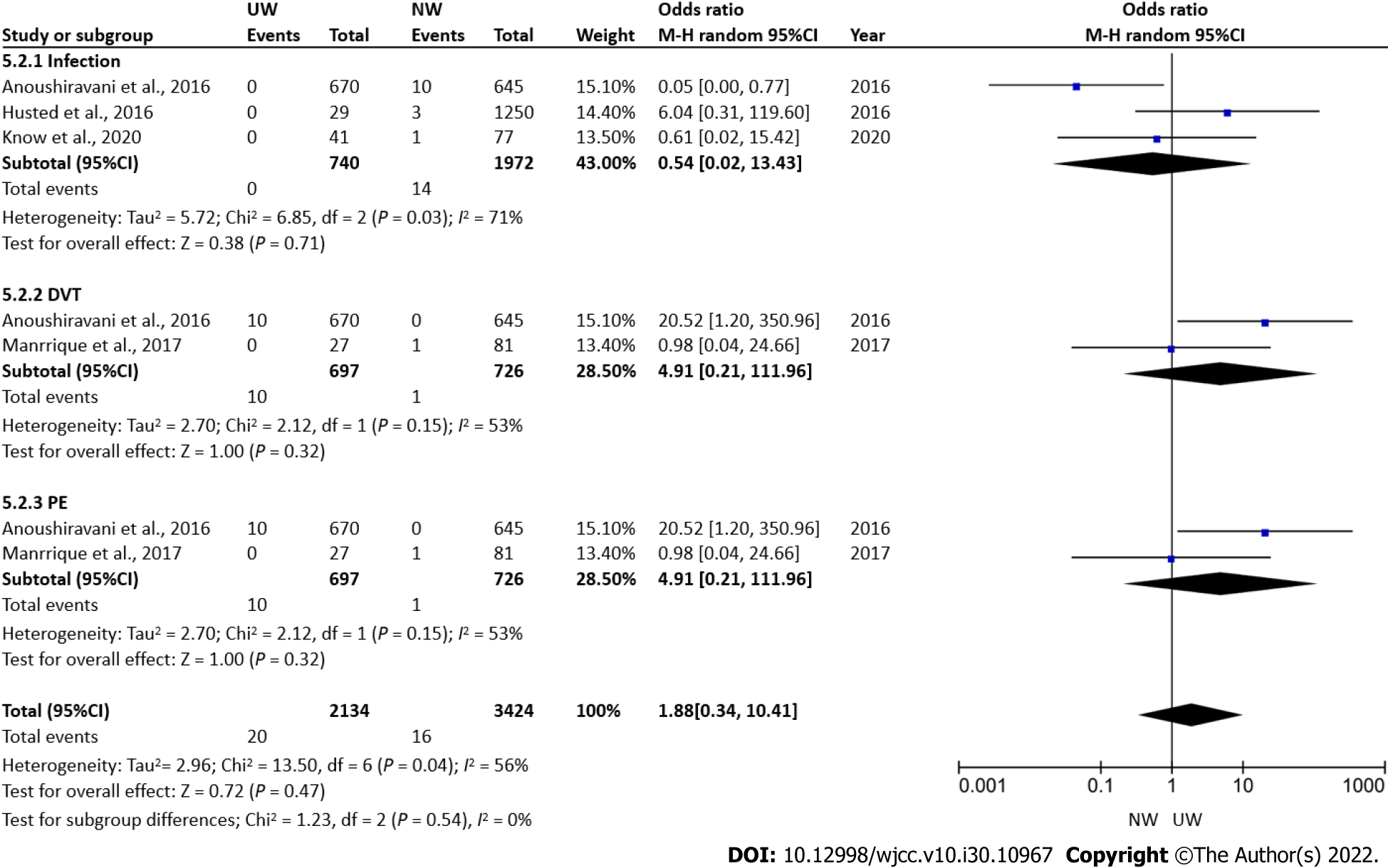
Post-operative complications in patients undergoing TKA: No significant difference in post-operative infection, DVT and pulmonary embolism was observed in UW (n = 2134) compared to NW (n = 3424) patients undergoing TKA with OR: 1.88 95%CI: [0.34, 10.41], P = 0.47, I2 = 56% (Figure 10).
This systematic review and meta-analysis included thirteen retrospective and five prospective cohort studies to compare UW and NW patients undergoing THA or TKA or TJA in terms of specific outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, DVT, pulmonary embolism, genito-urinary complications, dislocation/sub
Knee and hip osteoarthritis (OA) involves degeneration of articular cartilage, and bone hyperplasia of joint disease, is a common chronic disabling disease, causing physiological and psychological pain in patients[38]. OA is a common disease among the elderly, and elderly patients suffering from OA opt for arthroplasty for improved quality of life and morbidity-free life[39,40]. Modern-day arthroplasty includes the replacement of joints with a compatible metal prosthesis to restore function. TKA involves replacing the articular surfaces (femoral condyles and tibial plateau) of the knee joint with smooth metal and highly cross-linked polyethylene plastic[41,42]. THA involves the replacement of the acetabulum or hip socket, and the head of the femur is removed and replaced with a metal replica[43]. TJA involves both THA and TKA carried out simultaneously to manage OA complications. The prognosis after undergoing both procedures is good and is considered to improve quality of life by reducing pain and increasing function[44].
BMI is considered one of the key predictive tools for assessing outcomes after TKA or THA. An extreme BMI level is believed to worsen the prognosis and is associated with increased complications after TKA or THA. Many systematic reviews have assessed the effect of BMI on these procedures. According to a recent systematic review[45], BMI higher than normal can affect the intra-operative risk of TKA and post-operative recovery, and increase the risk of complications. Another review[46] concluded that increased BMI was associated with an increased risk of peri-prosthetic joint infection (PJI) after primary THA or TKA. Following THA, patients were more likely to suffer from PJI than TKA patients. All the systematic reviews and meta-analyses conducted have focused on the effect of obesity or patients with high BMI on various outcomes after undergoing THA or TKA. However, some studies have shown that even low BMI or UW patients have shown both peri-operative morbidity and poor post-operative recovery with complications. A study[47] that evaluated the readmission rate and post-operative infection in UW patients undergoing THA, demonstrated that patients with BMI < 18.5 kg/m2 were more likely to be associated with post-discharge infections and thereby increased readmission rates.
Most of the included studies classified underweight patients with a BMI < 18.5 kg/m2; however, a few studies such as those by Katakam et al[18] 2021 and Anoushiravani et al[30] 2016, used an up-bound cut-off of < 20 kg/m2 and < 19.5 kg/m2 to justify the fact that the present World Health Organization classification of BMI was set based on the findings in a young population and the included patients were elderly with a mean age of over 60 years.
The peri-operative outcomes assessed after undergoing arthroplasty include the operation duration and length of hospital stay. Our meta-analysis showed no significant difference in operation duration between UW and NW patients; however, the length of hospital stay after THA or TKA was found to be significantly higher for UW patients compared to NW patients with MD of 0.39 d 95%CI: [0.06, 0.72], P = 0.02. Poor nutritional status among UW patients leads to musculoskeletal degeneration characterized by less muscle mass, less soft tissue, and a greater probability of osteoporosis. A study in 2016[30] showed a higher proportion of UW patients with a length of hospital stay of more than 4 d compared to normal and obese patients. However, the mean difference of 0.39 d (= 9.4 h) for the length of hospital stay between UW and NW patients undergoing THA or TKA, though statistically significant, was not clinically significant. This negligible difference may be due to delay in discharge related to a system-level reason or inadequate staff availability.
Our systematic review did not find any significant differences in readmission and re-operation rates for both UW and NW patients undergoing THA or TKA or TJA. Although not significant, the 30-90 readmission rate was more likely to be observed in UW patients, compared to NW patients. This result cannot be regarded as sufficient certainty as the readmission rate is positively affected by various independent risk factors such as age, male sex, black race, presence of pre-operative co-morbidities, and increased operation time following TKA[48].
Our meta-analysis showed a significant association with post-operative mortality in UW patients OR: 2.20 95%CI: [1.43, 3.37]. UW patients can be malnourished, and often present with poor nutritional reserve. This may lead to a less pronounced immunological response. This may be a reasonable explanation for the higher incidence of post-operative mortality. The compromised immune response in these patients could trigger numerous debilitating diseases, leading to death. Additionally, patients undergoing both THA and TKA together showed an increased incidence of mortality with UW patients OR: 4.18 95%CI: [2.88, 6.07]. This could be explained by the fact that TJA (THA and TKA) is a more complicated surgery, with a higher incidence of complications than THA or TKA alone. A registry study[33] found U-shaped risk associations between BMI and perioperative cardiovascular events and mortality, which were highest in the UW group undergoing THA and TKA, suggesting that this was a subpopulation at risk.
Several authors have evaluated complications in UW patients; however, some of the reported data is controversial. Many authors suggest that UW patients have a higher complication rate than their NW or even obese counterparts. Our meta-analysis of included studies regarding post-operative complications showed a significantly higher incidence of DVT and cardiac infarction among the post-operative complications observed in UW patients undergoing THA alone. Three studies[11,24,31] showed that UW patients undergoing THA or TKA had increased risks for infection, cardiac complications, and venous thrombo-emboli. The reason for this is not entirely clear; however, in their studies, it appears that the UW group tended to have lower preoperative hematocrit and albumin which are markers of malnutrition and predispose patients to medical complications. Nowadays, autologous platelet concentrates[49-51] have been proved to be beneficial in the management of bone-related disorders[52-55]. They have also been used as an adjunct to arthroplasty[56,57]. Many studies have opted for this as an alternative to arthroplasty[58,59]. This can be used as an alternative to arthroplasty in less severe cases to improve the quality of life in UW patients.
Our systematic review and meta-analysis are the first to assess the impact of UW on peri-operative and post-operative outcomes of THA or TKA. However, our review also has certain limitations. Confounding factors such as age, presence of comorbidities including anemia, diabetes, hypertension, patients using anticoagulants, and preoperative use of any walking aids, were not taken into consideration to assess the peri-operative outcomes and readmission or reoperation rates. Moreover, no subgroup analysis could be performed based on follow-up time, especially on 30-d and 90-d readmission rates. The exclusion of articles other than the English language could also be a possible limitation as good evidence could have been missed.
UW patients undergoing THA or TKA had a higher incidence of post-operative complications and readmission rates. Moreover, UW patients undergoing TJA were associated with an increased incidence of mortality in the 31-365-d time frame. Also, a higher incidence of DVT and cardiac infarction was evident among all the post-operative complications in UW patients undergoing THA. No difference in post-operative complications was found in UW patients undergoing TKA. Hence, careful clinical judgment is needed by clinicians before UW patients undergo THA or TKA.
The effect of body mass index (BMI) on the outcomes and complications associated with total hip arthroplasty (THA) and total knee arthroplasty (TKA) is less studied and is believed to be a determining factor.
Systematic reviews on this issue have primarily focused on obesity compared to normal weight (NW). None of these reviews attempted to assess the effect of low BMI or underweight (UW) compared to NW in patients undergoing THA or TKA.
The objective of this review was to compare specific operative outcomes such as operation duration, length of hospital stay, and post-operative complications including mortality, infections, deep vein thrombosis, etc. along with rehospitalization and reoperation rates between UW and NW patients undergoing THA or TKA or both.
An electronic search was performed in PubMed, Scopus, Excerpta Medica database (EMBASE), Web of Science (WoS), and Cochrane Central Register of Controlled Trials (CENTRAL) along with a manual search. The quality of the studies was assessed using the Newcastle-Ottawa scale for cohort studies. The data were subjected to both qualitative and quantitative analysis.
Thirteen retrospective and five prospective cohort studies were included. The quality of included studies was assessed to be good to fair. The length of hospital stay after TKA or THA was found to be significantly higher for UW patients when compared to NW patients. Mean difference: 0.39 95%CI: [0.06, 0.72], P = 0.02 (in days). Studies presenting both THA and TKA together as total joint arthroplasty showed an increased incidence of mortality in patients who underwent THA or TKA alone with an odds ratio: 4.18 95%CI: [2.88, 6.07]. A higher incidence of post-operative complications was also observed in UW patients undergoing THA.
UW patients undergoing THA or TKA had a higher incidence of post-operative complications and were associated with a higher readmission rate. Moreover, UW patients were associated with an increased incidence of mortality in the studies that reported THA and TKA together.
Careful clinical judgment is needed by clinicians before UW patients undergo THA or TKA to attain better outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia; Solarino G, Italy; Velázquez-Saornil J, Spain S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Sun K, Li H. Body mass index as a predictor of outcome in total knee replace: A systemic review and meta-analysis. Knee. 2017;24:917-924. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Nuttall FQ. Body Mass Index: Obesity, BMI, and Health: A Critical Review. Nutr Today. 2015;50:117-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1039] [Cited by in F6Publishing: 982] [Article Influence: 109.1] [Reference Citation Analysis (0)] |
| 3. | Fruh SM. Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract. 2017;29:S3-S14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 191] [Cited by in F6Publishing: 287] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 4. | Wallace G, Judge A, Prieto-Alhambra D, de Vries F, Arden NK, Cooper C. The effect of body mass index on the risk of post-operative complications during the 6 months following total hip replacement or total knee replacement surgery. Osteoarthritis Cartilage. 2014;22:918-927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | George J, Piuzzi NS, Ng M, Sodhi N, Khlopas AA, Mont MA. Association Between Body Mass Index and Thirty-Day Complications After Total Knee Arthroplasty. J Arthroplasty. 2018;33:865-871. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 6. | Russo MW, Macdonell JR, Paulus MC, Keller JM, Zawadsky MW. Increased Complications in Obese Patients Undergoing Direct Anterior Total Hip Arthroplasty. J Arthroplasty. 2015;30:1384-1387. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Boyce L, Prasad A, Barrett M, Dawson-Bowling S, Millington S, Hanna SA, Achan P. The outcomes of total knee arthroplasty in morbidly obese patients: a systematic review of the literature. Arch Orthop Trauma Surg. 2019;139:553-560. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 100] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 8. | Lim YZ, Wang Y, Cicuttini FM, Giles GG, Graves S, Wluka AE, Hussain SM. Obesity defined by body mass index and waist circumference and risk of total knee arthroplasty for osteoarthritis: A prospective cohort study. PLoS One. 2021;16:e0245002. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Zusmanovich M, Kester B, Feng J, Schwarzkopf R. Postoperative complications in underweight patients undergoing total hip arthroplasty: A comparative analysis to normal weight patients. J Orthop. 2018;15:345-348. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Manrique J, Chen AF, Gomez MM, Maltenfort MG, Hozack WJ. Surgical site infection and transfusion rates are higher in underweight total knee arthroplasty patients. Arthroplast Today. 2017;3:57-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Molloy IB, Martin BI, Moschetti WE, Jevsevar DS. Effects of the Length of Stay on the Cost of Total Knee and Total Hip Arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99:402-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 183] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 12. | Foote J, Panchoo K, Blair P, Bannister G. Length of stay following primary total hip replacement. Ann R Coll Surg Engl. 2009;91:500-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Abdulla I, Mahdavi S, Khong H, Gill R, Powell J, Johnston KD, Sharma R. Does body mass index affect the rate of adverse outcomes in total hip and knee arthroplasty? Can J Surg. 2020;63:E142-E149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Elsiwy Y, Jovanovic I, Doma K, Hazratwala K, Letson H. Risk factors associated with cardiac complication after total joint arthroplasty of the hip and knee: a systematic review. J Orthop Surg Res. 2019;14:15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Pozzobon D, Ferreira PH, Blyth FM, Machado GC, Ferreira ML. Can obesity and physical activity predict outcomes of elective knee or hip surgery due to osteoarthritis? BMJ Open. 2018;8:e017689. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Onggo JR, Onggo JD, de Steiger R, Hau R. Greater risks of complications, infections, and revisions in the obese versus non-obese total hip arthroplasty population of 2,190,824 patients: a meta-analysis and systematic review. Osteoarthritis Cartilage. 2020;28:31-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 17. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12640] [Cited by in F6Publishing: 12184] [Article Influence: 812.3] [Reference Citation Analysis (0)] |
| 18. | Katakam A, Melnic CM, Bragdon CR, Sauder N, Collins AK, Bedair HS. Low Body Mass Index Is a Predictor for Mortality and Increased Length of Stay Following Total Joint Arthroplasty. J Arthroplasty. 2021;36:72-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Kwon HM, Han CD, Yang IH, Lee WS, Kim CW, Park KK. Being Underweight Is Associated with Worse Surgical Outcomes of Total Knee Arthroplasty Compared to Normal Body Mass Index in Elderly Patients. Orthop Res Rev. 2020;12:53-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Hartford JM, Graw BP, Frosch DL. Perioperative Complications Stratified by Body Mass Index for the Direct Anterior Approach to Total Hip Arthroplasty. J Arthroplasty. 2020;35:2652-2657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Woo SH, Cha DH, Park EC, Kim SJ. The association of under-weight and obesity with mortality after hip arthroplasty. Age Ageing. 2019;48:94-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Sloan M, Sheth N, Lee GC. Is Obesity Associated With Increased Risk of Deep Vein Thrombosis or Pulmonary Embolism After Hip and Knee Arthroplasty? Clin Orthop Relat Res. 2019;477:523-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 23. | Sayed-Noor AS, Mukka S, Mohaddes M, Kärrholm J, Rolfson O. Body mass index is associated with risk of reoperation and revision after primary total hip arthroplasty: a study of the Swedish Hip Arthroplasty Register including 83,146 patients. Acta Orthop. 2019;90:220-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 24. | Hung CY, Chang CH, Lin YC, Lee SH, Chen SY, Hsieh PH. Predictors for Unfavorable Early Outcomes in Elective Total Hip Arthroplasty: Does Extreme Body Mass Index Matter? Biomed Res Int. 2019;2019:4370382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Shohat N, Fleischman A, Tarabichi M, Tan TL, Parvizi J. Weighing in on Body Mass Index and Infection After Total Joint Arthroplasty: Is There Evidence for a Body Mass Index Threshold? Clin Orthop Relat Res. 2018;476:1964-1969. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Mouchti S, Whitehouse MR, Sayers A, Hunt LP, MacGregor A, Blom AW. The Association of Body Mass Index with Risk of Long-Term Revision and 90-Day Mortality Following Primary Total Hip Replacement: Findings from the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J Bone Joint Surg Am. 2018;100:2140-2152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Dowsey MM, Choong PFM, Paxton EW, Spelman T, Namba RS, Inacio MCS. Body Mass Index Is Associated With All-cause Mortality After THA and TKA. Clin Orthop Relat Res. 2018;476:1139-1148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Shaparin N, Widyn J, Nair S, Kho I, Geller D, Delphin E. Does the obesity paradox apply to early postoperative complications after hip surgery? J Clin Anesth. 2016;32:84-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Husted H, Jørgensen CC, Gromov K, Kehlet H; Lundbeck Foundation Center for Fast-track Hip and Knee Replacement Collaborative Group. Does BMI influence hospital stay and morbidity after fast-track hip and knee arthroplasty? Acta Orthop. 2016;87:466-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 30. | Anoushiravani AA, Sayeed Z, Chambers MC, Gilbert TJ, Scaife SL, El-Othmani MM, Saleh KJ. Assessing In-Hospital Outcomes and Resource Utilization After Primary Total Joint Arthroplasty Among Underweight Patients. J Arthroplasty. 2016;31:1407-1412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Zhao J, Li J, Zheng W, Liu D, Sun X, Xu W. Low body mass index and blood loss in primary total hip arthroplasty: results from 236 consecutive ankylosing spondylitis patients. Biomed Res Int. 2014;2014:742393. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Thornqvist C, Gislason GH, Køber L, Jensen PF, Torp-Pedersen C, Andersson C. Body mass index and risk of perioperative cardiovascular adverse events and mortality in 34,744 Danish patients undergoing hip or knee replacement. Acta Orthop. 2014;85:456-462. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 33. | Zhang ZJ, Zhao XY, Kang Y, Zhang ZQ, Yang ZB, He AS, Fu M, Sheng PY, Liao WM. The influence of body mass index on life quality and clinical improvement after total hip arthroplasty. J Orthop Sci. 2012;17:219-225. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Roth A, Anis HK, Emara AK, Klika AK, Barsoum WK, Bloomfield MR, Brooks PJ, Higuera CA, Kamath AF, Krebs VE, Mesko NW, Murray TG, Muschler GF, Nickodem RJ, Patel PD, Schaffer JL, Stearns KL, Strnad G, Warren JA, Zajichek A, Mont MA, Molloy RM, Piuzzi NS; Cleveland Clinic OME Arthroplasty Group. The Potential Effects of Imposing a Body Mass Index Threshold on Patient-Reported Outcomes After Total Knee Arthroplasty. J Arthroplasty. 2021;36:S198-S208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 35. | Murgatroyd SE, Frampton CM, Wright MS. The effect of body mass index on outcome in total hip arthroplasty: early analysis from the New Zealand Joint Registry. J Arthroplasty. 2014;29:1884-1888. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Guan Z, Chen Y, Song Y. [Influence of body mass index and age on deep vein thrombosis after total hip and knee arthroplasty]. Zhongguo Xiufu Chongjian Waike Zazhi. 2006;20:611-615. [Cited in This Article: ] |
| 37. | Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I. Caspian J Intern Med. 2011;2:205-212. [PubMed] [Cited in This Article: ] |
| 38. | Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. 2008;168:1430-1440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 114] [Cited by in F6Publishing: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 39. | Katz JN, Arant KR, Loeser RF. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA. 2021;325:568-578. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 634] [Cited by in F6Publishing: 688] [Article Influence: 229.3] [Reference Citation Analysis (0)] |
| 40. | Softness KA, Murray RS, Evans BG. Total knee arthroplasty and fractures of the tibial plateau. World J Orthop. 2017;8:107-114. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 35] [Cited by in F6Publishing: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 41. | Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total knee arthroplasty: improving outcomes with a multidisciplinary approach. J Multidiscip Healthc. 2018;11:63-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 42. | Varacallo M, Luo TD, Johanson NA. Total Hip Arthroplasty Techniques. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2021 Available from: http://www.ncbi.nlm.nih.gov/books/NBK507864/. [Cited in This Article: ] |
| 43. | Bumpass DB, Nunley RM. Assessing the value of a total joint replacement. Curr Rev Musculoskelet Med. 2012;5:274-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Wang H, Qiong M, Ma B. Analysis of the influence of BMI on the outcome after total knee arthroplasty. IJS Glob Health. 2021;4:e55. [DOI] [Cited in This Article: ] |
| 45. | Zhong J, Wang B, Chen Y, Li H, Lin N, Xu X, Lu H. Relationship between body mass index and the risk of periprosthetic joint infection after primary total hip arthroplasty and total knee arthroplasty. Ann Transl Med. 2020;8:464. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 46. | Alfonso DT, Howell RD, Caceres G, Kozlowski P, Di Cesare PE. Total hip arthroplasty in the underweight. J Arthroplasty. 2008;23:956-959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 47. | Lehtonen EJ, Hess MC, McGwin G Jr, Shah A, Godoy-Santos AL, Naranje S. RISK FACTORS FOR EARLY HOSPITAL READMISSION FOLLOWING TOTAL KNEE ARTHROPLASTY. Acta Ortop Bras. 2018;26:309-313. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Panda S, Mishra L, Arbildo-Vega HI, Lapinska B, Lukomska-Szymanska M, Khijmatgar S, Parolia A, Bucchi C, Fabbro MD. Effectiveness of Autologous Platelet Concentrates in Management of Young Immature Necrotic Permanent Teeth-A Systematic Review and Meta-Analysis. Cells. 2020;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 49. | Panda S, Satpathy A, Chandra Das A, Kumar M, Mishra L, Gupta S, Srivastava G, Lukomska-Szymanska M, Taschieri S, Del Fabbro M. Additive Effect of Platelet Rich Fibrin with Coronally Advanced Flap Procedure in Root Coverage of Miller's Class I and II Recession Defects-A PRISMA Compliant Systematic Review and Meta-Analysis. Materials (Basel). 2020;13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 50. | Panda S, Purkayastha A, Mohanty R, Nayak R, Satpathy A, DAS AC, Kumar M, Mohanty G, Panda S, Fabbro MD. Plasma rich in growth factors (PRGF) in non-surgical periodontal therapy: a randomized clinical trial. Braz Oral Res. 2020;34:e034. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 51. | Panda S, Doraiswamy J, Malaiappan S, Varghese SS, Del Fabbro M. Additive effect of autologous platelet concentrates in treatment of intrabony defects: a systematic review and meta-analysis. J Investig Clin Dent. 2016;7:13-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 52. | Del Fabbro M, Lolato A, Panda S, Corbella S, Satpathy A, Das AC, Kumar M, Taschieri S. Methodological Quality Assessment of Systematic Reviews on Autologous Platelet Concentrates for the Treatment of Periodontal Defects. J Evid Based Dent Pract. 2017;17:239-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 53. | Del Fabbro M, Karanxha L, Panda S, Bucchi C, Nadathur Doraiswamy J, Sankari M, Ramamoorthi S, Varghese S, Taschieri S. Autologous platelet concentrates for treating periodontal infrabony defects. Cochrane Database Syst Rev. 2018;11:CD011423. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 54. | Panda S, Ramamoorthi S, Jayakumar ND, Sankari M, Varghese SS. Platelet rich fibrin and alloplast in the treatment of intrabony defect. J Pharm Bioallied Sci. 2014;6:127-131. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | Safdar A, Shaaban H, Tibayan R, Miller R, Boairdo R, Guron G. The clinical efficacy of using autologous platelet rich plasma in hip arthroplasty: A retrospective comparative study. J Nat Sci Biol Med. 2015;6:49-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 56. | Guerreiro JP, Danieli MV, Queiroz AO, Deffune E, Ferreira RR. Platelet-rich plasma (PRP) applied during total knee arthroplasty. Rev Bras Ortop. 2015;50:186-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Prodromos C, Finkle S. Autologous Biologic Treatment with Fat, Bone Marrow Aspirate and Platelet Rich Plasma Is an Effective Alternative to Total Knee Arthroplasty for Patients with Moderate Knee Arthrosis. Medicines (Basel). 2020;7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Sánchez M, Jorquera C, Sánchez P, Beitia M, García-Cano B, Guadilla J, Delgado D. Platelet-rich plasma injections delay the need for knee arthroplasty: a retrospective study and survival analysis. Int Orthop. 2021;45:401-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 59. | Pace TB, Foret JL, Palmer MJ, Tanner SL, Snider RG. Intraoperative platelet rich plasma usage in total knee arthroplasty: does it help? ISRN Orthop. 2013;2013:740173. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |