Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.10873
Peer-review started: August 7, 2022
First decision: August 17, 2022
Revised: August 26, 2022
Accepted: September 20, 2022
Article in press: September 20, 2022
Published online: October 26, 2022
The World Health Organization (WHO) called the recent monkeypox (MPX) outbreak a Public Health Emergency of International Concern on July 23, 2022. The United States of America (US) alarmed the recent MPX outbreak as the US public health emergency on August 4, 2022. Since early May 2022, more than 35000 MPX cases and 12 deaths had been reported to WHO from 92 countries and territories by August 17, 2022, and MPX cases continue rising rapidly with improved surveillance, access to diagnosis, and continuous virus spreading globally. Approximately 99% MPX cases are men, of which 95% cases are men who have sex with man. No evidence of MPX being sexually transmitted infec
Core Tip: The World Health Organization called the current monkeypox (MPX) outbreak a Public Health Emergency of International Concern on 23 July, 2022. United States (US) alarmed the recent MPX outbreak as the US public health emergency on August 4, 2022. Despite MPX cases continue to rise rapidly with improved surveillance, as MPX outbreaks is primarily contained in adult men, it should be manageable, and will be controlled by education, MPX surveillance, careful monitoring, vaccination, and crossborder collaborations with international sectors.
- Citation: Ren SY, Li J, Gao RD. 2022 Monkeypox outbreak: Why is it a public health emergency of international concern? What can we do to control it? World J Clin Cases 2022; 10(30): 10873-10881
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/10873.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.10873
The World Health Organization (WHO) announced the recent global outbreak of monkeypox (MPX) a public health emergency on July 23, 2022[1-3]. Since May, 2022, more than 35000 MPX cases and 12 deaths had been reported to WHO, from 92 countries and territories by August 17, 2022[4], where the MPX virus is not endemic. Previous cases of MPX found in non-endemic regions were usually related with travel to Central or West Africa, however, cases in recent outbreak appear to have no link with endemic areas that suggests community transmission[3]. It is timely to know the transmissibility and available preventive approaches to obtain the outbreak of MPX.
The references were systematically searched and reviewed on the Internet homepage of the National Library of Medicine, web of science without language limitations. The search covered all years available on the internet. The search terms were applied as follows: Monkeypox, outbreak, Public Health Emergency of International Concern vaccination, Infectivity, Transmission, and Man who have sex with man. The citations in each article found during the main search were researched for potential relevance. Published articles were included and reviewed, the related results were extracted given they provided original data on monkeypox.
MPX is a rare zoonotic disease in humans, induced by the MPX virus that is alike to other ortho
The natural hosts of MPX virus are rodents such as squirrels and giant pouched rats, which stand for the largest animal reservoirs for the virus[1]. MPX usually spreads through intimate touch with infected skin or mucosal lesions, body fluids and blood, and polluted personal clothes[3,6-10]. Outbreaks occur occasionally in sub-Saharan Africa after contacting with an infected wild animal. Outside of Africa, the largest known outbreak in the United States (US) happened in 2003, when 47 cases were infected by pet prairie dogs that had contaminated the virus from rodents imported from Ghana[1,9]. In Belgium, many MPX cases were related to a gay festival in Antwerp. The virus can be detected in semen[10,11], most MPS cases have lesions exclusively perigenital, perianal, and around the mouth[10,12].
Recent epidemiologic study shows that the main mode of transmission is through skin-to-skin and sexual contact, rather than contact with polluted clothes. Currently, US and most of the European (EU) countries are epidemic countries[3,6-8]. Reported cases in recent outbreak have mainly but not exclusively been identified among men who have sex with men (MSM), particularly those with new or multiple partners, and bisexual men between the ages of 20-59 years, 99% cases are men, of which 95% cases are MSM[13,14].
Whether monkeypox is STIs, infected from person to person through blood, semen or other bodily fluids during sex, is unclear yet. But several studies indicate that DNA from MPX virus is present in semen for weeks after infection. Infectious viruses were isolated from semen six days after their symptoms appeared. In United Kingdom (UK)[10], all 54 men being confirmed MPX infection were identifying as MSM, with a median age of 41 years, and 13 (24%) were living with human immunodeficiency virus (HIV)[10]. In Spain, 147 specimens were picked up from 12 patients and tested by real-time polymerase chain reaction (PCR). MPX DNA was identified in saliva, rectal swab, nasopharyngeal swab, semen, urine and faeces[15]. In Italy, four PMX cases of young adult men informing condomless sexual intercourse are healthy necessitating no specific antiviral therapy, MPX DNA were tested positive in seminal fluid[16]. In Germany, first two human MPX patients demonstrate clinical and virological findings, revealing MPX DNA in blood and semen[17]. The close contact during sexual activity may spread virus easier, it is most likely a accidental introduction of MPX which then spread among MSM[10]. Now there is not enough evidence to call PMX a STI. The possibility of sexual transmission of MPX virus needs to be confirmed[16].
MPX has an incubation time ranging from 5 to 21 d, most cases develop symptoms 6-13 d after the first contact[1,9]. MPX is generally a self-limited febrile rash of limited severity, and most patients are mild, and recover within a few weeks, usually have fever, chills, headaches fatigue, muscle pain, and enlargement of lymph node followed by an eruption of pus-filled blisters. Within 5 d after fever, a variety of sizes of rashes build up from the face to the trunk and extremities. The rashes often come out on the palms and soles of the feet with size of 0.5-1 cm in diameter, resolving into crusts then falling off[1,9]. The median time between symptom onset and diagnosis was 7 d[13].
More serious cases can be found in children, elderly, pregnant women and immunocompromised patients[17], who may have many complications, such as respiratory disorders and encephalitis. Death usually occurs within the second week of the infection[17,18].
The MPX genome has more than 200000 base pairs, is approximately seven times the size of severe acute respiratory coronavirus 2 (SARS-CoV-2)’s and more than 20 times longer than HIV’s. As MPX virus is a DNA virus, MPX has far better genetic repair mechanisms than RNA viruses such as HIV and SARS-CoV-2, which hints at it evolves more slowly[6,10]. Although smallpox viruses belong to the genus orthopoxvirus, but the infectivity and pathogenicity of MPX virus are weaker than smallpox virus. The fatality rate of smallpox can reach 30%, the fatality rate of MPX in Central Africa (the Congo Basin strain) is about 10.6%, and that in West Africa is around 3.6%. The mortality rate of MPX cases reported worldwide in 2022 was about 0.03%, and the eight reported deaths were all in Africa. As of May 2022, the Democratic Republic of the Congo was the country with the highest number of cases and deaths with 1284 verified cases between January 1, 2022 and May 8, 2022, including 58 deaths[19].
More than 35000 MPX cases and 12 deaths had been informed to WHO from 92 countries and territories by August 17, 2022[3,6-9,14,20].
Symptoms do not have any specific characteristics, but help establish the suspicion of MPX. The enlarged lymph nodes are uncommon signal of smallpox, but occur in 90% of MPX distributed in the neck, the groin and submandibular areas[1,18]. They are considered a distinctive hallmark indicating MPX. Diagnosis is made initially with a pan-orthopox PCR then by a specific MPX PCR test and genome sequencing[10]. IgM is more useful in diagnosing newly infectious cases, while IgG itself cannot provide a definitive diagnosis for a patient infected with orthopoxvirus[21]. As the symptoms are various and non-specific, many disorders can be included in a differential diagnosis of MPX, e.g. sexual transmitted infections (STIs), chickenpox, syphilis, water warts, red measles, drug reactions, staphylococcus skin infections, bacillus anthracis, and itch mites[6,9]. Community transmission happened several times globally without recognition may be misdiagnosis of MPX as STIs especially as it showed with atypical genital and peri-anal lesions, mild or asymptomatic cases, non-reporting of cases, and a dearth of active surveillance. Another reason is the population’s withdrawing protection from smallpox vaccines. Smallpox, being in the same family as MPX, was eradicated in the 1980s through mass vaccination. The lack of immunity in young people allows them easier to get MPX[9,10].
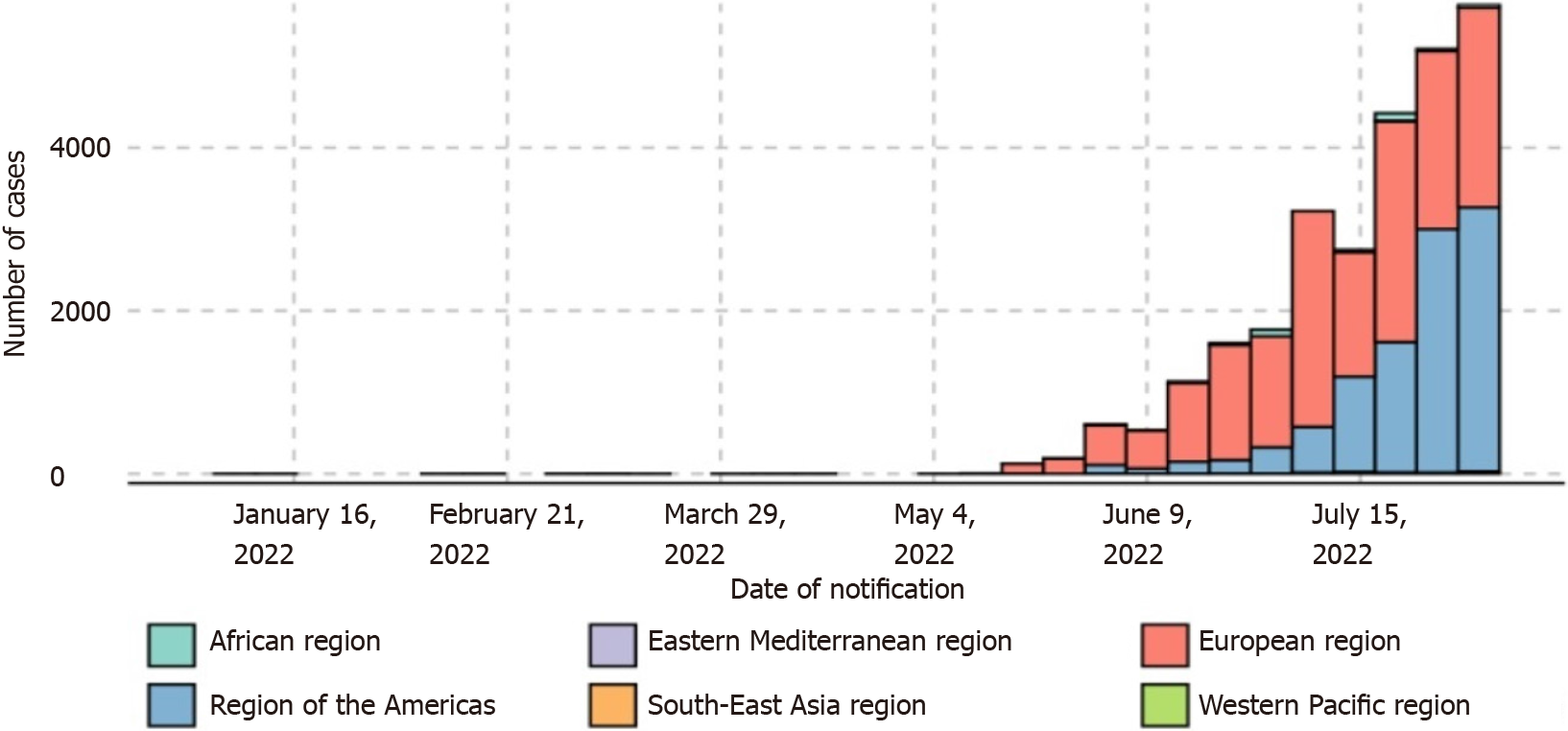
A disease outbreak is endemic when it is consistently present but limited to a particular geographic area or region. WHO classified some African countries such as Cameroon, the Central African Republic, the Democratic Republic of the Congo, and Nigeria, as MPX endemic. Previous MPX cases in non-endemic regions were usually related with travel to Central or West Africa[18]. But, since early May 2022 an unique outbreak of MPX from non-endemic countries has been reported to WHO globally (Figure 1), US and most EU become endemic, global spread is clearly a concern, and requires collaborative international efforts[9].
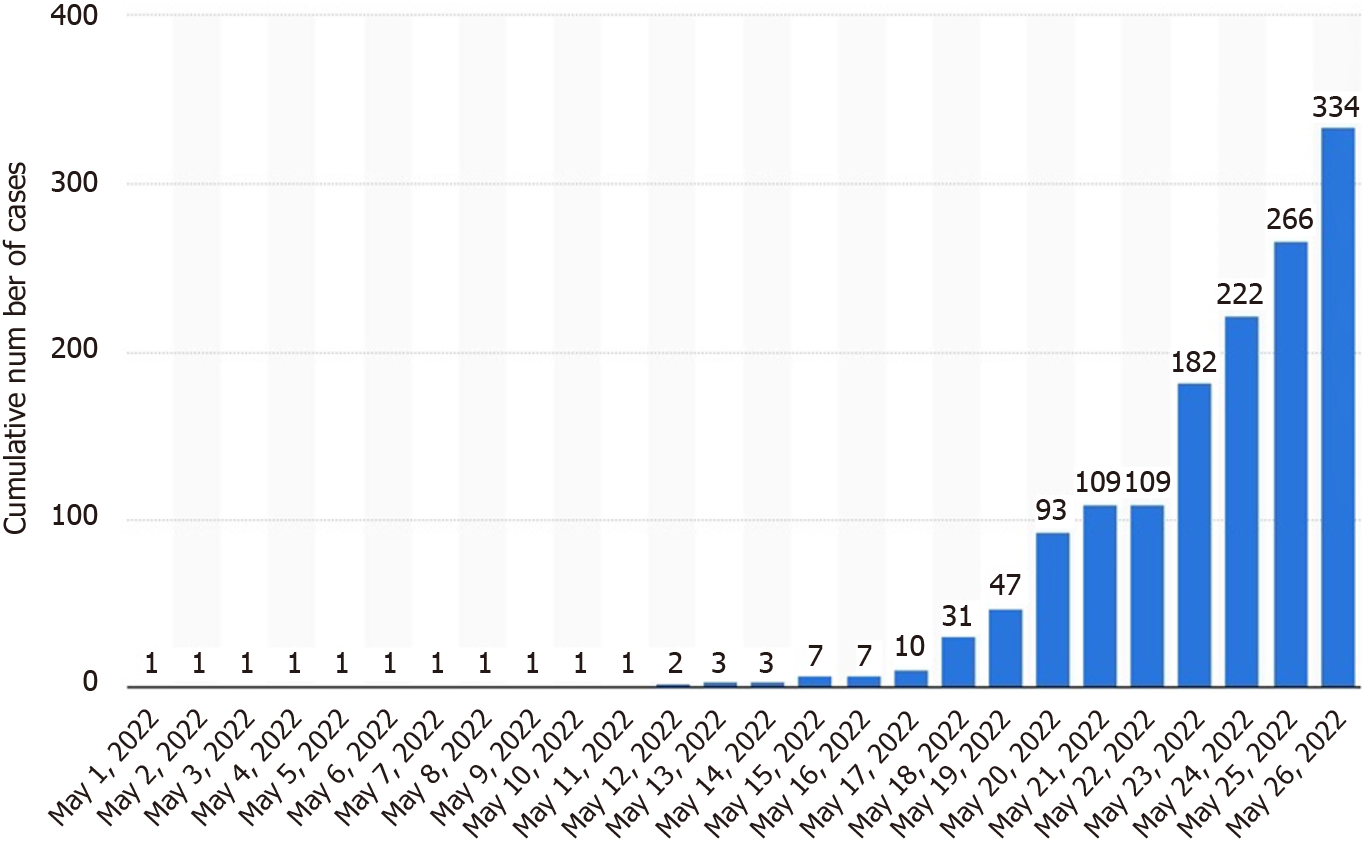
May 6, 2022 an outbreak of MPX was proved in the UK, coming from a British resident who had travelled to Nigeria, the endemic area, inducing the index case of the outbreak into the UK[3,5]. As of May 22, 2022, 92 cases from 15 non-endemic countries have been confirmed worldwide[9]. As of May 26, the number increased to 334[19] (Figure 2).
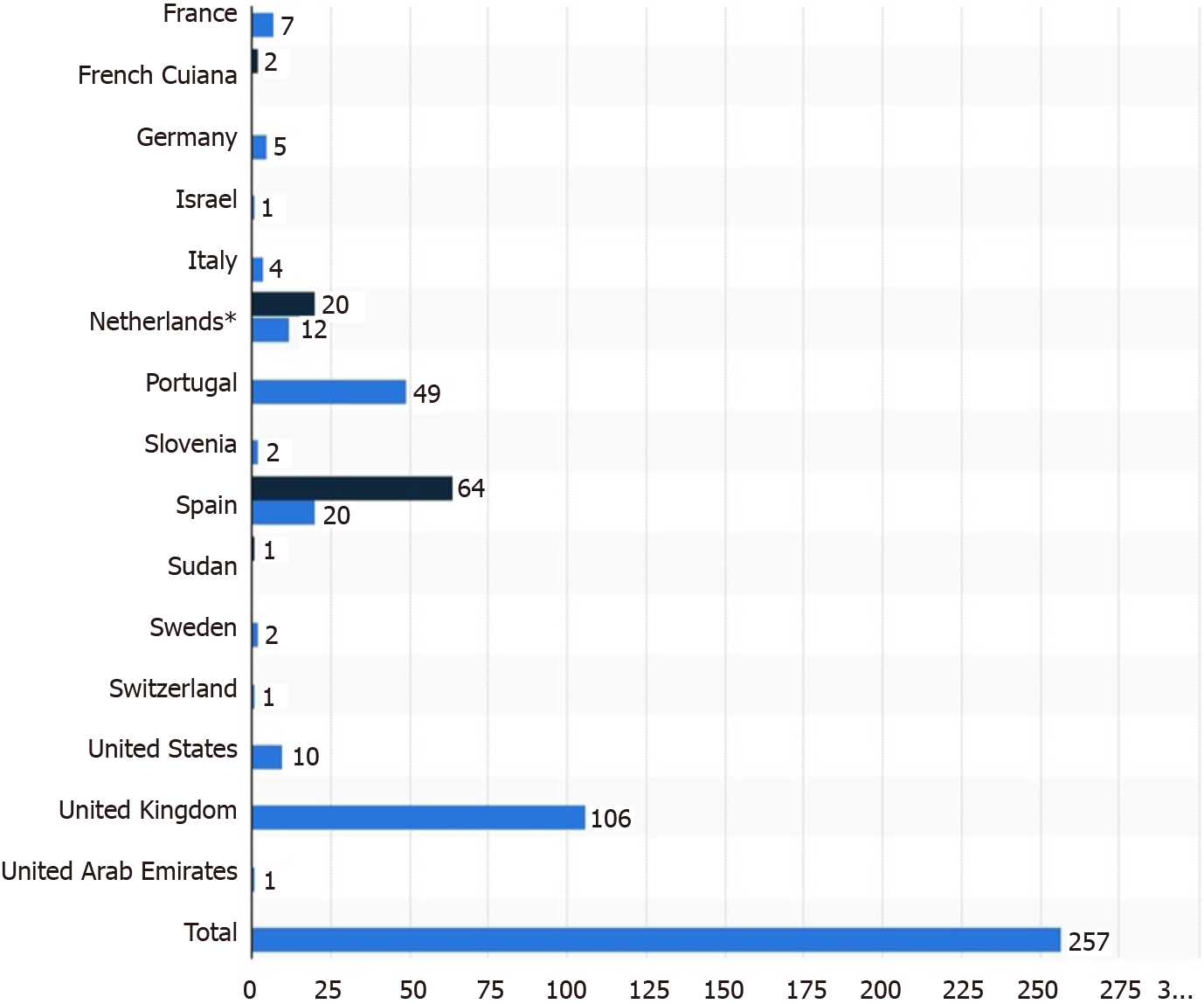
MPX is endemic to some African countries and usually came up outside this region only when related to travelers. The current outbreak, mostly in some Western countries, has no evidence of travel history to endemic areas suggesting community transmission[14]. The countries reporting the highest number of confirmed cases were the UK, Portugal, and Canada. Figure 3 shows the number of confirmed and suspected cases of MPX in non-endemic countries that had been reported to the WHO between May 13, 2022 and 26, 2022[19].
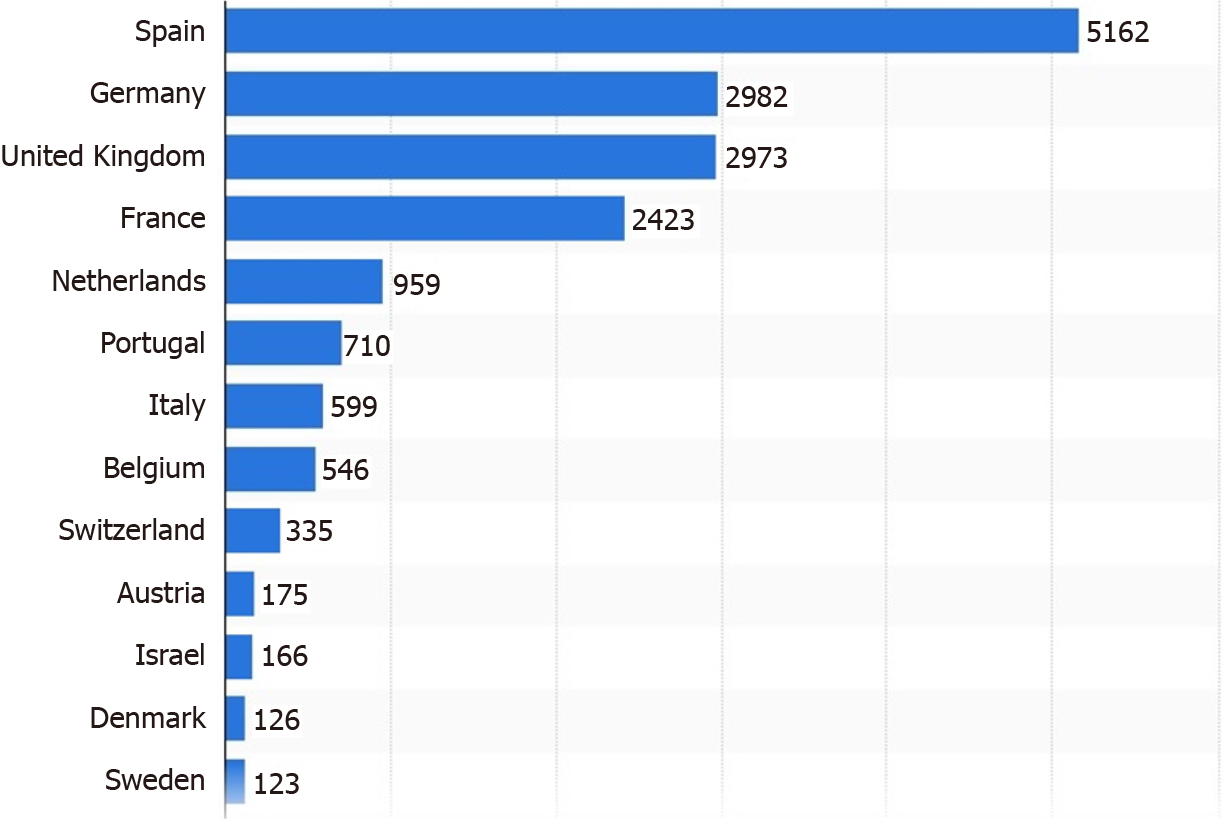
On the afternoon of June 23, 2022, 3040 cases had been reported in 47 countries and regions, the WHO emergency committee held an expert meeting to evaluate the risk of MPX outbreaks in the world, only three members were for declaring a "public health emergency of international concern" (PHEIC) and 11 were opposed, therefore, the alarm of PHEIC was not sounding[22]. As of August 10, 2022, 41 countries across Europe had reported confirmed MPX cases, 5162 cases in Spain, while 2982 cases in the UK (Figure 4).
On the afternoon of July 21, 2022, 75 countries and regions, mainly in non-endemic area such as Europe and North America had reported more than 16000 cases including 5 deaths, the WHO emer
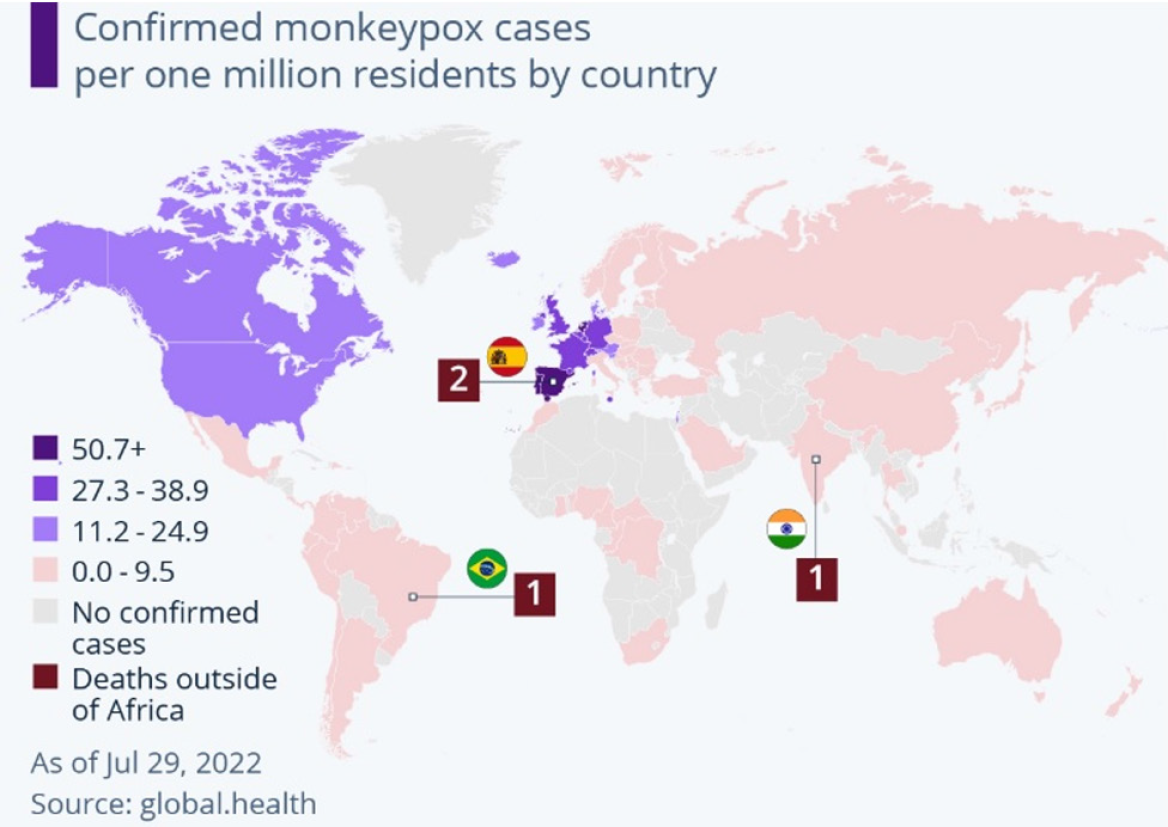
The worldwide number of MPX cases has risen to 21099 as of July 29, 2022 according to data by global.health, while mortality is not a concern yet (Figure 5). A total of 19429 cases of MPX have been found from 43 countries and areas throughout the European region through The European Surveillance System (TESSy), up to August 16, 2022[13]. The majority of cases were between 31 and 40 years-old (40%) and male (98.9%). Among cases with known HIV status, 38% (2749/7322) were HIV-positive. The majority of cases have rash (77.1%) and systemic symptoms such as fever, fatigue, muscle pain, chills, or headache (65%). 505 cases were hospitalized (5.8%), of which 179 cases demanded clinical care. Three cases were admitted to intensive care unit, of which, one was unrelated to MPX infection, the other two died of MPX later[13]. On August 4, 2022, a total of 26800 cases of MPX had been documented globally, at least 7100 cases MPX were identified in US, the largest number of confirmed cases in the world. Therefore, the US alarmed the MPX outbreak as the US public health emergency. By August 22, 2022 there had been 15432 cases in the US, the highest number in the world.
However, MPX has a much less serious threat of a massive global pandemic than coronavirus disease 2019 (COVID-19). Unlike COVID-19, MPX does not transmit human to human very easily through the air like COVID-19, and is not contagious until the MPX case becomes symptomatic, that makes it much easier to isolate and prevent the spread of MPX cases.
Education, MPX surveillance, diligent monitoring, vaccination, and crossborder collaborations with international sectors are practical strategy to contain MPX outbreaks. People are educated to reduce the risk of exposure and to reduce the number of sexual partners especially new ones, to avoid close contacting travelers from epidemic areas or animals that may carry MPX virus. Virus spreading among MSM populations can be broken through aggressive public health measures, including increased vaccination and investigative testing and extensive education campaigns aimed at high risk persons and reducing social stigma[23-25].
It is critical to educate people and to identify, isolate and treat cases early and to shot vaccine for high risk persons. In case of rash and other symptoms, one should consult with a doctor and inform the travel history. To promptly recognize MPX cases and avoid further transmission, medical workers should be alert of the travel or contact history of the cases with similar symptoms[26].
MPX virus is closely related to smallpox virus. Due to cross immunization, smallpox vaccination with vaccinia virus was about 85% protective against MPX[9]. Nevertheless, the vaccine called vaccinia contains a natural pox virus cultured in labs. Vaccinia replicates inside the recipient and sometimes induced severe side effects, even one death in 1 million vaccinated people[3].
As to date no specific treatment for MPX is available. Since most cases of MPX are mild and self-limited disease, and can be treated with supportive care[9]. The vaccination was key to the success of the smallpox eradication campaign. Centers for Disease Control and Prevention recommends giving the smallpox vaccine within 4 d of exposure which may avoid the MPX disease, and within 2 wk to minimize symptoms[9]. Currently available vaccines for preexposure prophylaxis against orthopoxvirus infection among persons at risk include ACAM2000® (live, replication competent vaccinia virus), JYNNEOS (live, replication incompetent vaccinia virus) in US and EU, IMVAMUNE in Canada, IMVANEX in Europe, CJ-50300 in Korea, and LC16M8 in Japan. The two-dose MVA-BN JYNNEOS marked in US is same product of IMVANEX in Europe and IMVAMUNE in Canada that all manufactured by Bavarian Nordics[9].
Bavarian Nordic JYNNEOS smallpox (Monkeypox) vaccine is established on a live, attenuated vaccinia virus, modified vaccinia ankara that is cultured in chicken embryo fibroblast cells and a serum-free medium, it cannot replicate in the human body, and can elicit a potent immune response. The US Food and Drug Administration (FDA) explicitly approved JYNNEOS vaccine for both smallpox and MPX in adults 18 years of age and older verified to be at high risk for infection. JYNNEOS cannot replicate in the human, it needs two doses given 4 wk apart, it is efficient and safe in people infected with HIV or atopic dermatitis[9]. Exactly how well modified vaccinia virus ankara protects against monkeypox and for how long is unknown. Nor is it clear how much protection is lost by administering only a single dose rather than the suggested two doses, because some regions are short of vaccine supply, or how much protection a vaccine given after exposure can provide[9].
The ACAM2000 vaccine is licensed by the US FDA for smallpox and permitted to prevent MPX on an expanded access basis (“compassionate use” for an investigational drug use). ACAM2000, or LC16M8, is live, competent vaccinia virus and can replicated in immunocompromised patients, thereby cause adverse side effects that stimulates developing new vaccines like JYNNEOS.
Antivirals (e.g. tecovirimat, brincidofovir, cidofovir) and vaccinia immune globulin intravenous are indicated to use in severe disease, immunocompromised patients, pediatrics, pregnant and breastfeeding women, complicated lesions, and lesions around the mouth, eyes, and genitals[23]. Tecovirimat, in 2018 became the first ever approved by FDA to treat smallpox after it proved safe in human trials and effective in animals administered closely related viruses. FDA approved Smallpox antivirals tecovirimat to treat MPX[9]. One patient had taken 600 mg tecovirimat orally twice per day for 2 wk and was hospitalized for 10 d with no adverse effects except a shorter time of viral shedding[25]. In 2021, FDA approved a second drug for smallpox, brincidofovir, although it showed promising results against the virus in animal studies[25], three patients had 200 mg brincidofovir per week orally, all of them had elevated liver enzymes leading to stop this treatment[25]. Brincidofovir shows a better clinical effect than tecovirimat based on the limited data.
The World Health Organization called the current MPX outbreak a Public Health Emergency of International Concern on July 23, 2022. Cases of MPX continue to rise rapidly with improved surveillance, access to diagnosis, and continuing spreading of infection globally. JYNNEOS is the only FDA-approved non-replicating smallpox and monkeypox vaccine with less side effects. MPX has a much less serious threat of a massive global pandemic than COVID-19. As MPX outbreaks is primarily contained in adult men, it should be manageable, and will be controlled by education, MPX surveillance, diligent monitoring, vaccination, and crossborder collaborations with international sectors.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hraib M, Syria; Kwon SL, Korea S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Walter K, Malani PN. What Is Monkeypox? JAMA. 2022;328:222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 23] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 2. | Uwishema O, Adekunbi O, Peñamante CA, Bekele BK, Khoury C, Mhanna M, Nicholas A, Adanur I, Dost B, Onyeaka H. The burden of monkeypox virus amidst the Covid-19 pandemic in Africa: A double battle for Africa. Ann Med Surg (Lond). 2022;80:104197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Mahase E. Monkeypox: What do we know about the outbreaks in Europe and North America? BMJ. 2022;377:o1274. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 46] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 4. | Leung B. More than 35,000 cases of monkeypox reported worldwide. China Daily. 18 Aug 2022. [cited 26 Aug 2022]. Available from: https://global.chinadaily.com.cn/a/202208/18/WS62fd7b84a310fd2b29e72d0f.html. [Cited in This Article: ] |
| 5. | Rao AK, Schulte J, Chen TH, Hughes CM, Davidson W, Neff JM, Markarian M, Delea KC, Wada S, Liddell A, Alexander S, Sunshine B, Huang P, Honza HT, Rey A, Monroe B, Doty J, Christensen B, Delaney L, Massey J, Waltenburg M, Schrodt CA, Kuhar D, Satheshkumar PS, Kondas A, Li Y, Wilkins K, Sage KM, Yu Y, Yu P, Feldpausch A, McQuiston J, Damon IK, McCollum AM; July 2021 Monkeypox Response Team. Monkeypox in a Traveler Returning from Nigeria - Dallas, Texas, July 2021. MMWR Morb Mortal Wkly Rep. 2022;71:509-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 154] [Article Influence: 77.0] [Reference Citation Analysis (0)] |
| 6. | Kupferschmidt K. Why monkeypox is mostly hitting men who have sex with men. Science. 2022;376:1364-1365. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 42] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 7. | Tambo E, Al-Nazawi AM. Combating the global spread of poverty-related Monkeypox outbreaks and beyond. Infect Dis Poverty. 2022;11:80. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 26] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 8. | Mohapatra RK, Tuli HS, Sarangi AK, Chakraborty S, Chandran D, Chakraborty C, Dhama K. Unexpected sudden rise of human monkeypox cases in multiple non-endemic countries amid COVID-19 pandemic and salient counteracting strategies: Another potential global threat? Int J Surg. 2022;103:106705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 37] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 9. | Hraib M, Jouni S, Albitar MM, Alaidi S, Alshehabi Z. The outbreak of monkeypox 2022: An overview. Ann Med Surg (Lond). 2022;79:104069. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 61] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 10. | Girometti N, Byrne R, Bracchi M, Heskin J, McOwan A, Tittle V, Gedela K, Scott C, Patel S, Gohil J, Nugent D, Suchak T, Dickinson M, Feeney M, Mora-Peris B, Stegmann K, Plaha K, Davies G, Moore LSP, Mughal N, Asboe D, Boffito M, Jones R, Whitlock G. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis. 2022;22:1321-1328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 275] [Cited by in F6Publishing: 258] [Article Influence: 129.0] [Reference Citation Analysis (0)] |
| 11. | Julvez J, Vannier P. [Risk and risk management connected with xenograft]. Pathol Biol (Paris). 2000;48:399-403. [PubMed] [Cited in This Article: ] |
| 12. | Awan MAE, Waseem M, Sahito AF, Sahito AM, Khatri G, Butt MA, Ramproshad S, Mondal B, Hasan MM. Monkeypox has devastated the world; should we prepare for the outbreak of a new pandemic? Ann Med Surg (Lond). 2022;79:104051. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | European Centre for Disease Prevention and Control. Joint ECDC-WHO regional office for Europe monkeypox surveillance bulletin. [cited 26 August 2022]. Available from: https://monkeypoxreport.ecdc.europa.eu/. [Cited in This Article: ] |
| 14. | European Centre for Disease Prevention and Control. Epidemiological update: Monkeypox multi-country outbreak. Summary of epidemiological update as of 15 June. [cited 26 August 2022]. Available from: https://www.ecdc.europa.eu/en/news-events/epidemiological-update-monkeypox-multi-country-outbreak-15-june. [Cited in This Article: ] |
| 15. | Peiró-Mestres A, Fuertes I, Camprubí-Ferrer D, Marcos MÁ, Vilella A, Navarro M, Rodriguez-Elena L, Riera J, Català A, Martínez MJ, Blanco JL; Hospital Clinic de Barcelona Monkeypox Study Group. Frequent detection of monkeypox virus DNA in saliva, semen, and other clinical samples from 12 patients, Barcelona, Spain, May to June 2022. Euro Surveill. 2022;27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 187] [Cited by in F6Publishing: 171] [Article Influence: 85.5] [Reference Citation Analysis (0)] |
| 16. | Antinori A, Mazzotta V, Vita S, Carletti F, Tacconi D, Lapini LE, D'Abramo A, Cicalini S, Lapa D, Pittalis S, Puro V, RivanoCapparuccia M, Giombini E, Gruber CEM, Garbuglia AR, Marani A, Vairo F, Girardi E, Vaia F, Nicastri E; INMI Monkeypox Group. Epidemiological, clinical and virological characteristics of four cases of monkeypox support transmission through sexual contact, Italy, May 2022. Euro Surveill. 2022;27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 330] [Cited by in F6Publishing: 298] [Article Influence: 149.0] [Reference Citation Analysis (0)] |
| 17. | Noe S, Zange S, Seilmaier M, Antwerpen MH, Fenzl T, Schneider J, Spinner CD, Bugert JJ, Wendtner CM, Wölfel R. Clinical and virological features of first human monkeypox cases in Germany. Infection. 2022;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 74] [Article Influence: 74.0] [Reference Citation Analysis (0)] |
| 18. | Kozlov M. Monkeypox in Africa: the science the world ignored. Nature. 2022;607:17-18. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 19. | Statista. Monkeypox - Statistics & Facts. [cited 17 August 2022]. Available from: https://www.statista.com/topics/9473/monkeypox/#topicHeader__wrapper. [Cited in This Article: ] |
| 20. | Bosworth A, Wakerley D, Houlihan CF, Atabani SF. Monkeypox: An old foe, with new challenges. Infect PrevPract. 2022;4:100229. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Aden TA, Blevins P, York SW, Rager S, Balachandran D, Hutson CL, Lowe D, Mangal CN, Wolford T, Matheny A, Davidson W, Wilkins K, Cook R, Roulo RM, White MK, Berman L, Murray J, Laurance J, Francis D, Green NM, Berumen RA 3rd, Gonzalez A, Evans S, Hudziec M, Noel D, Adjei M, Hovan G, Lee P, Tate L, Gose RB, Voermans R, Crew J, Adam PR, Haydel D, Lukula S, Matluk N, Shah S, Featherston J, Ware D, Pettit D, McCutchen E, Acheampong E, Buttery E, Gorzalski A, Perry M, Fowler R, Lee RB, Nickla R, Huard R, Moore A, Jones K, Johnson R, Swaney E, Jaramillo J, Reinoso Webb C, Guin B, Yost J, Atkinson A, Griffin-Thomas L, Chenette J, Gant J, Sterkel A, Ghuman HK, Lute J, Smole SC, Arora V, Demontigny CK, Bielby M, Geeter E, Newman KAM, Glazier M, Lutkemeier W, Nelson M, Martinez R, Chaitram J, Honein MA, Villanueva JM. Rapid Diagnostic Testing for Response to the Monkeypox Outbreak - Laboratory Response Network, United States, May 17-June 30, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:904-907. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Kupferschmidt K. WHO holds off on global alarm for monkeypox. Science. 2022;377:17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y. Prevention and Treatment of Monkeypox. Drugs. 2022;82:957-963. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 228] [Article Influence: 114.0] [Reference Citation Analysis (0)] |
| 24. | Petersen E, Zumla A, Hui DS, Blumberg L, Valdoleiros SR, Amao L, Ntoumi F, Asogun D, Simonsen L, Haider N, Traore T, Kapata N, Dar O, Nachega J, Abbara A, Al Balushi A, Kock R, Maeurer M, Lee SS, Lucey DR, Ippolito G, Koopmans M. Vaccination for monkeypox prevention in persons with high-risk sexual behaviours to control on-going outbreak of monkeypox virus clade 3. Int J Infect Dis. 2022;122:569-571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 43] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 25. | Adler H, Gould S, Hine P, Snell LB, Wong W, Houlihan CF, Osborne JC, Rampling T, Beadsworth MB, Duncan CJ, Dunning J, Fletcher TE, Hunter ER, Jacobs M, Khoo SH, Newsholme W, Porter D, Porter RJ, Ratcliffe L, Schmid ML, Semple MG, Tunbridge AJ, Wingfield T, Price NM; NHS England High Consequence Infectious Diseases (Airborne) Network. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. 2022;22:1153-1162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 686] [Cited by in F6Publishing: 599] [Article Influence: 299.5] [Reference Citation Analysis (0)] |
| 26. | Dhawan M, Priyanka, Choudhary OP. Emergence of monkeypox: Risk assessment and containment measures. Travel Med Infect Dis. 2022;49:102392. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |