Copyright
©The Author(s) 2022.
World J Clin Cases. Sep 26, 2022; 10(27): 9619-9627
Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9619
Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9619
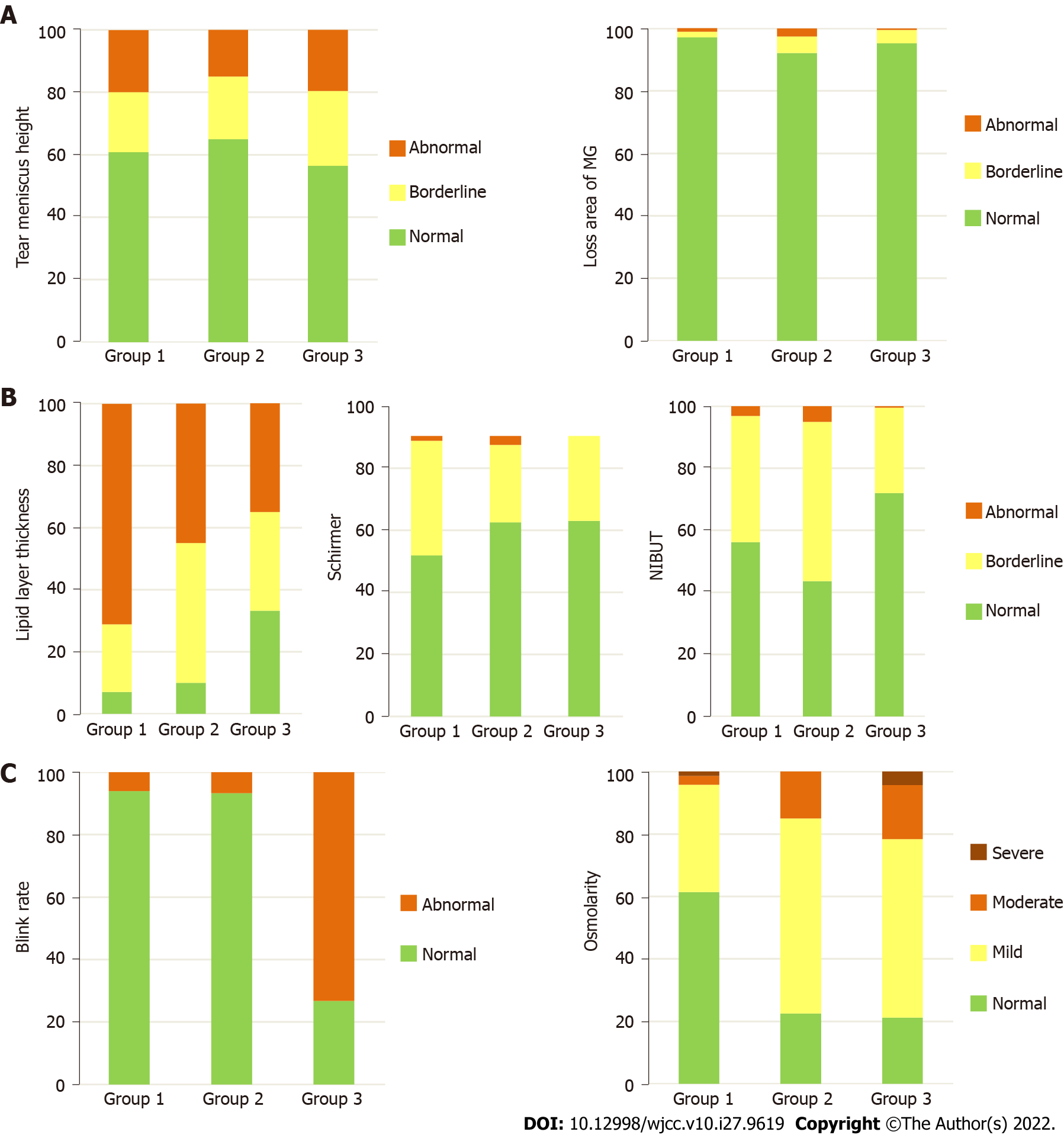
Figure 2 Tear meniscus height, lipid layer thickness, Schirmer test, loss area of meibomian gland, blink rate, non-invasive break-up time, and osmolarity grade frequencies before lockdown (from August 2019 to March 2020 - group 1), after lockdown without mask mandate (from April 2020 to October 2020 - group 2), and after lockdown with mask mandate (from December 2020 to April 2021 - group 3).
Tear meniscus height grade: Abnormal (< 0.22), borderline (> 0.44), and normal (0.22-0.44). Lipid grade: Abnormal (< 60), borderline (60-80), and normal (> 80). Schirmer test grade: Abnormal (< 5), borderline (5-10), and normal (> 10). Loss area of meibomian gland grade: Abnormal (> 60), borderline (40-60), and normal (< 40). Blink grade: Normal (90-100) and abnormal (< 90). Non-invasive break-up time grade: Abnormal (< 5), borderline (5-10), and normal (> 10). Osmolarity grade: Abnormal (> 320), borderline (300-320), and normal (< 300). A: Variables that did not change the frequency of the grade included: Tear meniscus height (P = 0.598) and loss area of meibomian gland (P = 0.529); B: Variables that improved the frequency of the grade along with groups included: Lipid layer thickness (P < 0.001) and Schirmer test (P = 0.013); C: Variables that worsened the frequency of the grade included: Blink rate (P < 0.001), non-invasive break-up time (P < 0.001), and osmolarity (P < 0.001). MG: Meibomian gland; NIBUT: Non-invasive break-up time.
- Citation: Marta A, Marques JH, Almeida D, José D, Sousa P, Barbosa I. Impact of COVID-19 pandemic on the ocular surface. World J Clin Cases 2022; 10(27): 9619-9627
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9619.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9619