Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6543
Peer-review started: September 14, 2021
First decision: September 29, 2021
Revised: November 2, 2021
Accepted: May 5, 2022
Article in press: May 5, 2022
Published online: July 6, 2022
Esophageal granular cell tumor (eGCT) is a relatively rare, usually benign neoplasm of the neuroectoderm. It is derived from Schwann cells. Clinical symptoms of this disease are non-specific. However, the most common presenting symptom is dysphagia, which is mostly misdiagnosed as esophageal polyps under gastroscopy, yet it has a 2% chance of forming cancers. We report the case of a 52-year-old woman with solitary eGCT, then analysed retrospectivelyanalyze the clinical features and elucidate on the reduction of misdiagnosis and missed diagnosis.
A 52-year-old woman was diagnosed with “esophageal granulossoma” after esophagoscopy, which was mistaken for eGCT.
eGCT diagnosis depends on characteristic pathomorphologies and detection of the S-100 protein. Endoscopic mucosal resection is the preferred therapeutic method.
Core Tip: Esophageal granular cell tumor is a relatively rare, usually benign neoplasm of the neuroectoderm. It is derived from Schwann cells. Clinical symptoms of this disease are non-specific. However, the most common presenting symptom is dysphagia, which is mostly misdiagnosed as esophageal polyps under gastroscopy, yet it has a 2% chance of forming cancers. In this report, clinical features are analyzed to facilitate the reduction of misdiagnosis and missed diagnosis.
- Citation: Chen YL, Zhou J, Yu HL. Esophageal granular cell tumor: A case report. World J Clin Cases 2022; 10(19): 6543-6547
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6543.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6543
Granular cell tumor (GCT) is a rare disease that was first detected in the tongue by Abrikossoff in 1926[1]. Usually, GCT develops on the skin or oral mucosa, especially in the tongue[2]. In 1931, Abrikossoff first described GCT in the esophagus, which is currently the most common site of involvement within the gastrointestinal tract, primarily the distal segment of the esophagus[3]. Most esophageal granular cell tumor (eGCT) are benign, with fewer than 2% of clinical cases being malignant[4].
In this report, we describe an eGCT that had developed in the middle of the esophagus, and we conducted a systematic review of 72 cases reported in China. The clinical data were analyzed to conclude the characteristics of eGCT so as to raise clinical awareness.
A 2-year history of acid reflux heartburn and a choking sensation during eating for the past month.
A 52-year-old female patient with a 2-year history of acid reflux heartburn and a choking sensation during eating for the past month was admitted to our hospital. Symptoms could be alleviated by oral administration of acid suppressants. We performed gastroscopy to establish the cause of the disease (June 2020). Upon admission, vital signs were within normal limits. Cardiopulmonary and abdominal examination did not show any abnormalities. Physical examination did not reveal a significant weight loss. There was no clinically significant family history, the patient had no smoking or drinking habits, and neither did she have a history of using special drugs or exposures to toxic substances.
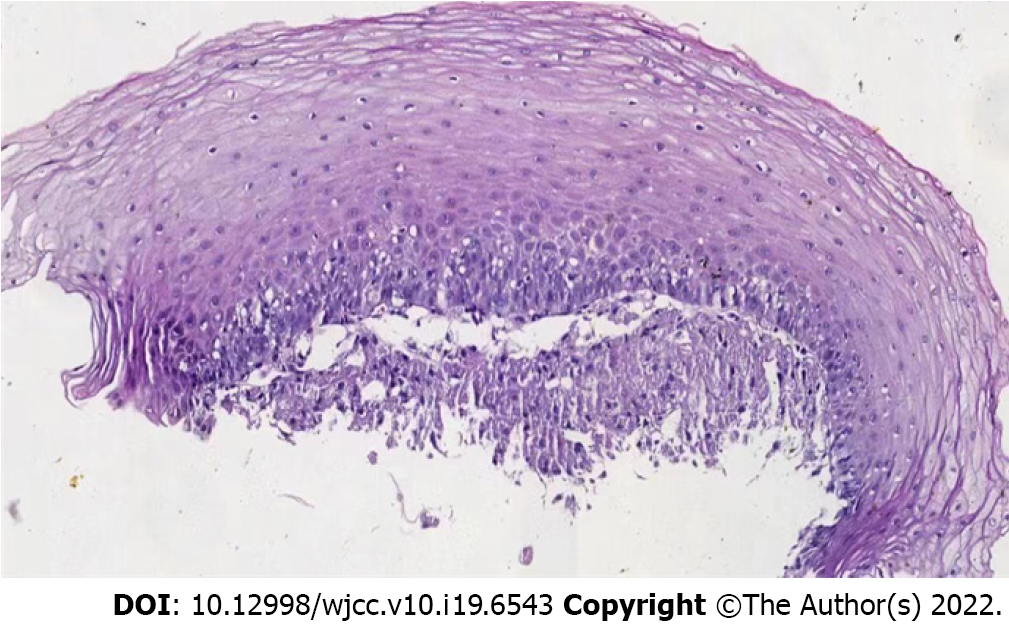
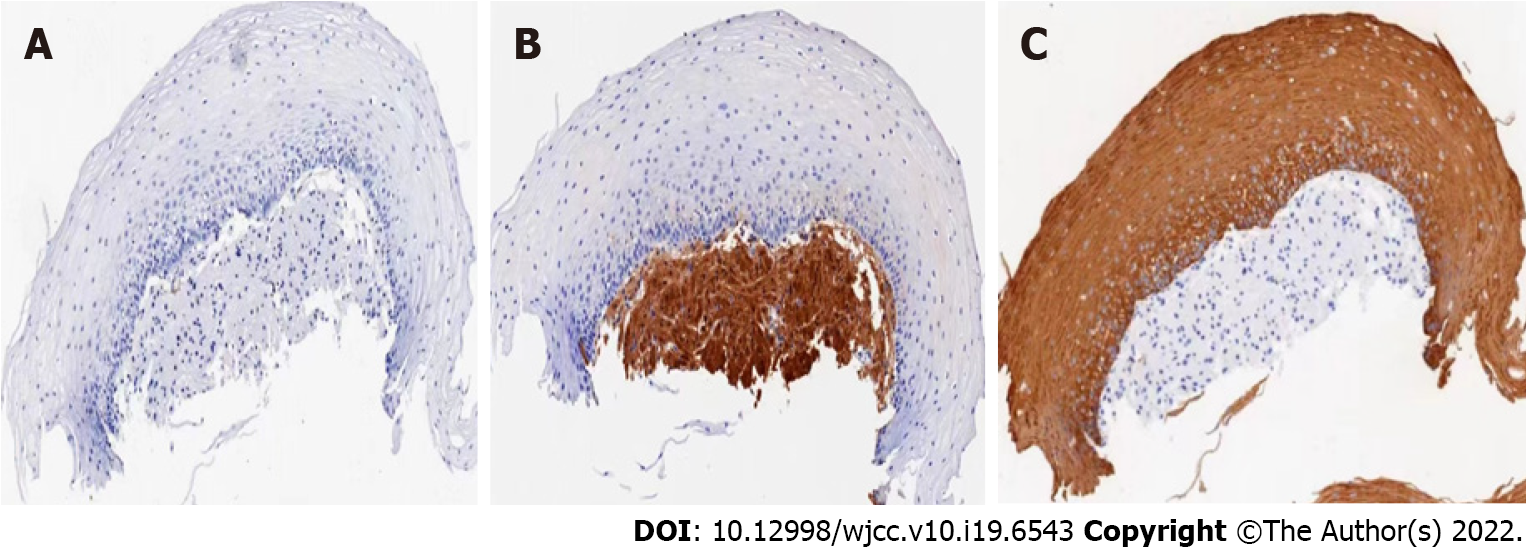
Under white light gastroscopy, there was a humulous-shaped eminence about 26 cm away from the incisor. Mucosa was smooth and clearly demarcated, with a size of about 0.4 cm and a hard yellow texture (Figure 1). Biopsy of the mass was performed. Pathological HE staining showed that tumor cells were closely arranged in a nest or strip shape, cell sizes were the same, the cytoplasm was rich, there was a large number of eosinophilic granulosa cells, while the nucleus was small, round and centered (Figure 2). The diagnosis of GCT was established by immunohistochemical staining, which was positive for the glycoprotein S100 protein, CK (+), SMA (-) (Figure 3).
The patient had an unremarkable medical history.
There was no clinically significant family history, the patient had no smoking or drinking habits, and neither did she have a history of using special drugs or exposures to toxic substances.
Cardiopulmonary and abdominal examination did not show any abnormalities.
No abnormality was found in blood routine examination and liver and kidney function. CEA, CA125 and CA199 were normal.
Under white light gastroscopy, there was a humulous-shaped eminence about 26 cm away from the incisor. Mucosa was smooth and clearly demarcated, with a size of about 0.4 cm and a hard yellow texture.
Esophageal granular cell tumor.
Because the volume of the mass was less than 1 cm, re-examination was performed by gastroscopy.
Her patient was diagnosed with granulosa cell tumor, but endoscopic surgery was not performed due to the small size of the tumor, and the tumor size did not increase during the 1-year follow-up.
The esophageal granular cell tumor is extremely uncommon. It was first described by Abrikossoff in 1931, when he reported on a patient with such tumors found in the esophagus. However, eGCT is an unusual developmental site for GCTs. Johnston and Helwig[3] reported on 75 GCTs of the gastrointestinal tract, most of them being located in the esophagus, which accounts for about 1 to 2 % of GCTs. Majority of these GCTs are often located in the esophageal distal part, followed by the colon, perianal region, stomach, small intestines and appendix[5].
Recently, we conducted a literature search in PubMed, Web of Science, and China National Knowledge Infrastructure (CNKI) were searched for all studies published till July 2021. Using relevant keywords “esophageal granular cell tumor” in Chinese, and found 71 cases. The patient described in this report is the 72nd case, which confirms that Esophageal GCTs are rare. Of the 72 patients, 44 were male while 28 were female, their ages ranged from 28 years to 66 years, with a mean of 46 years. Regarding clinical manifestations, 30 patients exhibited upper abdominal pain and fullness while 10 patients had swallowing discomforts, acid reflux and heartburn. Regarding esophageal location, they were in the upper (n = 9), middle (n = 18), and distal (n = 45) parts. Most of the tumors appeared yellow. Maximum diameters of tumors ranged from 0.4 cm to 5.5 cm, however, most of them were within 1 cm. A total of 35 patients had been subjected to endoscopic ultrasonography: 22 cases originated from the submucosa, 6 cases from the mucosal layer, 5 cases from the mucosal muscularis, and 2 cases from muscularis propria. One case of malignant granulosa cell tumor was pathologically confirmed (1.38%).
Usually, eGCT, which is diagnosed by gastroscopy, clinically manifests as a slow-growing round tumor with somewhat undefined margins measuring between 5-20 mm in diameter[6]. It appears yellow or white, with a hard, fixed texture. Endoscopy can be performed to provide additional information on the layer of origin and tumor extension[7]. Most eGCTs originate from the submucosa, it doesn't invade serosal layers of the esophagus. Histologic evaluation is the gold standard method for diagnosis.
Clinically, eGCT is a rare soft lesion with potential malignant tissue neoplasms. Its tissue origin is unclear. Various cell lines, derived from Schwann cells of the neuroectoderm have been proposed to be possible causes of GCT[8]. GCT exhibits typical pathomorphology and immunohistochemical characteristics. The main characteristics consist of nests of round or polygonal large cells with round, central nuclei and with eosinophilic cytoplasms as well as markedly enlarged lysosomes with a granular appearance[3]. Immunohistochemistry expressing S-100, CD68 and Vimentin, did not express CD117, CD34, SMA, Desmin, CK. Observation of these tumors is indicated unless the patient is symptomatic or the tumor is greater than 1 cm or has atypical endoscopic ultrasonographic or histologic features[7]. The most preferred treatment option for eGCT is endoscopic resection, which is highly associated with bleeding and perforation[9,10]. Although most granulocytomas are benign and grow slowly, about 2% of granulocytomas are malignant, which require surgery. For clinical evaluation, tumor diameter ≥ 3 cm is considered malignant, however, malignancy is also suspected if the tumor grows rapidly and forms ulcers[11]. The rapid growth of malignant tumors can lead to metastasis, especially to regional lymph nodes, lungs, liver, and bone[12].
In conclusion, the gastro- intestinal tract is an unusual developmental site for a GCTs, with the esophagus being the most common site of origin. Its diagnosis depends on characteristic pathomorphologies and detection of the S-100 protein. Endoscopic mucosal resection is the preferred therapeutic method.
We sincerely thank the patient and their family for their support and dedication.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Grawish ME, Egypt; Kai K, Japan S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Abrikossoff A. Uber Myome' ausgehend von der uergestreiften will-kurlichen Muskulatur. Virchows Arch Pathol Anat. 1926;260(1):215-233. [DOI] [Cited in This Article: ] [Cited by in Crossref: 714] [Cited by in F6Publishing: 455] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Calonje E, Tsai KE. Soft-tissue tumours and tumour-like conditions. 9th ed. London: Wiley; 2016. [Cited in This Article: ] |
| 3. | Galanopoulos M, Liatsos C, Nakos G, Kalafatis E. Abrikossoff cell tumor of the esophagus: case presentation of a rare endoscopic entity and review of literature. J Gastrointest Cancer. 2015;46:87-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Barakat M, Kar AA, Pourshahid S, Ainechi S, Lee HJ, Othman M and Tadros M. Gastrointestinal and biliary granular cell tumor: Diagnosis and management. Ann Gastroenterol. 2018;31:439-447. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Johnston MJ, Helwig EB. Granular cell tumors of the gastro intestinal tract and perianal region A study of 74 cases. Dig Dis Sci 1981; 26: 807 816. [Cited in This Article: ] |
| 6. | Taban SM, Barna RA, Dema ALC, Ratiu IM, Popa O, Plopeanu AD. Unexpected diagnosis for a gastric polyp: Granular cell tumor: Case report and review of the literature. Exp Ther Med. 2021;21:536. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Goldblum JR, Rice TW, Zuccaro G, Richter JE. Granular cell tumors of the esophagus: a clinical and pathologic study of 13 cases. Ann Thorac Surg. 1996;62: 860-865. [Cited in This Article: ] |
| 8. | Lewin KJ, Applebaum HD. Tumors of the esophagus and stomach. In: Atlas of tumor pathology, Series 3, vol. 18. Washington, DC: Armed Forces Institute of Pathology (AFIP); 1996. 154-155. [Cited in This Article: ] |
| 9. | Komori K, Akahoshi K, Tanaka Y, Motomura Y, Kubokawa M, Itaba S, Hisano T, Osoegawa T, Nakama N, Iwao R, Oya M, Nakamura K. Endoscopic submucosal dissection for esophageal granular cell tumor using the clutch cutter. World J Gastrointest Endosc. 2012;4:17-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Lu W, Xu MD, Zhou PH, Zhang YQ, Chen WF, Zhong YS, Yao LQ. Endoscopic submucosal dissection of esophageal granular cell tumor. World J Surg Oncol. 2014;12:221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Aoyama K, Kamio T, Hirano A, Seshimo A, Kameoka S. Granular cell tumors: a report of six cases. World J Surg Oncol. 2012;10:204. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Machado I, Cruz J, Lavernia J, Llombart-Bosch A. Solitary, multiple, benign, atypical, or malignant: the Granular Cell Tumor puzzle. Virchows Arch. 2016;468:527-538. [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |