Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4574
Peer-review started: October 5, 2021
First decision: February 7, 2022
Revised: February 11, 2022
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: May 16, 2022
Globe luxation is rare and is mostly due to direct orbital trauma with fractures of the medial and floor walls, which displace the globe into the maxillary sinus. Only a few cases have been reported; moreover, patients who suffer global luxation rarely achieve eyesight recovery.
This report describes the treatment and prognosis of global luxation occurring in a child. A 6-year-old boy presented with left globe luxation that occurred after a sudden stop on a tricycle, without any injury to the orbital or maxillofacial bony structures. After admission to the hospital, an external canthus incision, globe repositioning, orbital exploration and temporary blepharoplasty were performed. Finally, the child completely recovered and maintained good eyesight in his left eye even though the right eye developed myopia after four years of follow-up.
The aim of this study was to report the special occurrence of globe luxation in the child and share some experience of the treatment. Immediate surgical management plays an important role in the recovery of visual function, and globe luxation may prevent nearsightedness by reducing the distortion of the eyeball, shortening the axis and improving ciliary function.
Core Tip: Globe luxation is rare and is mostly due to direct orbital trauma with fractures of the medial and floor walls, displacing the globe into the maxillary sinus. In our case, globe luxation was not as severe as those previously reported, and luxation occurred when the boy’s tricycle stopped suddenly. The boy maintained an intact retinal nerve and extraocular muscle and completely recovered after eye repositioning. After the surgery and 4-year follow-up, we consider that immediate surgical management must be performed, especially for patients whose retinal nerve is not severely injured. In addition, we hypothesize that there might exist some correlation between globe luxation and myopia; globe luxation might prevent nearsightedness by reducing the distortion of the eyeball and improving the function of ciliary.
- Citation: Li Q, Xu YX. Globe luxation may prevent myopia in a child: A case report. World J Clin Cases 2022; 10(14): 4574-4579
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4574.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4574
Luxation of the globe is a rare event that results from severe trauma to the orbit that often causes orbital rim and wall fractures, and it is sometimes accompanied by optic nerve avulsion and extraocular muscle (EOM) rupture. Most of these patients present impaired vision and restricted movement of the injured eyeball, even after the globe is repositioned. Herein, we report of a case of a 6-year-old boy who solely suffered left globe luxation, without any injury to the orbital bones or the maxillofacial structures. He achieved complete visual functional recovery and good cosmesis. However, after 4 years of follow-up, we were surprised to learn that the vision of his injured eye was better than that of the other eye, and his left eye maintained good eyesight, whereas the right eye was nearsighted.
A 6-year-old child was admitted to the Eye Department of the Second Affiliated Hospital of Anhui Medical University (on June 3, 2017) with a complaint of ocular proptosis and no light perception after his tricycle had come to a sudden stop.
He was admitted to our department 4 h after the left eyeball was dislocated without any other facial injury after his tricycle had come to a sudden stop. He had pain in his left eye and experienced no light perception; moreover, his extraocular motility was limited.
The child and his grandfather denied any other medical conditions.
The child and his grandfather denied any family history of related diseases.
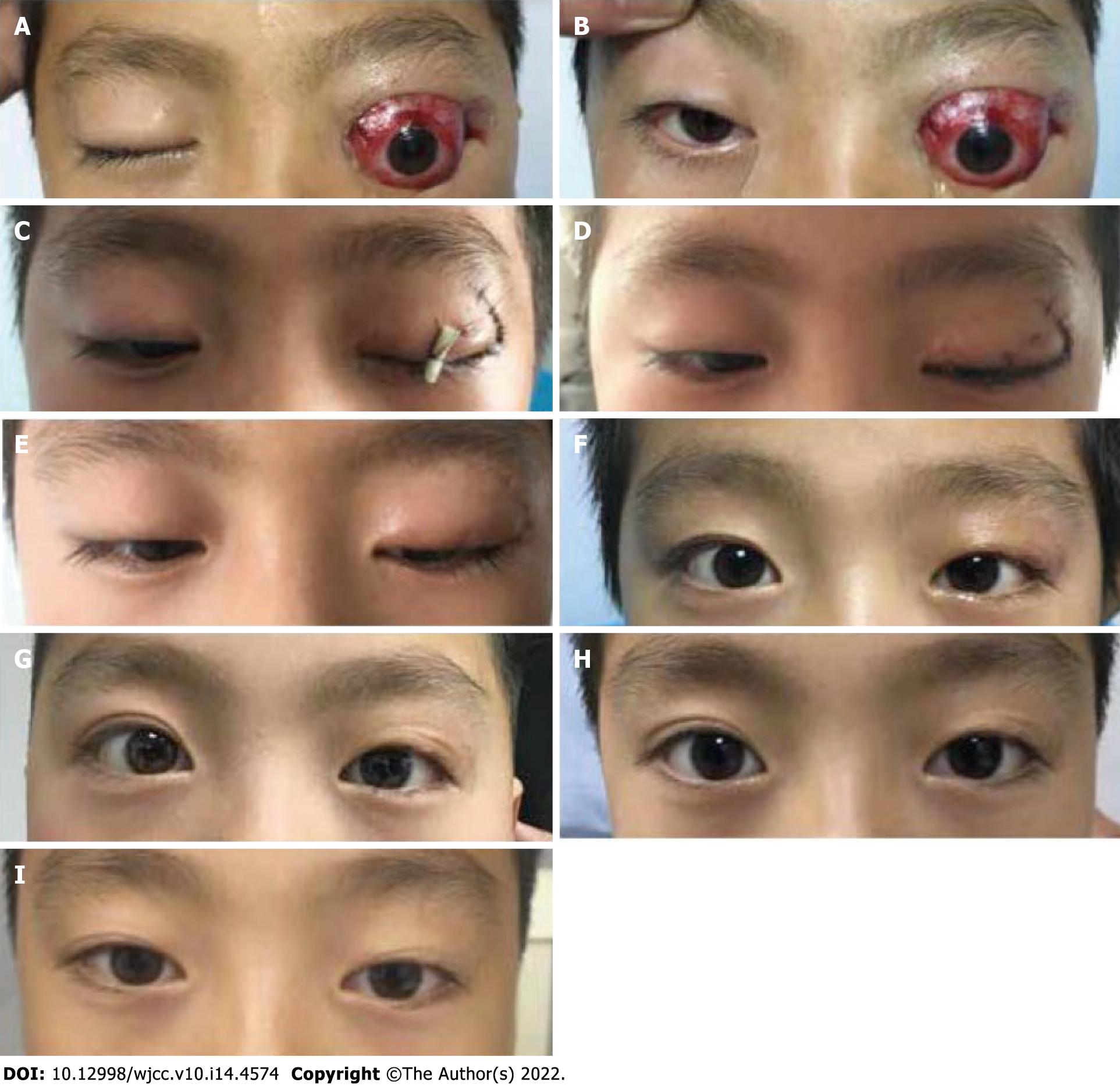
Upon clinical examination, the patient presented with intact left globe luxation, exophthalmos (L/R = 5 mm), no visual acuity, no perception of light and a complete limitation of extraocular motility in all directions. The eyelid was intact, the conjunctiva showed hyperaemia, the cornea was dry and completely exposed and the pupil was mid-dilated, with no reaction to light (Figure 1A and B). Furthermore, he could not keep his right eye open.
No laboratory tests.
Computed tomography and magnetic resonance imaging showed proptosis of the left globe and gas accumulation in the superior intraconal space and stretching of the EOM (Figure 2A-E). Magnetic resonance angiography excluded carotid cavernous fistula (Figure 2F).
Combined with the clinical and imaging examination, the final diagnosis was globe luxation.
One day after admission, the patient was transferred to an operating room to treat the ocular lesions, and an external canthus incision, globe repositioning, orbital exploration and temporary blepharoplasty were performed. The eyeball was pressure bandaged for the next 48 h. Seven days later, the eyelid suture was removed.
His ocular signs were essentially normal when he left the hospital 8 d after the surgery (Figure 1D). His left globe was repositioned with slight ocular hyperaemia and vision recovery (R/L = 1.0/0.2). After 1 mo of postoperative follow-up, the vision of the left eye had improved to 1.0, without restricted ocular movement and no signs of infection (Figure 1E). The patient has undergone 48 mo of follow-up, with satisfactory cosmetic and functional results. However, the visual acuity of his right eye was 0.2 due to nearsightedness (optometry: spherical equivalent of 1.25 D), and the axes of his eyes were oculus dexter: 23.66 mm and oculus sinister: 23.24 mm (measured on June 4, 2021) (Figure 1).
Globe luxation rarely occurs and is often caused by direct orbital trauma with fractures of the medial and floor walls displacing the globe into the paranasal sinuses[1]. In our case, the boy experienced globe luxation when his tricycle stopped suddenly and did not have any other facial injuries. He did not remember whether he hit his head on any hard surfaces, such as the handlebar; thus, we believed that his globe luxation may have been caused by a sudden deceleration force while the eye maintained a high speed, which caused the orbit to stop suddenly after hitting a hard object of the tricycle. We found it interesting that globe luxation is often caused by severe trauma, which leads to severe orbital fractures and intraconal retrobulbar haematoma; however, the injured eye of this boy completely recovered, and the vision of the injured eye remained at 1.0, whereas the other eye was nearsighted. In this case, the pathogenesis, outcome and prognosis of globe luxation requires further study and discussion.
Globe luxation is often accompanied by different degrees of optic nerve avulsion, which is associated with prognosis[2]. In this case, the boy kept his optic nerve intact and completely recovered his visual acuity, which was consistent with the cases reported by Ramstead et al[3] and Müller-Richter et al[4]. It can be concluded that patients with globe luxation (but without optic nerve avulsion) have an increased possibility of achieving complete visual recovery. Moreover, immediate surgical management must be emphasized; once the possibility of other diseases is ruled out, every attempt should be made to anatomically reposition a displaced globe as soon as possible[5]. Treatment delays will increase the risk of complications, such as oedema and strain on the optic nerve and central retinal artery over time, especially in those patients with optic nerve avulsion[6].
When globe luxation occurs, the EOM can be injured as well, depending on the degree of trauma. The medial rectus is most commonly affected, followed by the inferior rectus, which often severely restricts eyeball movement[7]. Luckily, in our case, the EOM of the boy was only stretched. After globe repositioning, there was no proof of EOM injury; the movements of the globe were not restricted to any degree in any direction, and his eye function consistently remained good. After four years of follow-up, the visual acuity in the injured eye remained at 1.0, whereas the right eye had unexpected myopia. We are unsure how this result occurred. Myopic development is associated with stress imposed on the globe by the lids and EOM. Extraocular muscle forces may temporarily distort the eyeball; over time, such distortion may become permanent and lead to myopia[8,9]. Moreover, Li et al[10] demonstrated that the development of staphyloma in patients with a high degree of myopia is related to EOM displacement. Therefore, we may reasonably infer that after the EOM was stretched, its flexibility was decreased, which may reduce the stress imposed on the eyeball by the EOM, thereby reducing the distortion to some degree. Furthermore, the ciliary muscle plays an important role in regulating the lens; after luxation, the blood circulation in the ciliary may be changed, which may have a relaxing effect in the ciliary, thus reducing the incidence of myopia[11]. Of course, we cannot exclude that the boy may have taken more care of the left eye after it was injured; however, we believe that the use of both eyes was equal. It may be possible that both eyes were myopic, but that one of them exhibited more severe myopia. However, it is difficult to understand why the injured eye consistently remained good, even though the other eye was myopic (spherical equivalent of 1.25D).
In our case, globe luxation was not as severe as what has been previously reported, and luxation occurred when the boy’s tricycle stopped suddenly. The boy maintained an intact retinal nerve and EOM and completely recovered after eye repositioning. According to this case, we believe that immediate surgical management must be performed, especially for patients with retinal nerves that are not severely injured. In addition, we hypothesize that there may exist some correlation between globe luxation and myopia; globe luxation may prevent nearsightedness by reducing the distortion of the eyeball and improving ciliary function.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Laddha UD, India; Vagholkar K, India S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Amaral MB, Carvalho MF, Ferreira AB, Mesquita RA. Traumatic globe luxation associated with orbital fracture in a child: a case report and literature review. J Maxillofac Oral Surg. 2015;14:323-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | de Saint Sardos A, Hamel P. Traumatic globe luxation in a 6-year-old girl playing with a tube of wrapping paper. J AAPOS. 2007;11:406-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ramstead C, McCabe J, Alkahtani M, Leong-Sit J, Morhart M. Traumatic dislocation of the globe into the maxillary sinus. Can J Ophthalmol. 2008;43:364-366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Müller-Richter UD, Kohlhof JK, Driemel O, Wagener H, Reichert TE. Traumatic dislocation of the globe into the maxillary sinus. Int J Oral Maxillofac Surg. 2007;36:1207-1210. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Haggerty CJ, Roman P. Repositioning of a traumatically displaced globe with maxillary antrostomy: review of the literature and treatment recommendations. J Oral Maxillofac Surg. 2013;71:1915-1922. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Noman SA, Shindy MI. Immediate Surgical Management of Traumatic Dislocation of the Eye Globe into the Maxillary Sinus: Report of a Rare Case and Literature Review. Craniomaxillofac Trauma Reconstr. 2017;10:151-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Gaur N, Kumari S, Takkar B, Sharma P. Globe luxation, complex eyelid laceration and lost medial rectus: extreme complication of ocular trauma. BMJ Case Rep. 2019;12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Mathur A, Atchison DA, Kasthurirangan S, Dietz NA, Luong S, Chin SP, Lin WL, Hoo SW. The influence of oblique viewing on axial and peripheral refraction for emmetropes and myopes. Ophthalmic Physiol Opt. 2009;29:155-161. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Hartwig A, Gowen E, Charman WN, Radhakrishnan H. Working distance and eye and head movements during near work in myopes and non-myopes. Clin Exp Optom. 2011;94:536-544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Li Y, Wei Q, Le A, Gawargious BA, Demer JL. Rectus Extraocular Muscle Paths and Staphylomata in High Myopia. Am J Ophthalmol. 2019;201:37-45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Nomi Y, Iwasaki-Kurashige K, Matsumoto H. Therapeutic Effects of Anthocyanins for Vision and Eye Health. Molecules. 2019;24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |