Published online May 16, 2022. doi: 10.12998/wjcc.v10.i14.4425
Peer-review started: August 19, 2021
First decision: November 11, 2021
Revised: March 25, 2022
Article in press: March 25, 2022
Published online: May 16, 2022
With the rapid development of haploidentical hematopoietic stem cell trans
To evaluate the role of PND capsule in acute leukemia patients with haplo-HSCT.
We retrospectively collected data of acute leukemia patients who underwent haplo-HSCT at the Affiliated People’s Hospital of Ningbo University between April 1, 2015 and June 30, 2020. Twenty-nine consecutive patients received oral PND capsule from the sixth day to the first month after haplo-HSCT were included in the PND group. In addition, 31 patients who did not receive PND capsule during haplo-HSCT were included in the non-PND group. Subsequently, we compared the therapeutic efficacy according to the western medical evaluation indexes and Chinese medical symptom scores, and the survival between the PND group and the non-PND group, using the chi-square test, Fisher’s exact test, and the Kaplan–Meier method.
The duration of platelet engraftment was shorter in the PND group than in the non-PND group (P = 0.039). The PND group received a lower frequency of red blood cells and platelet transfusions than the non-PND group (P = 0.033 and P = 0.035, respectively). In addition, PND capsule marginally reduced the rate of PGF (P = 0.027) and relapse (P = 0.043). After 33 (range, 4-106) months of follow-up, the 3-year relapse-free survival (P = 0.046) and progression-free survival (P = 0.049) were improved in the PND group than in the non-PND group. Also, the therapeutic efficacy of the PND group according to Chinese medical symptom scores was significantly better than that of the non-PND group (P = 0.022). Moreover, the adverse events caused by PND capsule were mild. Nevertheless, there were no significant differences in the duration of neutrophil engraftment, the risk of infection within 100 days after haplo-HSCT, the acute graft-versus-host disease, or the 3-year overall survival between the two groups.
PND capsule could promote hematopoiesis reconstitution, improve the therapeutic efficacy of Chinese medical symptom scores, present anti-tumor effectiveness, and prolong the survival of acute leukemia patients with haplo-HSCT.
Core Tip: New Chinese patent medicine Pai-Neng-Da (PND) Capsule exerts dual effect of promoting hematopoiesis recovery and regulating immunity. However, the efficacy of PND capsule in patients with haploidentical hematopoietic stem cell transplantation (haplo-HSCT) has not yet been reported. To the best of our knowledge, this is the first study that evaluated the effectiveness of PND capsule in acute leukemia (AL) patients following haplo-HSCT. Our study showed that PND capsule could promote hematopoietic function recovery, improve the therapeutic efficacy according to Chinese medical symptom scores, present anti-tumor effectiveness, and prolong the survival of AL patients who underwent haplo-HSCT.
- Citation: Yuan JJ, Lu Y, Cao JJ, Pei RZ, Gao RL. Hematopoiesis reconstitution and anti-tumor effectiveness of Pai-Neng-Da capsule in acute leukemia patients with haploidentical hematopoietic stem cell transplantation. World J Clin Cases 2022; 10(14): 4425-4435
- URL: https://www.wjgnet.com/2307-8960/full/v10/i14/4425.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i14.4425
Allogeneic hematopoietic stem cell transplantation is an effective therapy for hematologic malignancies. Over recent years, haploidentical hematopoietic stem cell transplantation (haplo-HSCT) has shown similar outcomes to identical-sibling transplants. Moreover, haplo-HSCT is an efficient post-remission treatment for patients lacking an identical donor[1-3]. Nonetheless, in haplo-HSCT, the human leukocyte antigen (HLA) disparity between the donor and the recipient can lead to an intense bidirectional alloreactivity predisposition for developing primary graft failure. Graft failure includes graft rejection and primary poor graft function (PGF). The reported incidence of primary PGF is 5–27%[4,5]. PGF results in prolonged hospitalization, expensive medical costs, and high transplant-related mortality owing to infectious complications or hemorrhage. According to recent studies, improving the bone marrow (BM) microenvironment represents a promising therapeutic approach to promote hema
Panaxadiol saponin component (PDS-C) is a biologically active component isolated from total saponins of ginsenosides and currently available in the form of capsules named as Pai-Neng-Da (PND) Capsule[7]. Preclinical studies have suggested that PDS-C can be used to treat multiple hemocytopenia in mice, including idiopathic thrombocytopenic purpura (ITP), aplastic anemia (AA), myelosuppression, and hemocytopenia caused by chemotherapy or radiation[8,9]. PDS-C possesses hematopoietic growth factor-like function that promotes proliferation and differentiation of hematopoietic progenitor cells in myelosuppressed mice, probably mediated by regulating phosphorylated mitogen-activated protein kinase, extracellular signal-regulated kinases protein kinases, receptor tyrosine kinase and globin transcription factor (GATA) 1 transcription factors[8]. PDS-C could modulate T lymphocyte immune functions by increasing CD4+ cells, downregulating T-bet protein expression, and upregulating GATA-3 protein expressions[8,9]. Moreover, panaxadiol showed anti-tumor activity in human leukemia cell lines by arresting the cell cycle at the G1/S phase[10,11].
So far, two certificates of new class-five Chinese patent medicine have been authorized and granted by China Food and Drug Administration, including PDS-C and its PND capsule. PND capsule for treating hemocytopenia has successfully passed Phase I clinical trial and has shown to be effective without significant side effects in Phase II trial[7]. On the other hand, the efficacy of PND capsule in hematopoietic recovery after haplo-HSCT has not yet been reported.
In this study, we evaluated the role of PND capsule in acute leukemia (AL) patients with haplo-HSCT. To the best of our knowledge, this is the first study that evaluates the efficacy of PND capsule in the treatment of AL patients following haplo-HSCT.
A total of 60 patients diagnosed with AL who underwent haplo-HSCT at the Department of Hematology, Affiliated People’s Hospital of Ningbo University, were included in this retrospective study. Twenty-nine consecutive patients received oral PND capsule from the sixth day to the first month after haplo-HSCT between April 1, 2018 and June 30, 2020 were included in the PND group. In addition, 31 patients who did not receive PND capsule during haplo-HSCT between April 1, 2015 and March 31, 2018 were included in the non-PND group. All patients were included in the analysis, and none were excluded on account of severe toxicity.
Hematopoietic stem cells were derived from both BM and peripheral blood. Potential haploidentical donors included both first- and non-first-degree relatives. The haploidentical donor was selected based on the status of donor-specific anti-HLA antibodies (DSA). In the presence of DSA, patients received plasmapheresis or rituximab therapy. The other factors that were considered were sex, age, cytomegalovirus (CMV) serostatus, and weight ratio between donors and recipients.
PND capsule was provided by the First Affiliated Hospital of Zhejiang Chinese Medical University and Ningbo Tianzhen Pharmaceutical Co. Ltd., China (Batch No. 20150401, each capsule contains PDS-C 40 mg with a purity of 92.44%, analyzed and defined by high-performance liquid chromatography using specific monomers of ginsenosides as the reference standards)[12].
Pediatric patients (< 14 years old) were given PND capsule 4 mg/kg/day (integer capsules were taken according to clinical operability). Adult patients were given two capsules at a time, three-times/day.
Primary PGF was defined as persistent neutropenia (≤ 0.5×109/L), thrombocytopenia (platelets ≤ 20 × 109/L), and/or hemoglobin concentration ≤ 70 g/L after engraftment with hypocellular BM and full donor chimerism without concurrent acute graft-versus-host disease (aGVHD) or disease relapse. Neutrophil engraftment was defined as the first step in the three consecutive days when the absolute neutrophil count was 0.5 × 109/L without granulocyte colony-stimulating factor (G-CSF) stimulation. Platelet engraftment was defined as the first 7 consecutive days when the platelet count was ≥ 20 × 109/L, independent of platelet transfusion. The hematological recovery was defined as neutrophils > 0.5 × 109/L, platelets > 20 × 109/L, and hemoglobin concentration > 70 g/L without transfusion support or G-CSF stimulation[13-16]. The red blood cells (RBC) transfusions were performed in patients with symptomatic anemia or hemoglobin concentration < 70 g/L or hematocrit level < 0.2. Platelet transfusions were performed considering a threshold level of ≥ 20×109 platelets/L in patients with bleeding or fever.
The therapeutic efficacy was assessed according to the rate of decrease in Chinese medical (CM) symptom score: (1) Cured: the CM symptoms disappeared, and the score decreased more than 95%; (2) Favorably effective: CM symptoms were improved, and the score decreased more than 75%; (3) Effective: CM symptoms were improved, and the score decreased more than 30%; and (4) Ineffective: No significant improvement or an even worse condition was observed, and the score reduced to less than 30%. CM symptoms included pale lips and nails, palpitation and dizziness, weakness and fatigue, soreness and weakness of waist and knees, dry mouth and thirst, hot flashes, night sweats, cold limbs, dry or thin feces, epistaxis, and bleeding. CM symptoms were evaluated and recorded from 0 to 3 according to severity[12].
According to the criteria established by the Center for Adverse Drug Reaction Monitoring of the Ministry of Health and the five-level classification, adverse drug reactions were assessed using the following levels: Certain, probable, possible, suspicious, and impossible; the first four levels were judged as possibly related to the investigational drug.
The conditioning therapy was as follows: Cytarabine (4 g/m2/d) intravenously on days –10 to –9, busulfan (3.2 mg/kg/d) intravenously on days -8 to -6, cyclophosphamide (1.8 g/m2/d) intravenously on days -5 to -4, semustine (250 mg/m2/d), orally once on day –3, and thymoglobulin (2.5 mg/kg/d, Sang Stat, Lyon, France) intravenously on days –5 to –2. Graft-versus-host disease (GVHD) prophylaxis regimen consisted of cyclosporine A, mycophenolate mofetil, and short-term methotrexate. Patients received prophylaxis against bacterial, viral, and fungal agents. The reactivation of CMV infection and Epstein–Barr virus (EBV) infection was monitored by polymerase chain reaction twice/week during the early period (days +15 to +100) and then once/week (from days +100 to +180).
All clinical data were analyzed in this study using SPSS 26.0 software. The patient characteristics between the two groups were compared using the Mann–Whitney test for continuous variables and the chi-square test or Fisher’s exact test for categorical data. Measurement data is shown with mean ± SD. The survival analysis was carried out using the Kaplan–Meier method. All statistical tests were 2-sided. P value < 0.05 was considered statistically significant.
The baseline characteristics are summarized in Table 1. No differences in the baseline data, including sex, age, diagnosis, high cytogenetic risk, disease status at transplantation, peripheral blood cell counts (pre-transplantation), the number of courses of chemotherapy before transplantation, donor’s age, female donor–male recipient pairs, CMV IgG-positive recipients, and the infused mononuclear cells (MNCs) and CD34+ cells of the grafts were observed between the PND and the non-PND groups (all P > 0.05).
| Characteristics | Non-PND group (n = 31) | PND group (n = 29) | P value |
| Age (yr) | 0.441 | ||
| Median | 33 | 37 | |
| Range | 3–63 | 2–62 | |
| Males, n (%) | 17 (54.8) | 18 (62.1) | 0.609 |
| Diagnosis, n (%) | 0.793 | ||
| Acute myeloid leukemia | 19 (61.3) | 19 (65.5) | |
| Acute lymphocytic leukemia | 12 (38.7) | 10 (34.5) | |
| High cytogenetic risk, n (%) | 11 (35.5) | 12 (41.4) | 0.791 |
| Courses of chemotherapy before transplantation | 0.819 | ||
| Median | 3 | 3 | |
| Range | 2–7 | 2–8 | |
| Disease status at transplantation, n (%) | 0.758 | ||
| First complete remission | 25 (80.6) | 22 (75.9) | |
| Second complete remission | 6 (19.4) | 7 (24.1) | |
| Peripheral blood cell counts (pre-transplantation) | |||
| Neutrophil count (109/L) | 0.824 | ||
| Median | 1.5 | 1.25 | |
| Range | 0.45-6.21 | 0.42-6.77 | |
| Hemoglobin concentration (g/L) | 0.773 | ||
| Median | 92 | 86 | |
| Range | 68-130 | 72-142 | |
| Platelet count (109/L) | 0.636 | ||
| Median | 87 | 83 | |
| Range | 34-310 | 45-275 | |
| Donor’s age (yr) | 0.668 | ||
| Median | 34 | 39 | |
| Range | 9–62 | 10–63 | |
| Female donor–male recipient pairs, n (%) | 7 (22.6) | 8 (27.5) | 0.769 |
| Cytomegalovirus IgG-positive recipients, n (%) | 16 (51.6) | 13 (44.8) | 0.617 |
| Infused mononuclear cells (× 108/kg) | 0.270 | ||
| Median | 12.42 | 14.67 | |
| Range | 8.39–44.41 | 7.93–39.44 | |
| Infused CD34 + cells (× 106/kg) | 0.243 | ||
| Median | 4.32 | 3.72 | |
| Range | 1.20–7.47 | 1.03–10.80 |
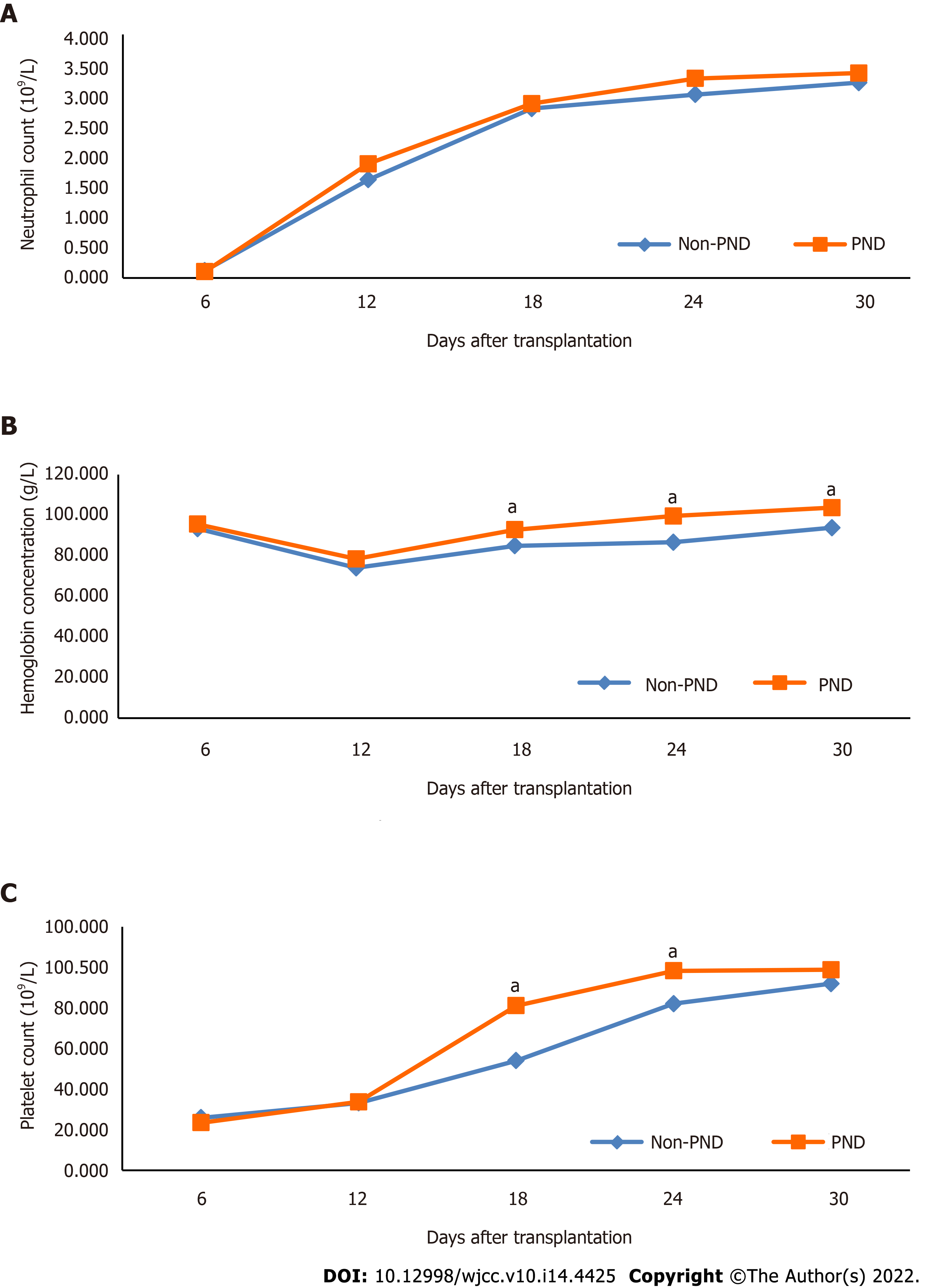
Compared with the non-PND group, the PND group achieved higher hemoglobin concentration on the eighteenth day (P = 0.029), the twenty-fourth day (P = 0.003), and the first month (P = 0.043) after haplo-HSCT, as well as the platelet count on the eighteenth day (P = 0.002) and the twenty-fourth day (P = 0.046) after haplo-HSCT (Table 2 and Figure 1).
| Group | Case | Days after transplantation | Neutrophil count (109/L) | Hemoglobin concentration (g/L) | Platelet count (109/L) |
| Non-PND | 31 | 6 | 0.12 ± 0.05 | 93.35 ± 15.23 | 21.55 ± 13.27 |
| 12 | 1.61 ± 1.15 | 73.97 ± 7.67 | 27.65 ± 11.96 | ||
| 18 | 2.78 ± 2.29 | 84.90 ± 12.17 | 45.03 ± 31.40 | ||
| 24 | 3.01 ± 1.15 | 86.65 ± 11.70 | 68.39 ± 49.61 | ||
| 30 | 3.21 ± 1.60 | 93.81 ± 16.94 | 76.65 ± 52.66 | ||
| PND | 29 | 6 | 0.10 ± 0.04 | 95.55 ± 14.13 | 19.55 ± 8.47 |
| 12 | 1.87 ± 1.18 | 78.41 ± 10.01 | 28.07 ± 12.49 | ||
| 18 | 2.86 ± 1.37 | 92.83 ± 14.58a | 67.55 ± 35.63a | ||
| 24 | 3.28 ± 1.47 | 99.55 ± 17.83a | 81.90 ± 38.37a | ||
| 30 | 3.36 ± 1.15 | 103.66 ± 19.22 a | 82.31 ± 37.70 |
The duration of platelet engraftment was shorter in the PND group than in the non-PND group [median 12 (range, 8–152) days vs median 13 (range, 9–145) days, respectively, P = 0.039]. Also, patients in the PND group received a lower frequency of RBC and platelet transfusions compared to the non-PND group (P = 0.033 and P = 0.035, respectively). Furthermore, compared to the non-PND group, patients in the PND group experienced a lower incidence of PGF (3.4% vs 25.8%, P = 0.027). In addition, the relapse rate after haplo-HSCT was reduced in patients using PND compared to those without PND (6.9% vs 29.0%, P = 0.043). However, the duration of neutrophil engraftment [median 12 (range, 10–14) days vs, median 12 (range, 10–15) days, respectively, P = 0.454], the rate of infectious complications within 100 days after haplo-HSCT (79.3% vs 87.1%, P = 0.500) and the occurrence of aGVHD (58.6% vs 45.2%, P = 0.316) were similar in the PND and non-PND groups (Table 3).
| Variates | Non-PND group(n = 31) | PND group(n = 29) | P value |
| Neutrophil engraftment time | 0.454 | ||
| Median | 12 | 12 | |
| Range | 10–15 | 10–14 | |
| Platelet engraftment time | 0.039 | ||
| Median | 13 | 12 | |
| Range | 9–145 | 8–152 | |
| RBC transfusion frequency | 0.033 | ||
| Median | 1 | 0 | |
| Range | 0–22 | 0–3 | |
| Platelet transfusion frequency | 0.035 | ||
| Median | 3 | 2 | |
| Range | 1–46 | 1–49 | |
| Poor graft function, n (%) | 8 (25.8) | 1 (3.4) | 0.027 |
| Infections within 100 d, n (%) | 27 (87.1) | 23 (79.3) | 0.500 |
| Cytomegaloviremia | 15 (48.4) | 11 (37.9) | |
| Pneumonia | 7 (22.6) | 7 (24.1) | |
| Sepsis | 2 (6.5) | 3 (10.3) | |
| Other infections | 3 (9.7) | 2 (6.9) | |
| aGVHD, n (%) | 14 (45.2) | 17 (58.6) | 0.316 |
| Ⅰ-Ⅱ | 11 (35.5) | 14 (48.3) | |
| Ⅲ-Ⅳ | 3 (9.7) | 3 (10.3) | |
| Relapse, n (%) | 9 (29.0) | 2 (6.9) | 0.043 |
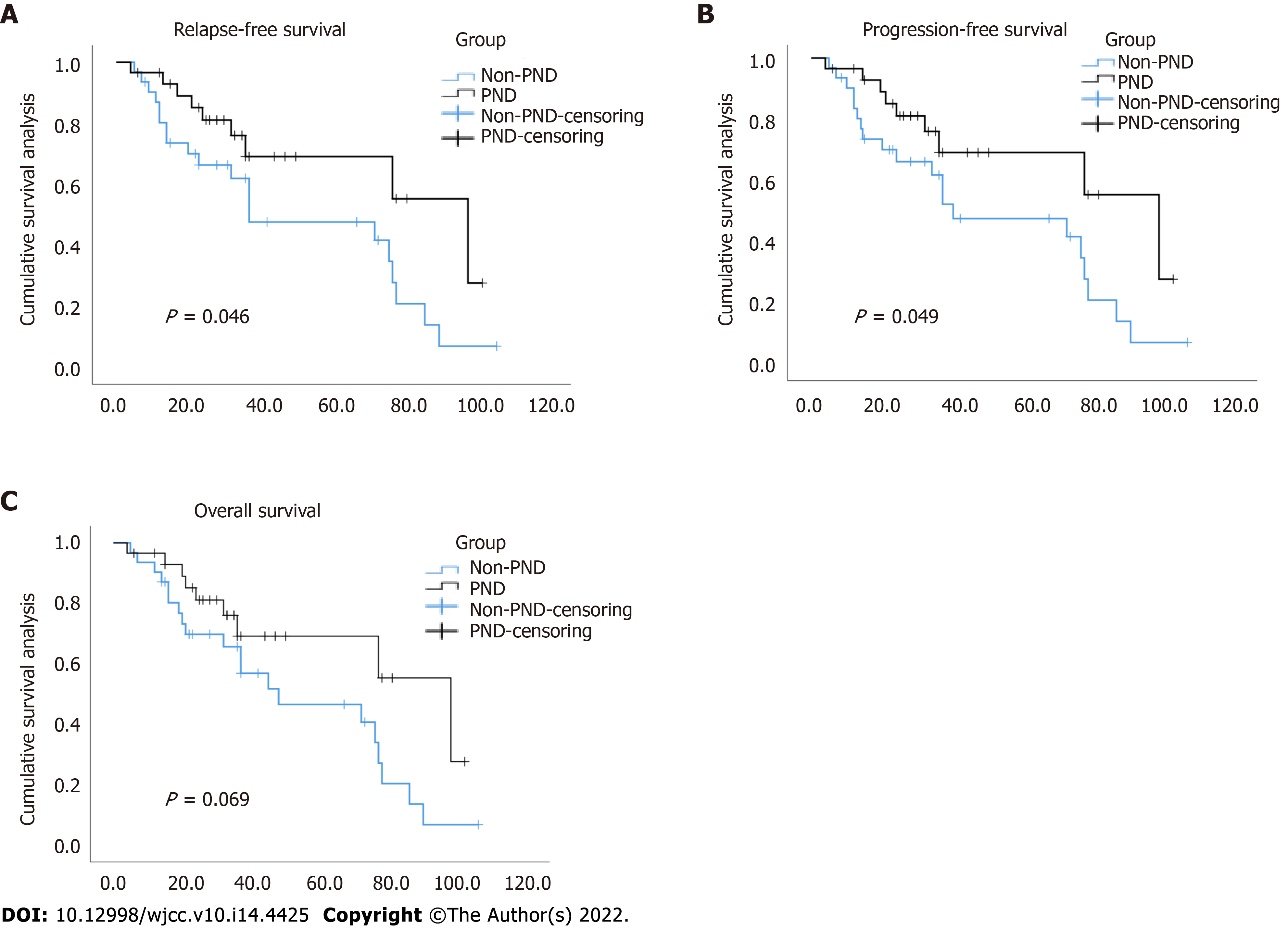
The survival analysis showed a statistically significant benefit for the 3-year relapse-free survival (RFS) (69.1% vs 61.9%, P = 0.046) and the 3-year progression-free survival (PFS) (69.1% vs 61.7%, P = 0.049) with the use of PND. Nonetheless, PND failed to improve the 3-year overall survival (OS) (69.1% vs 65.6%, P = 0.069) (Figure 2).
The therapeutic efficacy was assessed according to the rate of decrease in CM symptom score. In the PND group, 2 cases (6.90%) were cured, 9 cases (31.03%) were favorably effective, 16 cases (55.17%) were effective, 2 cases (6.90%) were ineffective; the effective rate was 93.10% (27/29). In the non-PND group, 0 cases were cured, 6 cases (19.35%) were favorably effective, 15 cases (48.39%) were effective, 10 cases (32.26%) were ineffective, and the effective rate was 67.74% (21/31). Thus, the therapeutic efficacy of the PND group according to CM symptom scores was significantly better than that of the non-PND group (P = 0.022) (Table 4).
During the administration of the PND capsule, the laboratory examinations of urine routine, electrocardiogram, hepatic and renal functions were normal. The hot flush, insomnia, dry mouth, sweating, and mild stomach discomfort at the early stage of medication were respectively observed in 1 case (3.4%), 2 cases (6.9%), 2 cases (6.9%), 1 case (3.4%) and 4 cases (13.8%) with PND capsule, and they spontaneously alleviated without any intervention.
With the rapid development of haplo-HSCT, primary PGF has become a life-threatening complication. The clinical risk factors of PGF include the number of infused CD34+ cells, donor-specific anti-HLA antibodies, GVHD, age, donor-recipient blood-type matching, and CMV infection[17-19]. Previous studies have found that patients with PGF have an inferior 2-year OS compared to those with good graft function[15]. However, reports related to the pathogenesis of primary PGF are limited. Effective therapies are inconclusive and need to be explored further.
PND capsule exerts dual effects of promoting hematopoiesis recovery and regulating immunity[7,9,20]. Phase I clinical trials have demonstrated that PND capsule is safe and does not induce side effects; the recommended safe dose range for clinical studies is 6–10 capsules (240-400 mg) daily[21]. State Food and Drug Administration of China has recommended PND capsule for treating ITP and unexplained leucopenia. Moreover, Zhu et al[22] found that PND capsule maintains peripheral hemograms, appropriately reducing the androgen dosage and improving the quality of life of patients with AA. However, the application of PND in haplo-HSCT has not yet been reported. Therefore, this study was conducted to evaluate the role of PND in promoting the recovery of hematopoietic function after haplo-HSCT and the correlation between PND and the prognosis of AL patients who underwent haplo-HSCT.
Our results showed that PND capsule markedly reduces the duration of platelet engraftment, the frequency of RBC and platelet transfusions, and the incidence of primary PGF. PND capsule can decrease the myelosuppression caused by chemotherapy, accelerate hematopoietic function recovery, especially for erythroid and megakaryocytic lineages, following haplo-HSCT. T cells have a crucial role in the immune destruction of BM. Patients with PGF showed significantly higher proportions of stimulated CD4+ and CD8+ T cells that produced IFN-gamma but notably decreased proportions of IL-4-producing T cells, resulting in a shift of the IFN-gamma/IL-4 ratio towards a type 1 response and an elevated percentage of activated CD8 + T cells[23]. PND-C could reduce peripheral blood CD8+ cells and increase CD4+ cells, reverting the ratio of CD4+/CD8+ cells to normal level in AA model mice[9]. Furthermore, hematopoiesis with PDS-C and its PND capsule is promoted via the intracellular signaling pathway, upregulating multiple transcription factors. The protein expression levels, phosphorylation status, and DNA binding activities were dramatically accentuated by PDS-C treatment in hematopoietic cells, promoting hematopoiesis and blood cells' formation[7,24]. However, PND capsule did not shorten the duration of neutrophil engraftment. Since the use of G-CSF on the sixth day after transplantation, the effect of PND capsule may be disturbed.
The correlation analysis related to risk factors of primary PGF could not be performed due to the small sample size. Notably, the primary PGF incidence (3.4%) caused by the use of PND capsule was lower than that reported in the current literature, ranging from 5% to 27%[4,5], which may be due to the following reasons: first, PND capsule has a role in improving hematopoietic recovery after transplantation, thereby reducing the rate of PGF. Second, the definition of primary PGF and the types of transplantation are different in the current and previous studies. Third, the number of our cases is limited. Thus, additional studies with more cases, unifying the definition of primary PGF and the types of transplantation, are required.
In our study, PND capsule significantly reduced the post-transplantation recurrence rates and increased the 3-year RFS and PFS, perhaps due to its anti-cancer effect. Basic research on anti-tumor effect of PND capsule is limited. As previously reported, panaxadiol selectively inhibits cyclin A-associated Cyclin-dependent kinase 2 activity by elevating the endogenous inhibitor proteins (CKIs) p21WAF1/CIP1 protein levels and arresting the cell cycle at the G1/S phase in human cancer cell lines[10,11]. The anti-tumor invasion and metastasis effects are related to the weakening of cell invasiveness[25]. Further in vivo and in vitro experiments are needed to explore the mechanism of anti-cancer effect of PND capsule. Yet, our data suggested that PND capsule does not affect the 3-year OS. The putative causes might be the insufficient follow-up time in the current study. Therefore, multicenter prospective studies with long follow-up times should be conducted to further investigate the potential influence of PND capsule on the survival of patients after haplo-HSCT.
According to CM symptom scores, the therapeutic efficacy of patients in the PND group was significantly better than the non-PND group. The adverse events of PND capsule were mild and spontaneously alleviated without intervention. Thus, these results indicated that PND capsule could improve the clinical effect and quality of life by alleviating the CM symptoms.
Our data suggest that PND capsule could promote hematopoiesis reconstitution, improve the therapeutic efficacy of CM symptom scores, present anti-tumor effectiveness, and prolong the survival of AL patients with haplo-HSCT. Yet, larger multicenter randomized controlled studies are needed to confirm these findings.
New Chinese patent medicine Pai-Neng-Da (PND) Capsule exerts dual effect in promoting hematopoiesis recovery and regulating immunity. However, the application of PND capsule in haplo-HSCT has not yet been reported. To the best of our knowledge, this is the first study that evaluates the efficacy of PND capsule in the treatment of acute leukemia (AL) patients following haplo-HSCT.
The main problem in this study is whether PND capsule could promote hematopoiesis reconstitution following haplo-HSCT and whether it is related to the prognosis of AL patients with haplo-HSCT.
Objective to evaluate the role of PND capsule in AL patients with haplo-HSCT.
We compared the therapeutic efficacy and the survival of AL patients with or without PND capsule during haplo-HSCT, using the chi-square test, Fisher’s exact test, and the Kaplan–Meier method.
PND capsule marginally reduced the rate of PGF and relapse. The 3-year relapse-free survival and progression-free survival were improved in the PND group than in the non-PND group. Also, the therapeutic efficacy of the PND group according to Chinese medical symptom scores was significantly better than that of the non-PND group.
PND capsule could promote hematopoiesis reconstitution, improve the therapeutic efficacy of Chinese medical symptom scores, present anti-tumor effectiveness, and prolong the survival of AL patients with haplo-HSCT.
The pathogenesis of primary PGF following haplo-HSCT is yet unclear. The effective therapies for primary PGF need to be explored.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Integrative and complementary medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Merli P, Italy; Yang T, China S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Lee CJ, Savani BN, Mohty M, Labopin M, Ruggeri A, Schmid C, Baron F, Esteve J, Gorin NC, Giebel S, Ciceri F, Nagler A. Haploidentical hematopoietic cell transplantation for adult acute myeloid leukemia: a position statement from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2017;102:1810-1822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 51] [Cited by in F6Publishing: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 2. | Salvatore D, Labopin M, Ruggeri A, Battipaglia G, Ghavamzadeh A, Ciceri F, Blaise D, Arcese W, Sociè G, Bourhis JH, Van Lint MT, Bruno B, Huynh A, Santarone S, Deconinck E, Mohty M, Nagler A. Outcomes of hematopoietic stem cell transplantation from unmanipulated haploidentical vs matched sibling donor in patients with acute myeloid leukemia in first complete remission with intermediate or high-risk cytogenetics: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica. 2018;103:1317-1328. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 3. | Brissot E, Labopin M, Ehninger G, Stelljes M, Brecht A, Ganser A, Tischer J, Kröger N, Afanasyev B, Finke J, Elmaagacli A, Einsele H, Mohty M, Nagler A. Haploidentical versus unrelated allogeneic stem cell transplantation for relapsed/refractory acute myeloid leukemia: a report on 1578 patients from the Acute Leukemia Working Party of the EBMT. Haematologica. 2019;104:524-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 4. | Larocca A, Piaggio G, Podestà M, Pitto A, Bruno B, Di Grazia C, Gualandi F, Occhini D, Raiola AM, Dominietto A, Bregante S, Lamparelli T, Tedone E, Oneto R, Frassoni F, Van Lint MT, Pogliani E, Bacigalupo A. Boost of CD34+-selected peripheral blood cells without further conditioning in patients with poor graft function following allogeneic stem cell transplantation. Haematologica. 2006;91:935-940. [PubMed] [Cited in This Article: ] |
| 5. | Lee KH, Lee JH, Choi SJ, Kim S, Seol M, Lee YS, Kim WK, Lee JS. Failure of trilineage blood cell reconstitution after initial neutrophil engraftment in patients undergoing allogeneic hematopoietic cell transplantation - frequency and outcomes. Bone Marrow Transplant. 2004;33:729-734. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Kong Y, Wang YT, Hu Y, Han W, Chang YJ, Zhang XH, Jiang ZF, Huang XJ. The bone marrow microenvironment is similarly impaired in allogeneic hematopoietic stem cell transplantation patients with early and late poor graft function. Bone Marrow Transplant. 2016;51:249-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Gao RL, Chong BH. Research and development of the effective components of panaxdiol saponin as new Chinese patent medicine for treating hemocytopenia. Chin J Integr Med. 2012;18:897-902. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Sun X, Zhao YN, Qian S, Gao RL, Yin LM, Wang LP, Chong BH, Zhang SZ. Ginseng-Derived Panaxadiol Saponins Promote Hematopoiesis Recovery in Cyclophosphamide-Induced Myelosuppressive Mice: Potential Novel Treatment of Chemotherapy-Induced Cytopenias. Chin J Integr Med. 2018;24:200-206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Zheng ZY, Yu XL, Dai TY, Yin LM, Zhao YN, Xu M, Zhuang HF, Chong BH, Gao RL. Panaxdiol Saponins Component Promotes Hematopoiesis and Modulates T Lymphocyte Dysregulation in Aplastic Anemia Model Mice. Chin J Integr Med. 2019;25:902-910. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Jin YH, Choi J, Shin S, Lee KY, Park JH, Lee SK. Panaxadiol selectively inhibits cyclin A-associated Cdk2 activity by elevating p21WAF1/CIP1 protein levels in mammalian cells. Carcinogenesis. 2003;24:1767-1772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Wang Z, Ding M, Lin Z, He C, Zhao Y. Esterified Derivatives of Panaxadiol and Their Inhibitory Effect on HL-60, THP-1, and PC-3 Cell Lines. Chem Biodivers. 2019;16:e1900188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Jiang ZY, Yu FQ, Gao RL, Kuang YM, Zhu Y, Chen YH, Li LJ, Ouyang GF, Hu J, Wu XL. Treatment of Chronic Aplastic Anemia with Chinese Patent Medicine Pai-Neng-Da capsule for Replacing Androgen Partially: A Clinical Multi-Center Study. Chin J Integr Med. 2021 Apr 10. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Sun YQ, He GL, Chang YJ, Xu LP, Zhang XH, Han W, Chen H, Chen YH, Wang Y, Wang FR, Wang JZ, Liu KY, Huang XJ. The incidence, risk factors, and outcomes of primary poor graft function after unmanipulated haploidentical stem cell transplantation. Ann Hematol. 2015;94:1699-1705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Shi MM, Kong Y, Song Y, Sun YQ, Wang Y, Zhang XH, Xu LP, Liu KY, Huang XJ. Atorvastatin enhances endothelial cell function in posttransplant poor graft function. Blood. 2016;128:2988-2999. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 15. | Zhao HY, Lyu ZS, Duan CW, Song Y, Han TT, Mo XD, Wang Y, Xu LP, Zhang XH, Huang XJ, Kong Y. An unbalanced monocyte macrophage polarization in the bone marrow microenvironment of patients with poor graft function after allogeneic haematopoietic stem cell transplantation. Br J Haematol. 2018;182:679-692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | Song Y, Zhao HY, Lyu ZS, Cao XN, Shi MM, Wen Q, Tang FF, Wang Y, Xu LP, Zhang XH, Huang XJ, Kong Y. Dysfunctional Bone Marrow Mesenchymal Stem Cells in Patients with Poor Graft Function after Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2018;24:1981-1989. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Stasia A, Ghiso A, Galaverna F, Raiola AM, Gualandi F, Luchetti S, Pozzi S, Varaldo R, Lamparelli T, Bregante S, Van Lint MT, di Grazia C, Bacigalupo A. CD34 selected cells for the treatment of poor graft function after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:1440-1443. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 18. | Chen J, Wang H, Zhou J, Feng S. Advances in the understanding of poor graft function following allogeneic hematopoietic stem-cell transplantation. Ther Adv Hematol. 2020;11:2040620720948743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Xiao Y, Song J, Jiang Z, Li Y, Gao Y, Xu W, Lu Z, Wang Y, Xiao H. Risk-factor analysis of poor graft function after allogeneic hematopoietic stem cell transplantation. Int J Med Sci. 2014;11:652-657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Wen WW, Sun X, Zhuang HF, Lin XJ, Zheng ZY, Gao RL, Yin LM. Effects of panaxadiol saponins component as a new Chinese patent medicine on proliferation, differentiation and corresponding gene expression profile of megakaryocytes. Chin J Integr Med. 2016;22:28-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Zou Ch, Xiong NN, Jiang M, Gao WM, Zou JD, Liu F. Phase I clinical study (human tolerance) on Painengda Capsules. Chin Trad Pat Med. 37: 2383-2386. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Zhu Y, Kuang YM, Gao RL, Jiang ZY, Huang L, Tong YJ, Lou XG, Gao XF. Clinical observation of Painengda capsule in improving the quality of life in patients with chronic aplastic anemia. Chin J Integr Med. 2016;26:124-126. [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Wang YT, Kong Y, Song Y, Han W, Zhang YY, Zhang XH, Chang YJ, Jiang ZF, Huang XJ. Increased Type 1 Immune Response in the Bone Marrow Immune Microenvironment of Patients with Poor Graft Function after Allogeneic Hematopoietic Stem Cell Transplantation. Biol Blood Marrow Transplant. 2016;22:1376-1382. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Sun X, Gao RL, Lin XJ, Xu WH, Chen XH. Panax notoginseng saponins induced up-regulation, phosphorylation and binding activity of MEK, ERK, AKT, PI-3K protein kinases and GATA transcription factors in hematopoietic cells. Chin J Integr Med. 2013;19:112-118. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Nakhjavani M, Smith E, Townsend AR, Price TJ, Hardingham JE. Anti-Angiogenic Properties of Ginsenoside Rg3. Molecules. 2020;25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |