Copyright
©The Author(s) 2017.
World J Clin Cases. Apr 16, 2017; 5(4): 153-158
Published online Apr 16, 2017. doi: 10.12998/wjcc.v5.i4.153
Published online Apr 16, 2017. doi: 10.12998/wjcc.v5.i4.153
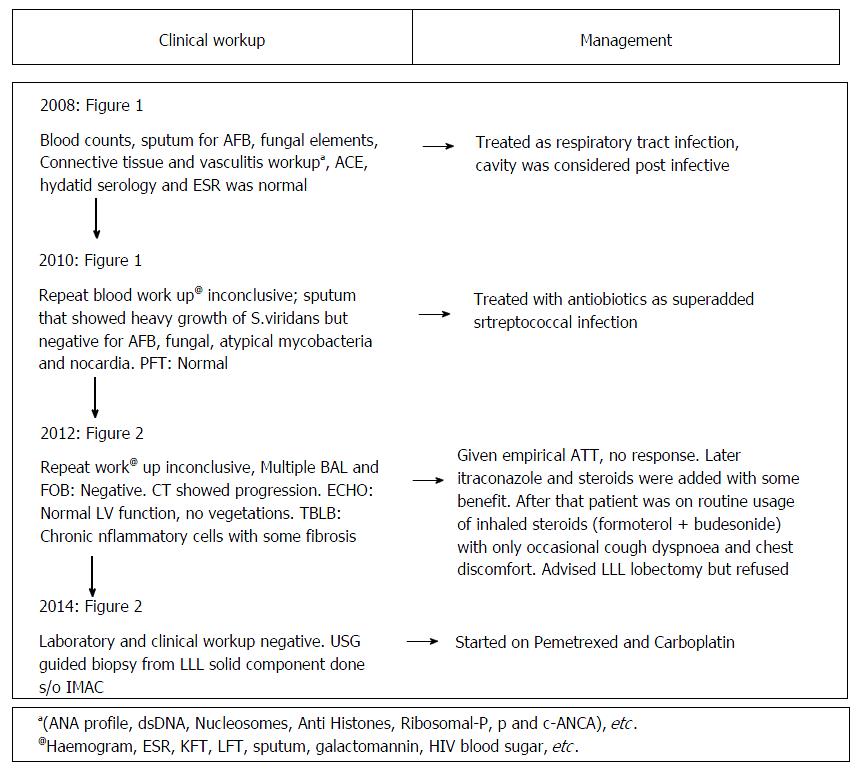
Figure 1 The clinical work-up and evaluation from onset till diagnosis.
BAL: Bronchoalveolar lavage; TBLB: Transbronchial lung biopsy; ACE: Angiotensin converting enzyme; EGFR: Epidermal derived growth factor receptor; PFT: Pulmonary function test; AFB: Acid fast bacilli; ESR: Erythrocyte sedimentation rate; GGO: Ground glass opacity; ATT: Anti tubercular therapy.
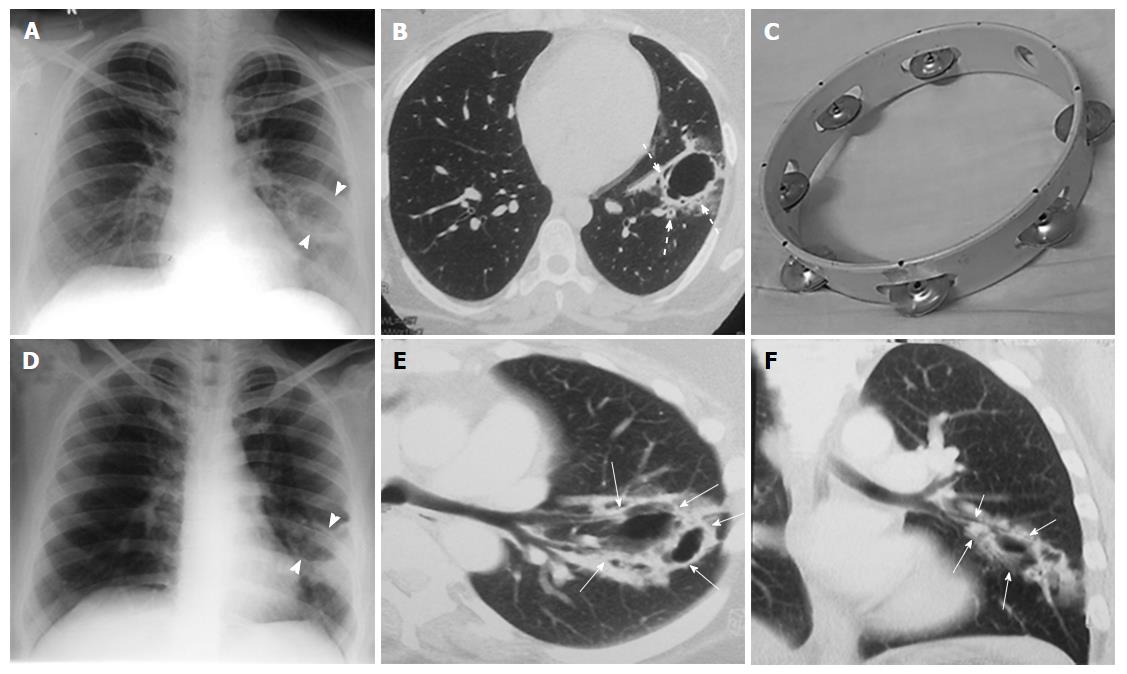
Figure 2 Initial and two year follow-up computed tomography imaging.
Chest radiograph (A) and CT (B) in 2008 (first study) show well-defined thin-walled (4 mm) irregular cavitary lesion (arrow head) in superior segment of left lower lobe. Thick walled bronchioles (dotted arrows) are seen near the edge and within the wall of cavity with adjacent ground glass giving rise to “Tambourine” sign; (C) depicts the musical instrument “tambourine” for comparison; subsequent radiograph (D) and CT (E and F) in 2010 shows increase in size and wall thickness of the cavity. Note the adjacent bronchioles (thin white arrows) entering into the cavity wall. CT: Computed tomography.
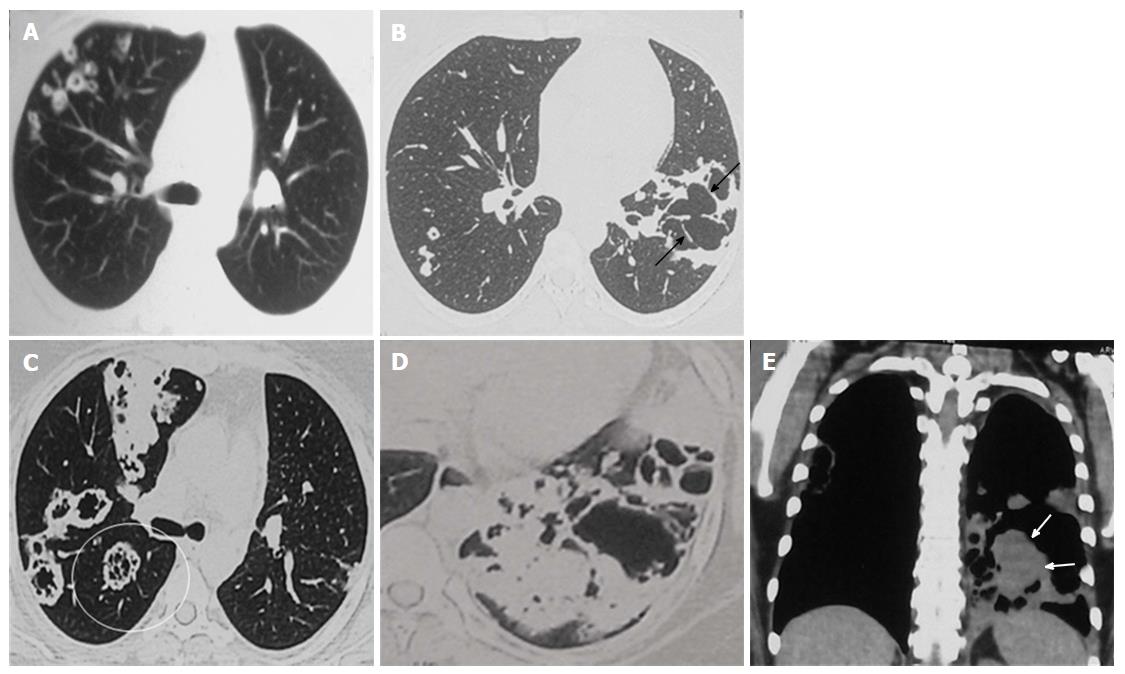
Figure 3 Disease progression with development of soft tissue.
Chest CT study of 2012 lung window (A and B) shows multiple new cavitating nodules in RUL (A) and increase in size of LLL cavity with development of internal septations (arrows) (B). No solid nodules or GGO or consolidation is seen. Current CECT images (2014: C to E) demonstrate further increase in size of the lesions and multiple new lesions having internal septations and development of significant soft tissue component in LLL cavity (solid arrows). Also note the “Tambourine” sign in RLL cavities as well (encircled cavity in C). LLL: Left lower lobe; RUL: Right upper lobe; GGO: Ground glass opacity; CECT: Contrast-enhanced computed tomography.
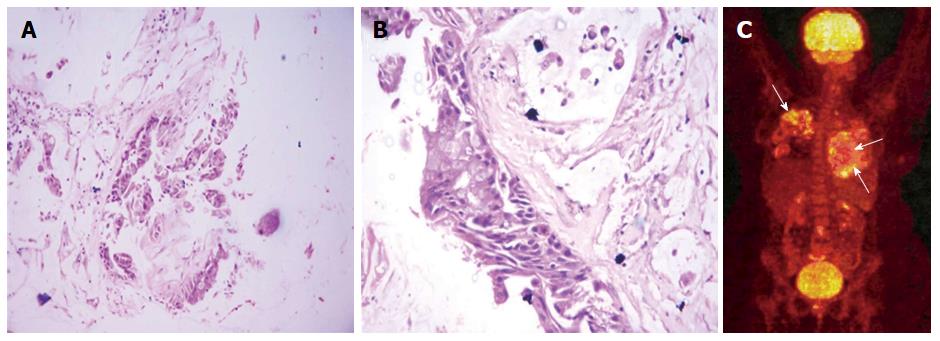
Figure 4 Histopathology and positron emission tomography findings.
A and B: Histological photomicrograph shows fragments of tumor with mucinous epithelium H and E × 40. Higher magnification (C) shows invasive mucinous adenocarcinoma with pools of extracellular mucin H and E × 400; C: Whole-body PET-CT image shows patchy mild uptake of FDG within the lung lesions. No evidence of extrathoracic primary site of malignancy is there. PET-CT: Positron emission tomography-computed tomography; FDG: 2-[fluorine-18] fluoro-2-deoxy-D-glucose.
- Citation: Verma R, Bhalla AS, Goyal A, Jain D, Loganathan N, Guleria R. Ominous lung cavity “Tambourine sign”. World J Clin Cases 2017; 5(4): 153-158
- URL: https://www.wjgnet.com/2307-8960/full/v5/i4/153.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i4.153