Copyright
©The Author(s) 2016.
World J Clin Cases. Oct 16, 2016; 4(10): 344-350
Published online Oct 16, 2016. doi: 10.12998/wjcc.v4.i10.344
Published online Oct 16, 2016. doi: 10.12998/wjcc.v4.i10.344
Figure 1 A metallic foreign body (white arrow) embedded in the lateral side of the left orbit.
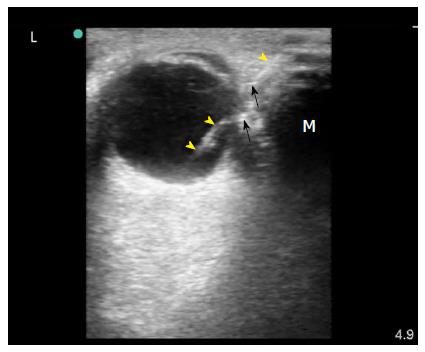
Figure 2 Surgeon performed point-of-care ultrasound of the left eye using a linear probe under sterile conditions with minimum pressure.
It showed a foreign body (yellow arrow heads) which was most probably touching the eye globe without penetration because the left eye moved freely. Gas bubbles were seen as shiny white dots within the wound (black arrows). The foreign body caused a mirror artefact (M) of the eye globe on its other side.
Figure 3 Plain computed tomography scan of the orbits showing the foreign body touching the left eye globe (yellow arrow).
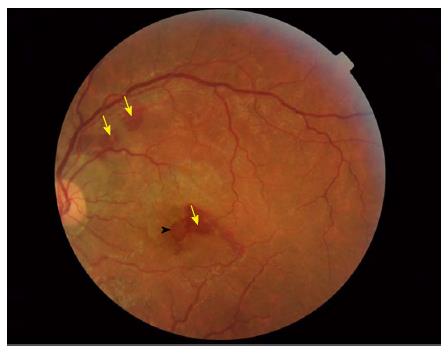
Figure 4 Fundoscopy showing retinal haemorrhages (yellow arrows) and a possible macular hole (black arrow head).
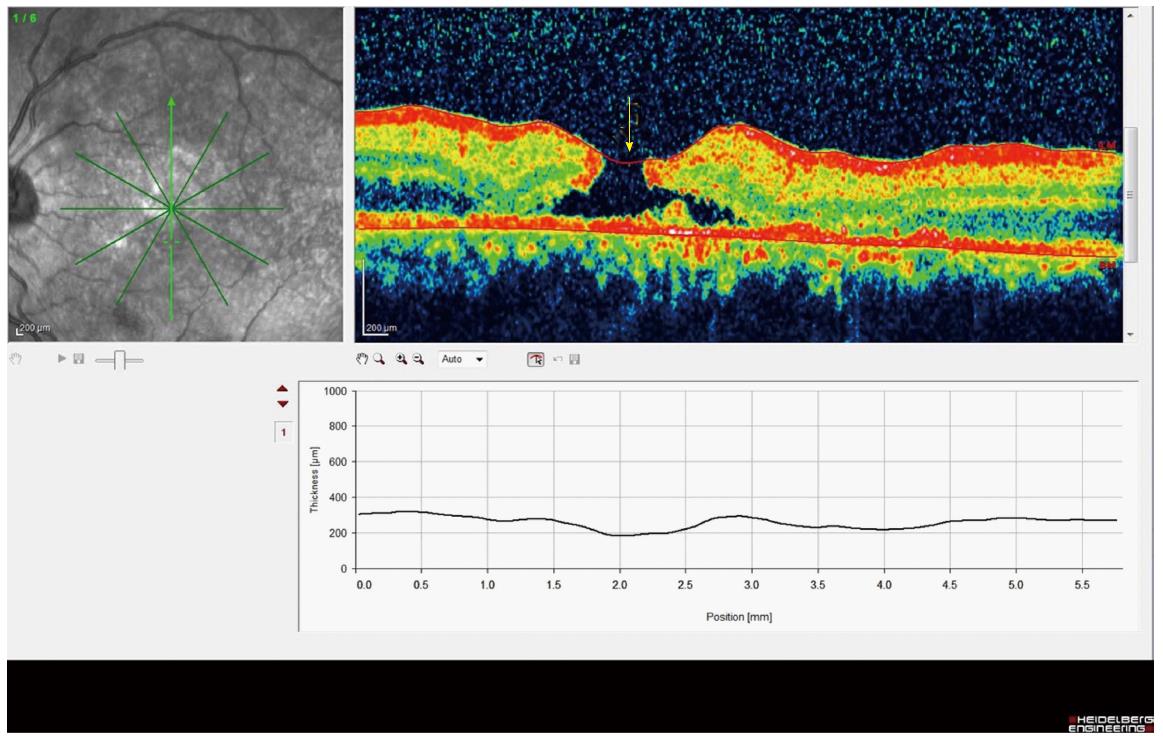
Figure 5 Optical coherence tomography showing a full thickness macular hole of the retina of the left eye (yellow arrow).
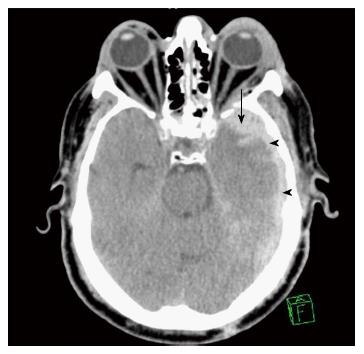
Figure 6 Brain computed tomography scan showing thin left subdural haematoma (arrow heads) associated with left parenchymal haemorrhagic contusion (arrow).
Figure 7 Examination of the left eye showed raccoon eye, an oedematous left eye lid, and severe ecchymosis of the conjunctiva.
The left pupil was dilated and not reactive to light.
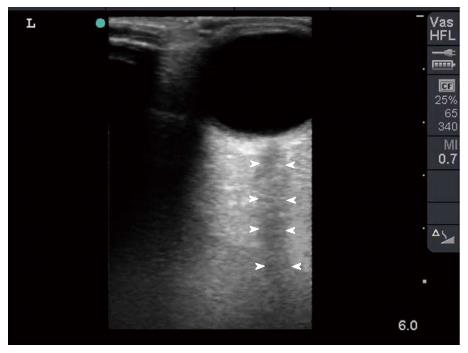
Figure 8 Bedside surgeon-performed point-of-care ultrasound of the left eye was normal.
There was no intraocular bleeding, the optic nerve was intact (arrow heads), and there was not retro-bulbar haematoma.
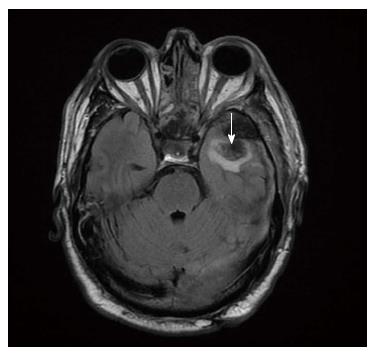
Figure 9 Magnetic resonance imaging confirmed that both optic nerves were intact.
Parenchymal haemorrhagic contusion is seen on the left side (arrow).
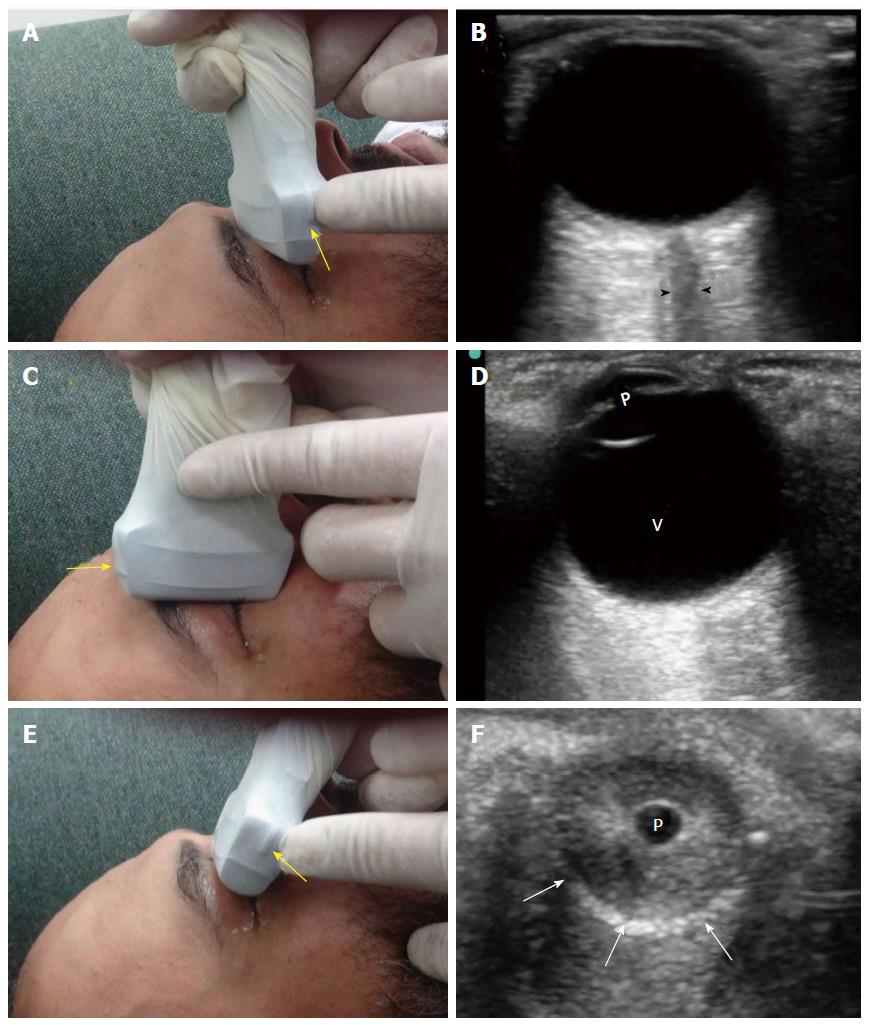
Figure 10 There are three common views to examine the eye.
The transverse antero-posterior view (A) is useful for examining the optic nerve (B, arrow heads). The sagittal antero-posterior view (C) is useful in visualizing the anterior and posterior chambers of the eye (D, V: Vitreous; p: Pupil). The coronal view (E) is useful for examining the pupil (F, p: Pupil, white arrows: Edge of the iris). The marker of the probe (yellow arrows) should point to the right side of the patient or upwards.
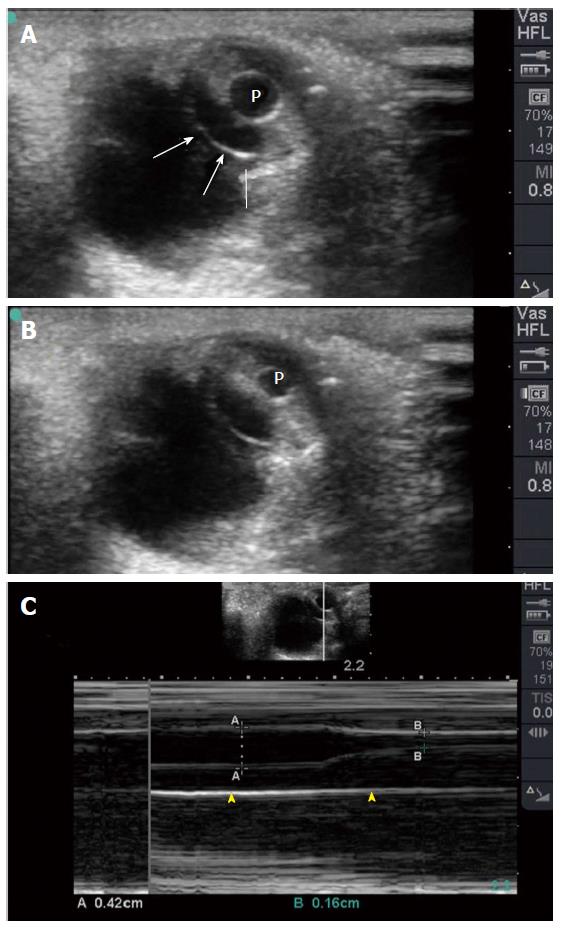
Figure 11 Coronal eye view (A) showing the pupil and edge of the iris (white arrows).
The pupil (P) constricts when light is applied to the closed eye (B). M Mode (C) accurately measures the size of the pupil which constricted from 4.2 mm to 1.6 mm to light reflex.
- Citation: Abu-Zidan FM, Balac K, Bhatia CA. Surgeon-performed point-of-care ultrasound in severe eye trauma: Report of two cases. World J Clin Cases 2016; 4(10): 344-350
- URL: https://www.wjgnet.com/2307-8960/full/v4/i10/344.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i10.344