Copyright
©The Author(s) 2024.
World J Clin Cases. May 16, 2024; 12(14): 2350-2358
Published online May 16, 2024. doi: 10.12998/wjcc.v12.i14.2350
Published online May 16, 2024. doi: 10.12998/wjcc.v12.i14.2350
Figure 1 Flow diagram of study cohort.
DLG: Direct lymphangiography; PB: Plastic bronchitis; CTL: Computed tomography lymphangiography.
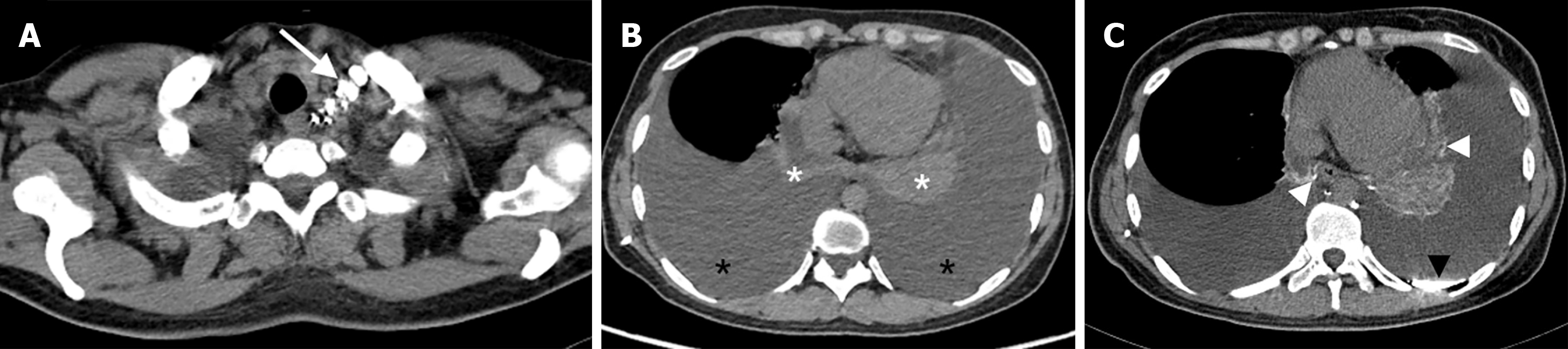
Figure 2 A 34-year-old woman with primary chylothorax.
A: The axial computed tomography lymphangiography (CTL) shows abnormal contrast medium accumulation in the thoracic duct outlet (long white arrow); B: A nonenhanced axial CT scan shows massive bilateral pleural effusions (black asterisk). Compressive atelectasis can be seen in both lungs (white asterisk); C: The CTL in the same plane as B shows abnormal contrast medium accumulation in the left pleura (black arrowhead), bilateral lung tissue (white arrowhead).
Figure 3 A 16-year-old woman with primary chylothorax.
A: The contrast-enhanced thoracic axial mediastinal window shows diffuse mediastinal soft-tissue infiltration (long white arrow), right pleural effusion (short white arrow), left pleural thickening (white arrowhead); B: The computed tomography lymphangiography in the same plane as A shows abnormal contrast medium scattered in surrounding mediastinum (short black arrow).
Figure 4 A 28-year-old man with plastic bronchitis.
The axial omputed tomography lymphangiography shows an abnormal contrast medium surrounding the right main bronchus (long white arrow), right hilar lung (short white arrow).
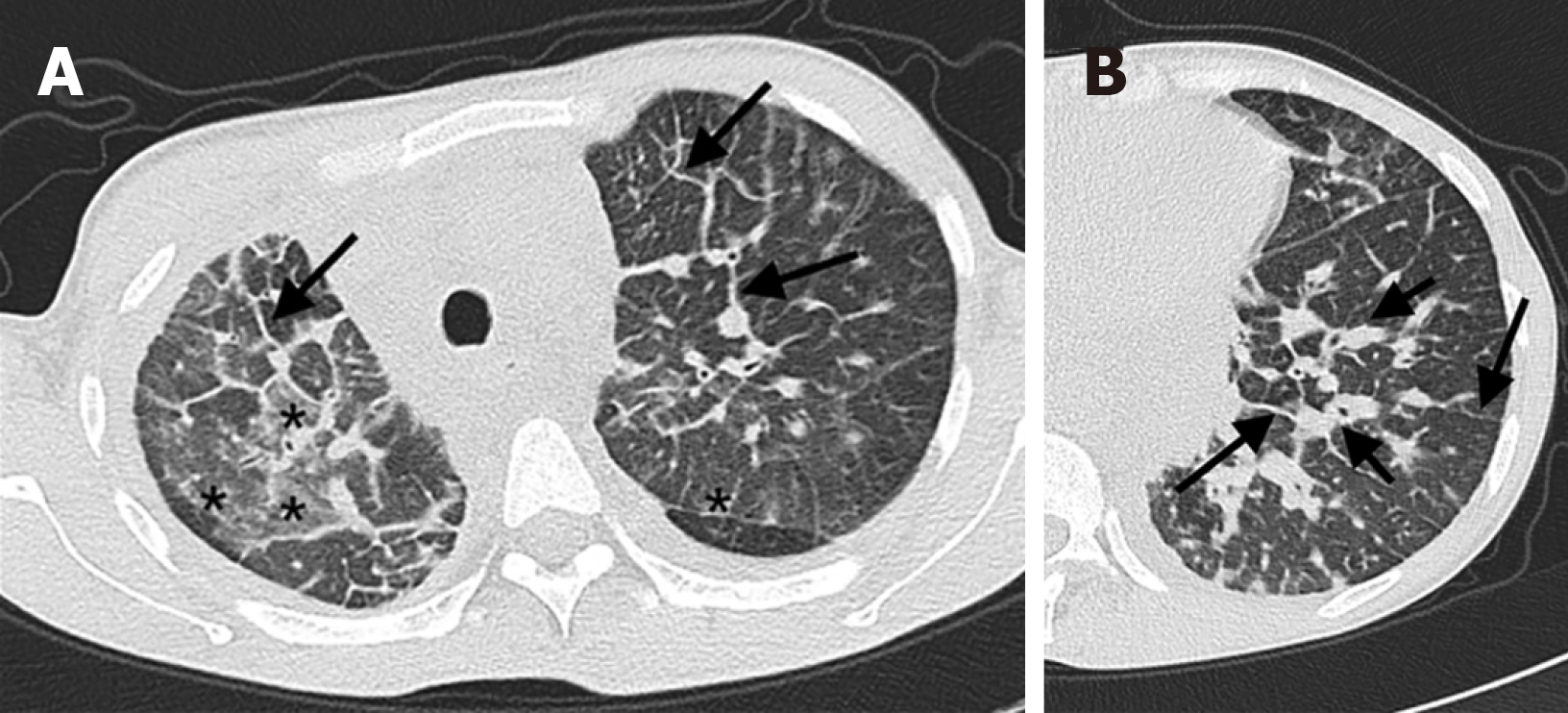
Figure 5 A 41-year-old woman with plastic bronchitis and primary chylothorax.
A and B: The thoracic axial lung window shows interlobular septal thickening (long black arrow), bronchovascular bundles thickening (short black arrow), diffuse ground-glass opacities in pulmonary parenchyma (black asterisk).
- Citation: Li XP, Zhang Y, Sun XL, Hao K, Liu MK, Hao Q, Wang RG. Lymphatic plastic bronchitis and primary chylothorax: A study based on computed tomography lymphangiography. World J Clin Cases 2024; 12(14): 2350-2358
- URL: https://www.wjgnet.com/2307-8960/full/v12/i14/2350.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i14.2350