Peer-review started: October 8, 2015
First decision: December 4, 2015
Revised: January 9, 2016
Accepted: January 29, 2016
Article in press: January 31, 2016
Published online: May 12, 2016
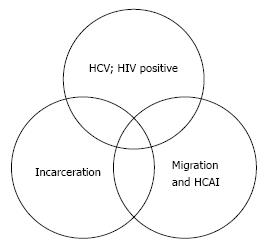
This review analyses current data concerning co-infection with hepatitis C virus (HCV) and human T lymphotropic virus (HTLV)-1/2 in people who inject drugs (PWID), with a particular focus on disease burden and global implications for virological outcome. In addition, the available treatment options for HTLV-1/2 are summarized and the ongoing and likely future research challenges are discussed. The data in this review was obtained from 34 articles on HCV/HTLV-1/2 co-infection in PWID retrieved from the PubMed literature database and published between 1997 and 2015. Despite unavailable estimates of the burden of HCV/HTLV-1/2 co-infection in general, the epidemiologic constellation of HTLV-1/2 shows high incidence in PWID with history of migration, incarceration, and other blood-borne infectious diseases such as HCV or human immunodeficiency virus. The most recent research data strongly suggest that HTLV-1 co-infection can influence HCV viral load, HCV sustained virological response to α-interferon treatment, and HCV-related liver disease progression. In short, outcome of HCV infection is worse in the context of HTLV-1 co-infection, yet more studies are needed to gain accurate estimations of the burden of HCV/HTLV-1/2 co-infections. Moreover, in the current era of new direct-acting antiviral treatments for HCV and proven HTLV-1/2 treatment options, prospective clinical and treatment studies should be carried out, with particular focus on the PWID patient population, with the aim of improving virological outcomes.
Core tip: People who inject drugs (PWID) are at higher risk of infection with blood-borne viruses and even co-infections. Co-infections with human immunodeficiency virus and human T lymphotropic virus (HTLV)-1/2 are common, and well-studied, among PWID; however, the rise of HTLV-1/2 co-infections with hepatitis C virus (HCV) has gained much research attention and studies have shown that the former influences the chronic disease course of the latter. This review summarizes the data from 34 articles on HCV/HTLV-1/2 co-infection in the PWID patient population, including current treatment options and impact on virological outcome.
- Citation: Castro E, Roger E. Hepatitis C virus/human T lymphotropic virus 1/2 co-infection: Regional burden and virological outcomes in people who inject drugs. World J Virol 2016; 5(2): 68-72
- URL: https://www.wjgnet.com/2220-3249/full/v5/i2/68.htm
- DOI: https://dx.doi.org/10.5501/wjv.v5.i2.68
The rate of hepatitis C virus (HCV) infection has reached the level of a global epidemic, with an estimated burden of 2.8% seroprevalence (anti-HCV antibody) in over 185 million individuals from both developed and developing nations[1]. In Europe and the United States, however, HCV transmission occurs mainly through intravenous drug use[2,3]. While this practice facilitates spread of blood-borne viruses, including the human immunodeficiency virus (HIV) as well as the hepatitis B virus, it allows transmission of HCV much more efficiently, as evidenced by the higher incidence rates of HCV in people who inject drugs (PWID) vs those with HIV[3]. Specifically, the 2011 estimate of global PWID seroprevalence for HCV was 67.0%[4]. PWID are a select population subgroup with extremely high seroprevalences of HCV; as such, they represent a primary driving force of the current HCV epidemic in high-resource settings, accounting for the majority of new (80%) and existing (60%) cases reportedly[5]. Yet, the high proportion of undiagnosed asymptomatic HCV carriers has precluded obtainment of an accurate estimate of chronic hepatitis C burden.
Human T lymphotropic virus (HTLV)-1 is an oncogenic retrovirus with a similar worldwide incidence. Although its founder effect remains unresolved, HTLV-1 shows high endemicity in Southwestern Japan, sub-Saharan Africa, South America, the Caribbean basin, the Middle East, and Australo-Melanesia[6]. The worldwide prevalence estimate of 20 million infected people is based on a serological screening from nearly 30 years ago, and an accurate estimate of the current global burden is unavailable[7]. The main transmission routes are contaminated blood products, sexual intercourse, and vertical transmission. In Europe, most HTLV-1 carriers are descendants of immigrants originally from regions with high endemicity and often with an HIV co-infection[6,7]. However, as reported for Spain, Italy and Ireland, PWID represent an especially affected population for HTLV-1 infection, even though HTLV-2 is much more prevalent[6]. In contrast, clinical onset of associated chronic illnesses, such as cancer [adult T-cell leukaemia/lymphoma (ATLL)] and neurological disorders [myelopathy and tropical spastic paraparesis (HAM/TSP)], has been reported in only 5%-10% of HTLV-1 carriers[8-10].
Similar to HTLV-1, HTLV-2 can be transmitted intravenously, sexually, or vertically. In the United States and Europe, needle sharing is a major route of HTLV-2 transmission among the PWID population[11-13]. Moreover, study of a cohort of PWID in the United States revealed significant associations between HTLV-2 infection and increased rates of pneumonia, acute bronchitis, urinary tract infection, and myelopathy[14], and the authors noted that the observed high correlation of HTLV-2 infection with HCV infection was suggestive of injection practices as a major route of transmission.
Studies of retroviral transmission carried out in various developing countries have identified incarceration as a risk factor, especially for HCV, suggesting that incarceration may be a surrogate marker for risky behaviour in general, such as needle sharing and unprotected sex[14]. In addition, our previous case report of HTLV in Eastern European countries indicated that the criminalization of drug use and lack of harm reduction strategies in prisons may also serve to increase risk for sexual and parental transmission[15].
Finally, the contribution of health care-associated infection (or “nosocomial”) as a source of HCV and retrovirus transmission among migrant population originally coming from limited resources settings has been largely undervalued to date, with little research available[16]. The limited data reported has shown nosocomial rates ranging from as low as 5% and all the way up to 19%[16].
In conclusion, the epidemiological constellation of HCV/HTLV-1/2 co-infection is found within regions with high rates of PWID and history of other risk factors (Figure 1).
In order to gain a comprehensive overview of the current available knowledge on the clinical and therapeutic implications of HCV/HTLV-1/2 co-infection, we searched the PubMed (https://www.ncbi.nlm.nih.gov/pubmed/) literature database for all articles affiliated with the terms “HTLV HCV”, “HCV and HTLV coinfection”, “HTLV burden”, “HTLV treatment”, and “HTLV migrants”. Exclusion of articles published before January 1, 1990 left a total of 34 studies for review.
A large-scale survey of residents of Iki Island in Japan, an endemic region for HTLV-1 infection, conducted by Kishihara et al[17] showed that individuals with HCV/HTLV-1 co-infection had a lower rate of natural clearance of HCV RNA and of sustained virological response to interferon (IFN) treatment than their counterparts with HCV infection alone; moreover, the co-infected population showed significantly higher HCV viremia (P < 0.05). Other Japanese studies of HCV/HTLV-1 co-infection in PWID showed associations with liver disease (6-fold increased risk)[18] and liver cancer mortality (2.6-fold increased risk)[19], leading to the hypothesis of an HTLV-1–induced immune modulation and inflammatory cytokine dysregulation that could affect HCV persistence and progression to liver disease[20,21]. In contrast to the Japanese findings, however, two Brazilian studies[22,23] of HCV/HTLV-1 co-infection provide epidemiological and immunological evidence of a higher rate of spontaneous clearance of HCV in patients with HIV/HTLV-1 co-infection as compared to patients harbouring only an HIV/HCV co-infection or an HCV mono-infection. The differences between HCV and HTLV-1 interaction outcomes in these two settings may be due to host genetic factors (e.g., HLA genotypes), study design, or other unmeasured parameters of the study populations. Studies of the molecular underpinnings of the HCV and HTLV-1 interaction outcomes have shown that HTLV-1-infected T cells, together with viral gene expression and cellular signalling mechanisms, can trigger a strong virus-specific immune response and increased proinflammatory cytokine production[24,25]. Moreover, the cellular immune response has been implicated in the control of HTLV-1 infection as well as in the development of related inflammatory alterations in patients[26]. The cellular immune response involves CD4+ T cells differentiating towards the Th1, Th2 and Th17 lineages, producing a variety of proinflammatory cytokines, chemokines, adhesion molecules and proinflammatory enzymes, which contribute to chronic inflammatory conditions and include reactive oxygen species (ROS), tumour necrosis factor alpha (TNFα), interleukins (IL1, 6, 8 and 18), nuclear factor-kappa B (NF-κB), hypoxia-inducible factor (HIF), IFNγ, and cyclooxygenase (COX)[27,28]. Moreover, contributions of different HTLV-1 oncogenic pathways related to viral proteins have been recently described recently[29]. Additionally, a study of 199 HTLV-1 infected subjects by Treviño et al[30] showed that the risk of developing TSP was 10-times higher among HTLV-1 carriers who harboured the IL B-28 CT and TT alleles than their counterparts who harboured the CC allele. The same study also showed an association between the CT polymorphism and increased HTLV-1 viral loads, and that the CC allele is found more frequently among asymptomatic carriers of HTLV-1 (62%). Collectively, these data strongly suggest that HTLV-1 co-infection plays a role in HCV viremia and evolution, attainment of HCV sustained virological response to α-interferon treatment, and HCV-related liver disease progression. Briefly, the current evidence supports postulation of worsening of HCV infection in the context of HTLV-1 co-infection.
HTLV-1/2 asymptomatic carriers do not require treatment. However, for HTLV-1/2 carriers who experience clinical onset of ATLL or HAM/TSP the current treatment options are limited and those available have a suboptimal range of efficacy. A meta-analysis of ATLL antiviral therapies showed that α-IFN and zidovudine (AZT) combination can induce complete remission and produce a high (82%) 5-year survival rate in ATLL patients[31]. Another ATLL therapeutic approach, specifically the α-interferon, arsenic and AZT combination, was evaluated in a later study of 16 patients and showed induction of a beneficial cytokine modulation response with a shift from the pre-treatment Treg/Th2 phenotype to the Th1 phenotype post-treatment[32]. Thus, this triple drug combination may be a useful treatment approach to restore an immuno-competent microenvironment, which will enhance the eradication of ATL cells and the prevention of opportunistic infections. Yet another study evaluated the combination of valproate (VPA) and AZT in patients with advanced HAM/TSP and found that the treatment may control viral replication through inhibition of the virus reverse-transcriptase and/or its associated molecular machinery[33]. The same strategy has been evaluated in non-human primates (Papio papio) naturally infected with the simian T cell lymphotropic virus type 1 (STLV-1; the equivalent of HTLV-1 which also causes simian ATLL). The animals were asymptomatic carriers and treatment with AZT/VPA induced a reduction of viral load which relapsed after treatment interruption[34]. A study of the HIV integrase inhibitor drug, raltegravir, as treatment for HTLV-1 (evaluating 5 carriers, including 2 with HAM and 3 asymptomatic) showed achievement of a transitory viral load reduction during the 24 wk of treatment but with no main clinical improvement[35]. Finally, Abad-Fernández et al[36] reported the only study to date in our collected articles from the PubMed literature to assess the evolution of HTLV co-infection (including with HIV, HTLV-2 and HCV) among patients who received treatment for HCV and showed reduction of HTLV-2 viral load in response to the α-IFN and ribavirin combination treatment.
The main features of HCV/HTLV-1/2 co-infection, based on evidence reported in the current literature, are summarized in Table 1. Briefly, they highlight the role of PWID as a core affected population and the negative immune modulation effect of HTLV-1 co-infection in patients with chronic hepatitis C. At the same time, HCV/HTLV-1/2 co-infection remains an unresolved clinical challenge; prospective studies looking at the HTLV-1/2 infection outcome in subjects receiving new direct-acting antiviral treatments targeting the HCV infection will likely provide further insights towards improvement.
| HTLV-1/2 infections are found in HCV co-infected PWID worldwide, as a consequence of unsafe injection practices |
| HTLV-1 infection induces chronic inflammation and oncogenic cellular changes |
| HTLV-1 co-infection of chronic hepatitis C carriers can increase HCV viral load, accelerate liver disease progression, and favour onset of liver cancer |
| Evidence suggests that HTLV-1/2 clinical presentations can be linked to higher viral loads in contrast to asymptomatic HTLV-1/2 carriers |
| Available treatment data shows that HTLV-1/2 viral load can be suppressed but not eradicated |
The features listed in Table 1 are a source of new research questions to be addressed. In addition, they should challenge the clinical field to reflect on the pertinence of adding HTLV-1/2 screening for PWID patients and particularly in relation to caring for migrant populations from high endemic areas in different worldwide settings.
We are grateful to Mr. José Winkler (Social Educator from the Addiction Medicine Clinic staff) for editing the audio core tip that accompanies this paper.
P- Reviewer: Chen CJ, Roohvand F, Skrypnyk IN, Toyoda T S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57:1333-1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1770] [Cited by in F6Publishing: 1801] [Article Influence: 163.7] [Reference Citation Analysis (0)] |
| 2. | Esteban JI, Sauleda S, Quer J. The changing epidemiology of hepatitis C virus infection in Europe. J Hepatol. 2008;48:148-162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 314] [Cited by in F6Publishing: 334] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 3. | Alter MJ. Epidemiology of hepatitis C virus infection. World J Gastroenterol. 2007;13:2436-2441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 838] [Cited by in F6Publishing: 811] [Article Influence: 47.7] [Reference Citation Analysis (2)] |
| 4. | Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, Degenhardt L. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378:571-583. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 949] [Cited by in F6Publishing: 936] [Article Influence: 72.0] [Reference Citation Analysis (0)] |
| 5. | Grebely J, Matthews GV, Lloyd AR, Dore GJ. Elimination of hepatitis C virus infection among people who inject drugs through treatment as prevention: feasibility and future requirements. Clin Infect Dis. 2013;57:1014-1020. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Gessain A, Cassar O. Epidemiological Aspects and World Distribution of HTLV-1 Infection. Front Microbiol. 2012;3:388. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 798] [Cited by in F6Publishing: 920] [Article Influence: 76.7] [Reference Citation Analysis (0)] |
| 7. | Manns A, Hisada M, La Grenade L. Human T-lymphotropic virus type I infection. Lancet. 1999;353:1951-1958. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 211] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Zehender G, Colasante C, De Maddalena C, Bernini F, Savasi V, Persico T, Merli S, Ridolfo A, Santambrogio S, Moroni M. High prevalence of human T-lymphotropic virus type 1 (HTLV-1) in immigrant male-to-female transsexual sex workers with HIV-1 infection. J Med Virol. 2004;74:207-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Gonçalves DU, Proietti FA, Ribas JG, Araújo MG, Pinheiro SR, Guedes AC, Carneiro-Proietti AB. Epidemiology, treatment, and prevention of human T-cell leukemia virus type 1-associated diseases. Clin Microbiol Rev. 2010;23:577-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 305] [Cited by in F6Publishing: 300] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 10. | Proietti FA, Carneiro-Proietti AB, Catalan-Soares BC, Murphy EL. Global epidemiology of HTLV-I infection and associated diseases. Oncogene. 2005;24:6058-6068. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 659] [Cited by in F6Publishing: 636] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 11. | Hlela C, Shepperd S, Khumalo NP, Taylor GP. The prevalence of human T-cell lymphotropic virus type 1 in the general population is unknown. AIDS Rev. 2009;11:205-214. [PubMed] [Cited in This Article: ] |
| 12. | Krook A, Albert J, Andersson S, Biberfeld G, Blomberg J, Eklund I, Engström A, Julander I, Käll K, Martin C. Prevalence and risk factors for HTLV-II infection in 913 injecting drug users in Stockholm, 1994. J Acquir Immune Defic Syndr Hum Retrovirol. 1997;15:381-386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | de la Fuente L, Toro C, Soriano V, Brugal MT, Vallejo F, Barrio G, Jiménez V, Silva T. HTLV infection among young injection and non-injection heroin users in Spain: prevalence and correlates. J Clin Virol. 2006;35:244-249. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Zunt JR, Tapia K, Thiede H, Lee R, Hagan H. HTLV-2 infection in injection drug users in King County, Washington. Scand J Infect Dis. 2006;38:654-663. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Roger E, Castro E. Etude de cas: pertinence du dépistage de l’HTLV-1/2 chez les usagers de drogues IV en Europe. As oral presentation in proceedings of the IV Colloque international francophone sur le traitement de la dépendance aux opioïdes. TDO4, Brussels, Belgium. Available from: http://www.tdo4.be/programme/. [Cited in This Article: ] |
| 16. | World Health Organization 2010. The burden of health care-associated infections worldwide. Available from: http://www.who.int/gpsc/country_work/summary_20100430_en.pdf. [Cited in This Article: ] |
| 17. | Kishihara Y, Furusyo N, Kashiwagi K, Mitsutake A, Kashiwagi S, Hayashi J. Human T lymphotropic virus type 1 infection influences hepatitis C virus clearance. J Infect Dis. 2001;184:1114-1119. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Hisada M, Chatterjee N, Zhang M, Battjes RJ, Goedert JJ. Increased hepatitis C virus load among injection drug users infected with human immunodeficiency virus and human T lymphotropic virus type II. J Infect Dis. 2003;188:891-897. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Boschi-Pinto C, Stuver S, Okayama A, Trichopoulos D, Orav EJ, Tsubouchi H, Mueller N. A follow-up study of morbidity and mortality associated with hepatitis C virus infection and its interaction with human T lymphotropic virus type I in Miyazaki, Japan. J Infect Dis. 2000;181:35-41. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Casseb J. Possible mechanism for positive interaction of human T cell leukemia type I on liver disease in a hepatitis C virus-infected Japanese cohort. J Infect Dis. 2000;182:379-380. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Tokunaga M, Uto H, Oda K, Tokunaga M, Mawatari S, Kumagai K, Haraguchi K, Oketani M, Ido A, Ohnou N. Influence of human T-lymphotropic virus type 1 coinfection on the development of hepatocellular carcinoma in patients with hepatitis C virus infection. J Gastroenterol. 2014;49:1567-1577. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Bahia F, Novais V, Evans J, Le Marchand C, Netto E, Page K, Brites C. The impact of human T-cell lymphotropic virus I infection on clinical and immunologic outcomes in patients coinfected with HIV and hepatitis C virus. J Acquir Immune Defic Syndr. 2011;57 Suppl 3:S202-S207. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Le Marchand C, Bahia F, Page K, Brites C. Hepatitis C virus infection and spontaneous clearance in HTLV-1 and HIV co-infected patients in Salvador, Bahia, Brazil. Braz J Infect Dis. 2015;19:486-491. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Ouaguia L, Mrizak D, Renaud S, Moralès O, Delhem N. Control of the inflammatory response mechanisms mediated by natural and induced regulatory T-cells in HCV-, HTLV-1-, and EBV-associated cancers. Mediators Inflamm. 2014;2014:564296. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Araya N, Sato T, Yagishita N, Ando H, Utsunomiya A, Jacobson S, Yamano Y. Human T-lymphotropic virus type 1 (HTLV-1) and regulatory T cells in HTLV-1-associated neuroinflammatory disease. Viruses. 2011;3:1532-1548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Leal FE, Ndhlovu LC, Hasenkrug AM, Bruno FR, Carvalho KI, Wynn-Williams H, Neto WK, Sanabani SS, Segurado AC, Nixon DF. Expansion in CD39+ CD4+ immunoregulatory t cells and rarity of Th17 cells in HTLV-1 infected patients is associated with neurological complications. PLoS Negl Trop Dis. 2013;7:e2028. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006;72:1605-1621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 954] [Cited by in F6Publishing: 903] [Article Influence: 50.2] [Reference Citation Analysis (0)] |
| 28. | Raval GU, Bidoia C, Forlani G, Tosi G, Gessain A, Accolla RS. Localization, quantification and interaction with host factors of endogenous HTLV-1 HBZ protein in infected cells and ATL. Retrovirology. 2015;12:59. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Bidoia C. Human T-lymphotropic virus proteins and post-translational modification pathways. World J Virol. 2012;1:115-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Treviño A, Lopez M, Vispo E, Aguilera A, Ramos JM, Benito R, Roc L, Eiros JM, de Mendoza C, Soriano V. Development of tropical spastic paraparesis in human T-lymphotropic virus type 1 carriers is influenced by interleukin 28B gene polymorphisms. Clin Infect Dis. 2012;55:e1-e4. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Bazarbachi A, Plumelle Y, Carlos Ramos J, Tortevoye P, Otrock Z, Taylor G, Gessain A, Harrington W, Panelatti G, Hermine O. Meta-analysis on the use of zidovudine and interferon-alfa in adult T-cell leukemia/lymphoma showing improved survival in the leukemic subtypes. J Clin Oncol. 2010;28:4177-4183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 267] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 32. | Kchour G, Rezaee R, Farid R, Ghantous A, Rafatpanah H, Tarhini M, Kooshyar MM, El Hajj H, Berry F, Mortada M. The combination of arsenic, interferon-alpha, and zidovudine restores an «immunocompetent-like» cytokine expression profile in patients with adult T-cell leukemia lymphoma. Retrovirology. 2013;10:91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Mahieux R. [Virological aspects of HTLV-1 infection and new therapeutical concepts]. Bull Soc Pathol Exot. 2011;104:181-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Afonso PV, Mekaouche M, Mortreux F, Toulza F, Moriceau A, Wattel E, Gessain A, Bangham CR, Dubreuil G, Plumelle Y. Highly active antiretroviral treatment against STLV-1 infection combining reverse transcriptase and HDAC inhibitors. Blood. 2010;116:3802-3808. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 35. | Treviño A, Parra P, Bar-Magen T, Garrido C, de Mendoza C, Soriano V. Antiviral effect of raltegravir on HTLV-1 carriers. J Antimicrob Chemother. 2012;67:218-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Abad-Fernández M, Dronda F, Moreno A, Casado JL, Pérez-Elías MJ, Quereda C, Moreno S, Vallejo A. Brief Report: Reduced Cell-Associated HTLV-2 DNA in Antiretroviral Treated HIV-1-HCV-Coinfected Patients Who Either Received Interferon-α/Ribavirin-Based Hepatitis C Therapy or Had Spontaneous HCV RNA Clearance. J Acquir Immune Defic Syndr. 2015;69:286-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |