Copyright
©The Author(s) 2023.
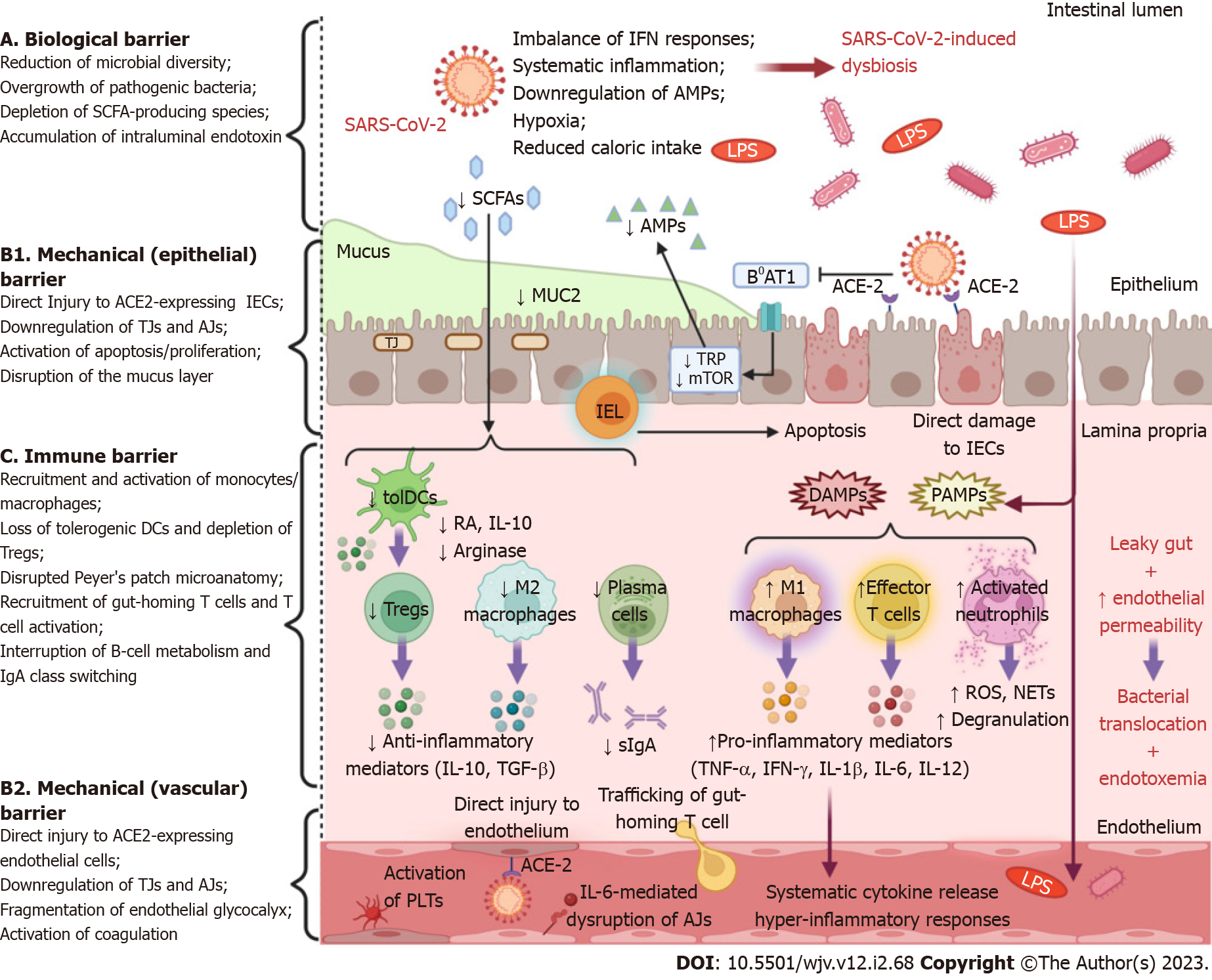
Figure 1 Schematic representation of intestinal barrier dysfunction in severe acute respiratory syndrome coronavirus 2 infection.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is associated with a multifaceted dysfunction of the gut barrier as it exerts detrimental effects on all of its major levels of defense. A: Systemic inflammation, an imbalance of interferon (IFN) responses, hypoxia or low blood flow, and reduced caloric intake, due to coronavirus disease 2019-associated cachexia, contribute to intestinal microbiome alterations. Gut dysbiosis is characterized by an overgrowth of opportunistic pathogens, which are a source of harmful substances, e.g., endotoxin, peptidoglycan, β-glucan, as well as a depletion of commensal microorganisms, which synthesize beneficial metabolites such as short-chain fatty acids; B: SARS-CoV-2 induces either direct cytopathic injury to angiotensin-converting enzyme 2 (ACE2)-expressing intestinal epithelial cells (IECs) and endothelial cells, or indirect immune-mediated damage, or both. Moreover, the secretion of mucin glycoproteins, the fundamental element of the mucus layer, is severely impaired. In addition, the virus undermines the expression of tight junction and adherens junction proteins, leading to increased paracellular permeability and structural destabilization of the epithelium and endothelium. Viral interference with ACE2 signaling attenuates the activity of the amino acid transporter B0AT1, which is necessary for intestinal absorption of tryptophan (TRP). As a result, TRP depletion downregulates the mammalian target of rapamycin pathway, which promotes the expression of antimicrobial peptides. The overwhelming intraepithelial CD8+ lymphocytes trigger the apoptosis of IECs, which is followed by reactive regeneration. In parallel, disease-activated and apoptotic endothelial cells are potent drivers of neutrophil/monocyte recruitment, platelet aggregation, and coagulation activation; C: Commensal-derived metabolites modulate innate immune responses by inducing tolerogenic dendritic cells and M2-polarized macrophages. SARS-CoV-2-induced dysbiosis eliminates these immunoregulatory effects, inhibits T regulatory (Treg) cell activity, and suppresses the secretion of anti-inflammatory cytokines such as interleukin 10 (IL-10) and transforming growth factor beta. The release of damage-associated molecular patterns from injured cells and the influx of pathogen-associated molecular patterns, as a result of leaky gut, orchestrate the recruitment and activation of innate immune cells that secrete pro-inflammatory mediators (IFN-γ, tumor necrosis factor alpha, IL-1β, IL-6, IL-12). Subsequently, this pro-inflammatory microenvironment precipitates the derangement of adaptive immune responses, as demonstrated by increased trafficking of gut-homing T cells and effector T cell predominance. Furthermore, interruption of B-cell metabolism, plasma cell differentiation, and immunoglobulin A (IgA) class switching impede the effective secretion of protective dimeric IgA. This multi-layered disruption of intestinal barrier integrity allows the dissemination of intraluminal bacteria and endotoxin into the mesenteric lymphatic vessel or/and into the systemic circulation (created with biorender.com). IEL: Intraepithelial lymphocyte; LPS: Lipopolysaccharides; MUC2: Mucin 2; NETs: Neutrophil extracellular traps; PLTs: Platelets; RA: Retinoic acid; ROS: Reactive oxygen species; sIgA: Secretory immunoglobulin A; SCFAs: Short-chain fatty acids.
- Citation: Tsounis EP, Triantos C, Konstantakis C, Marangos M, Assimakopoulos SF. Intestinal barrier dysfunction as a key driver of severe COVID-19. World J Virol 2023; 12(2): 68-90
- URL: https://www.wjgnet.com/2220-3249/full/v12/i2/68.htm
- DOI: https://dx.doi.org/10.5501/wjv.v12.i2.68