Published online Jan 7, 2025. doi: 10.5499/wjr.v12.i1.101278
Revised: December 4, 2024
Accepted: December 30, 2024
Published online: January 7, 2025
Processing time: 118 Days and 14.6 Hours
Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome, a rare inflammatory disease, was described in 1987 by Chamot et al, who identified its common characteristics and transitional forms through case reports. The inci
We present the case of a 44-year-old male patient who had previously been diagnosed with SAPHO syndrome. Following a two-year cessation of methotrexate therapy, he experienced recurrent anterior chest wall and joint pain accompanied by dyspnea. We conducted a comprehensive examination for the patient, which included physical examination, laboratory tests, and imaging studies. The clinical presentation and treatment outcomes suggest that his pneumothorax was related to an episode of SAPHO syndrome. We performed closed thoracic drainage surgery for the patient and treated his symptoms with etoricoxib (60 mg daily). Upon discharge, methotrexate was prescribed again. In subsequent follow-ups, there was no recurrence of joint and respiratory symptoms observed in the patient.
SAPHO syndrome has been proposed as a transitional stage between ankylosing spondylitis and psoriatic arthritis. One study reported a 0.29% incidence of spontaneous pneumothorax in patients with ankylosing spondylitis, higher than in the general population. Additionally, 30% of patients with SAPHO syndrome test positive for HLA-B27, an antigen linked to ankylosing spondylitis. Symptomatically, some patients with SAPHO syndrome meet diagnostic criteria for ankylosing spondylitis, with sternoclavicular joint involvement and paravertebral ossifications resembling syndesmophytes in ankylosing spondylitis. These features suggest a possible linked between SAPHO syndrome and ankylosing spondylitis.
Core Tip: This case report introduces a novel association between synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome and pneumothorax. The 44-year-old patient’s diagnosis and treatment underscore the importance of recognizing this rare but serious condition, broadening our understanding of SAPHO syndrome’s clinical manifestations.
- Citation: Zheng ZX, Gu MJ, Kang TL, Zhang YR, Wang YN, Li C, Wu YH. Synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome as a cause of pneumothorax: A case report. World J Rheumatol 2025; 12(1): 101278
- URL: https://www.wjgnet.com/2220-3214/full/v12/i1/101278.htm
- DOI: https://dx.doi.org/10.5499/wjr.v12.i1.101278
Synovitis, acne, pustulosis, hyperostosis, and osteitis (SAPHO) syndrome, a rare inflammatory disease, was described in 1987 by Chamot et al[1] who identified its common characteristics and transitional forms through case reports. The incidence rate is now 1 in 10000 among Caucasians and 0.00144 in 10000 among Japanese[2].
Pneumothorax occurs when gas enters the pleural cavity, typically due to lung disease or chest trauma, and is characterized as either spontaneous or traumatic[3]. Spontaneous pneumothorax is commonly linked to congenital lung tissue abnormalities or lung conditions, such as ruptured pulmonary bullae, emphysema, and bronchial asthma. Respiratory involvement in SAPHO syndrome has historically been noted. In this report, we present a case of a 44-year-old man who developed pneumothorax following SAPHO syndrome diagnosis.
The patient reported recurrent anterior chest wall and joint pain accompanied by dyspnea for thirteen days.
Two years after discontinuing methotrexate use, he experienced recurrent anterior chest wall and joint pain accompanied by dyspnea. He denied a history of coronary heart disease, diabetes, chronic obstructive pulmonary disease, tuberculosis, and smoking. He presented with right-sided chest pain and tenderness on chest palpation, and his oxygen saturation was 94%.
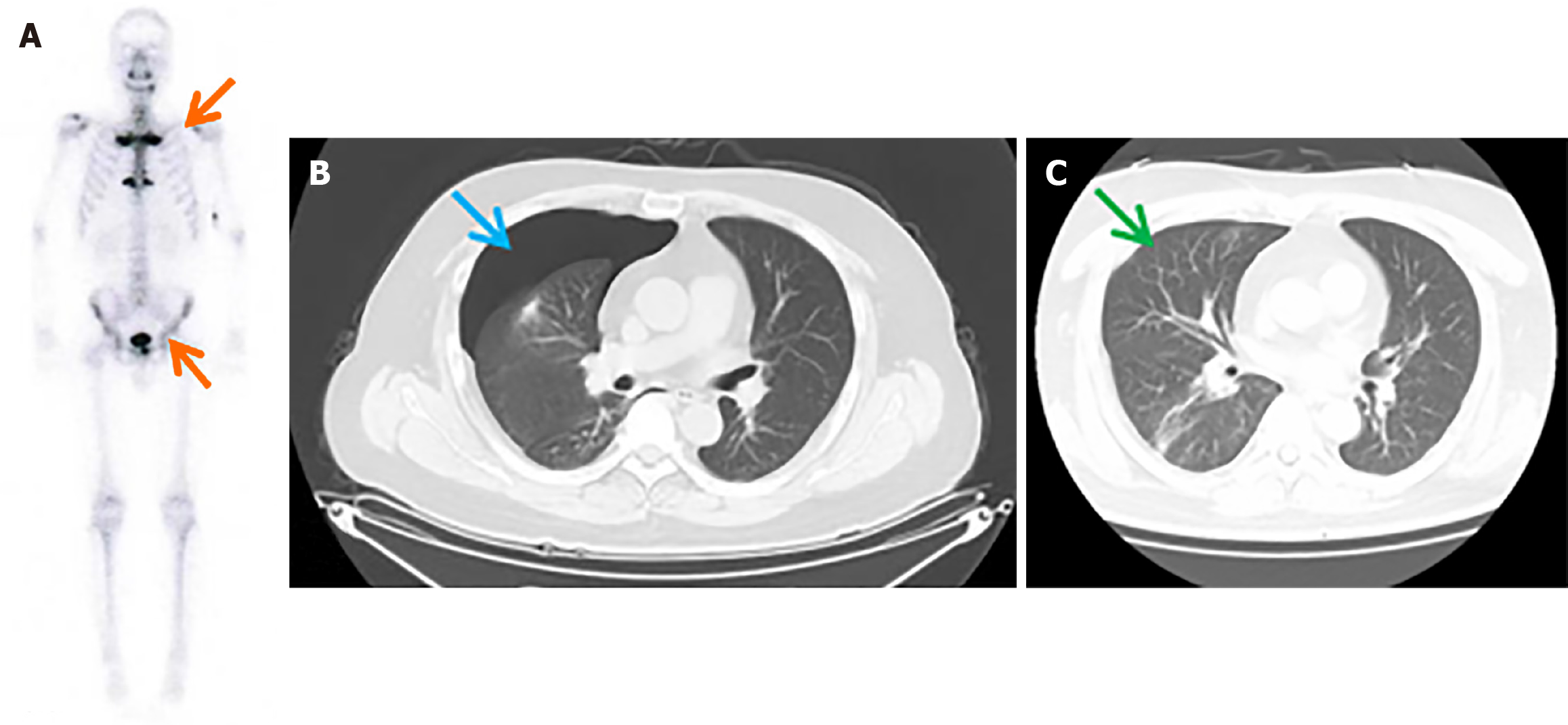
The patient, hypertensive for 10 years, presented with palmoplantar pustulosis and anterior chest wall pain lasting 2 years. Technetium-99m methylene diphosphonate (99mTc-MDP) bone scintigraphy revealed radioactive element accumulation in the bilateral sternoclavicular joints (Figure 1A). Based on his symptoms and imaging findings, the patient was diagnosed with SAPHO syndrome. He was treated with methotrexate for 1 year, which relieved his skin and joint pain, after which the treatment was discontinued.
He denied a history of coronary heart disease, diabetes, chronic obstructive pulmonary disease, tuberculosis, and smoking.
He presented with right-sided chest pain and tenderness on chest palpation, and his oxygen saturation was 94%.
Tuberculosis was ruled out with a negative T-SPOT test. Blood tests indicated an elevated C-reactive protein level at 2.24 mg/dL (normal: < 0.3 mg/dL), whereas serum procalcitonin was negative, excluding bacterial infection.
Based on the patient’s symptoms and computed tomography (CT) imaging, he was diagnosed with right-sided pneumothorax (Figure 1B), and a chest radiograph revealed 37% lung collapse. The patient underwent closed thoracic drainage surgery, which alleviated his dyspnea, and follow-up chest CT one week later confirmed no pneumothorax (Figure 1C).
The clinical presentation and treatment outcomes suggest that his pneumothorax was related to an episode of SAPHO syndrome.
The patient underwent closed thoracic drainage surgery, which alleviated his dyspnea, and follow-up chest CT one week later confirmed no pneumothorax (Figure 1C). Subsequent treatment with etoricoxib (60 mg daily) relieved his anterior chest wall and joint pain.
Following the discontinuation of methotrexate two years prior, the patient resumed the medication regimen, and in our subsequent follow-up, no recurrence of joint and respiratory symptoms was observed.
The occurrence of pulmonary and pleural lesions in SAPHO syndrome is not uncommon. The first reported case of SAPHO syndrome complicated by pleural effusion appeared in 1999[4]. In a previous study evaluating high-resolution CT findings in the lungs of patients with SAPHO syndrome, irregular linear opacities were observed in 29 (43.3%) patients, opacities in 22 (32.8%), ground-glass opacities in 11 (16.4%), pleural thickening in 9 (13.4%), solitary nodules in 6 (9%), bronchiectasis in 3 (4.5%), pulmonary bulla in 2 (3%), multiple nodules in 1 (1.5%), and reticular patterns in 1 (1.5%)[5]. However, a literature search on respiratory manifestation in patients with SAPHO syndrome did not identify any previously reported cases involving pneumothorax or its symptoms.
SAPHO syndrome has been proposed as a transitional stage between ankylosing spondylitis and psoriatic arthritis[6,7]. One study reported a 0.29% incidence of spontaneous pneumothorax in patients with ankylosing spondylitis, higher than in the general population[8]. Additionally, 30% of patients with SAPHO syndrome test positive for HLA-B27[9], an antigen linked to ankylosing spondylitis. Symptomatically, some patients with SAPHO syndrome meet diagnostic criteria for ankylosing spondylitis, with sternoclavicular joint involvement and paravertebral ossifications resembling syndesmophytes in ankylosing spondylitis[10]. These features suggest a possible linked between SAPHO syndrome and ankylosing spondylitis. The present case report is the first to document the coexistence of SAPHO syndrome and pneumothorax.
This case report underscores a novel association between SAPHO syndrome and spontaneous pneumothorax, previously unreported. The patient's recovery following treatment and the absence of symptom recurrence upon methotrexate resumption suggest a potential link between SAPHO syndrome and pneumothorax development. This observation warrants further investigation into the relationship between these conditions and the need for vigilant monitoring of respiratory issues in SAPHO syndrome patients.
| 1. | Chamot AM, Benhamou CL, Kahn MF, Beraneck L, Kaplan G, Prost A. [Acne-pustulosis-hyperostosis-osteitis syndrome. Results of a national survey. 85 cases]. Rev Rhum Mal Osteoartic. 1987;54:187-196. [PubMed] [Cited in This Article: ] |
| 2. | Bintcliffe OJ, Hallifax RJ, Edey A, Feller-Kopman D, Lee YC, Marquette CH, Tschopp JM, West D, Rahman NM, Maskell NA. Spontaneous pneumothorax: time to rethink management? Lancet Respir Med. 2015;3:578-588. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Kurata I, Tsuboi H, Terasaki M, Shimizu M, Toko H, Honda F, Ohyama A, Yagishita M, Osada A, Ebe H, Kawaguchi H, Takahashi H, Hagiwara S, Asashima H, Kondo Y, Matsumoto I, Sumida T. Effect of Biological Disease-modifying Anti-rheumatic Drugs on Airway and Interstitial Lung Disease in Patients with Rheumatoid Arthritis. Intern Med. 2019;58:1703-1712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Dumolard A, Gaudin P, Juvin R, Bost M, Peoc'h M, Phelip X. SAPHO syndrome or psoriatic arthritis? A familial case study. Rheumatology (Oxford). 1999;38:463-467. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Li C, Liu S, Sui X, Wang J, Song W, Xu W, Xu KF, Tian X, Zhang W. Pulmonary high-resolution computed tomography findings in patients with synovitis, acne, pustulosis, hyperostosis and osteitis syndrome. PLoS One. 2018;13:e0206858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Colina M, Govoni M, Orzincolo C, Trotta F. Clinical and radiologic evolution of synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome: a single center study of a cohort of 71 subjects. Arthritis Rheum. 2009;61:813-821. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in RCA: 156] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 7. | Hayem G, Bouchaud-Chabot A, Benali K, Roux S, Palazzo E, Silbermann-Hoffman O, Kahn MF, Meyer O. SAPHO syndrome: a long-term follow-up study of 120 cases. Semin Arthritis Rheum. 1999;29:159-171. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 310] [Cited by in RCA: 276] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 8. | Danve A. Thoracic Manifestations of Ankylosing Spondylitis, Inflammatory Bowel Disease, and Relapsing Polychondritis. Clin Chest Med. 2019;40:599-608. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Maugars Y, Berthelot JM, Ducloux JM, Prost A. SAPHO syndrome: a followup study of 19 cases with special emphasis on enthesis involvement. J Rheumatol. 1995;22:2135-2141. [PubMed] [Cited in This Article: ] |
| 10. | Shen K, Yang CL, Yin G, Xie QB. Sacroiliitis and Spondylitis with Sternoclavicular Hyperostosis: SAPHO or an Ankylosing Spondylitis Variant? Chin Med J (Engl). 2016;129:110-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |