Copyright
©The Author(s) 2017.
World J Crit Care Med. Feb 4, 2017; 6(1): 28-36
Published online Feb 4, 2017. doi: 10.5492/wjccm.v6.i1.28
Published online Feb 4, 2017. doi: 10.5492/wjccm.v6.i1.28
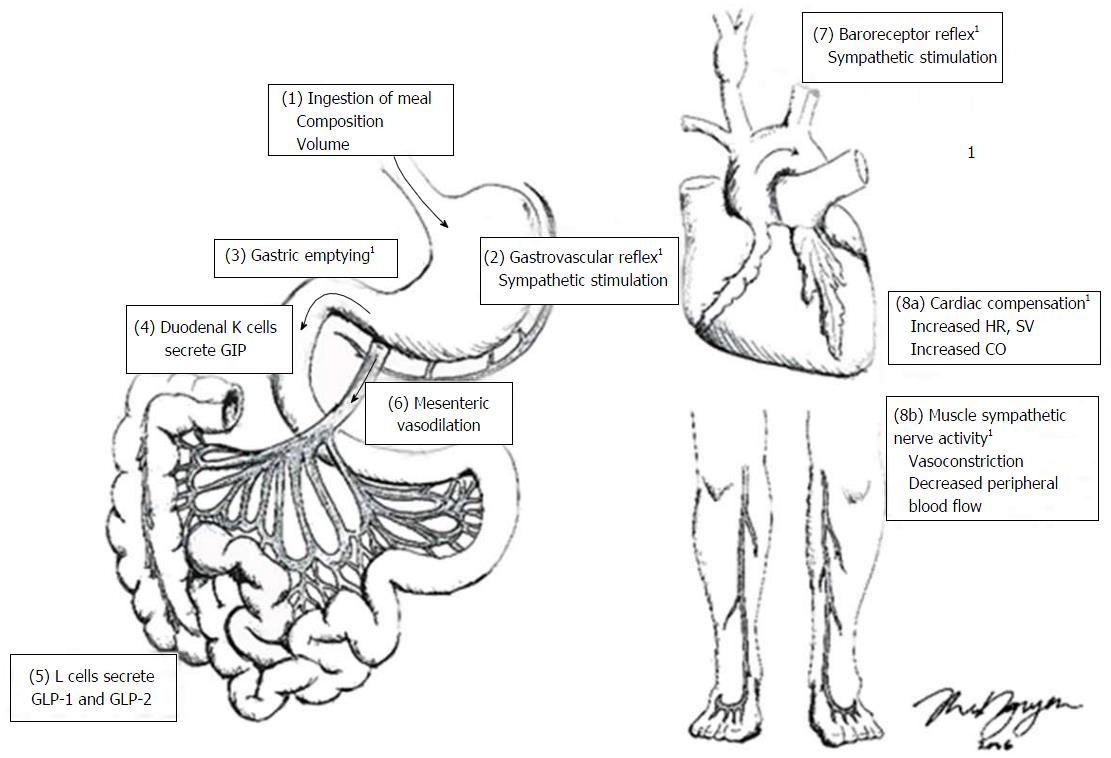
Figure 1 Factors involved in the regulation of postprandial blood pressure.
(1) ingestion of a meal, with a greater carbohydrate load results in a greater postprandial hypotensive response; (2) Meal-induced gastric distension from the meal triggers stretch receptors in the stomach wall, increasing sympathetic nerve outflow; (3) gastric content is emptied into the small intestine, and, in response to the nutrient in the small intestine; (4, 5) gastrointestinal peptides are secreted from the small intestine (e.g., GLP-1 and GLP-2, glucagon-like peptide-1 and 2; GIP, glucose insulinotropic polypeptide); (6) gastrointestinal peptides stimulate mesenteric vessel dilation; (7) this results in reduced circulating blood volume and the reduction in blood pressure is detected by baroreceptors; (8a) the “gastrovascular” and baroreceptor reflexes stimulate sympathetic activity to increase heart rate (HR), stroke volume (SV) and thus cardiac output (CO) to maintain postprandial blood pressure; (8b) skeletal vasculature constricts to decrease peripheral blood flow. 1These factors are affected by age and have been identified as potential pathophysiological mechanisms of postprandial hypotension. Figure drawn by Ms. T. Nguyen. GIP: Glucose-dependent insulinotropic peptide; GLP: Glucagon-like peptide.
- Citation: Nguyen TA, Abdelhamid YA, Phillips LK, Chapple LS, Horowitz M, Jones KL, Deane AM. Nutrient stimulation of mesenteric blood flow - implications for older critically ill patients. World J Crit Care Med 2017; 6(1): 28-36
- URL: https://www.wjgnet.com/2220-3141/full/v6/i1/28.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v6.i1.28