Published online Dec 28, 2023. doi: 10.5412/wjsp.v13.i3.14
Peer-review started: September 23, 2023
First decision: November 1, 2023
Revised: November 18, 2023
Accepted: December 19, 2023
Article in press: December 19, 2023
Published online: December 28, 2023
Processing time: 94 Days and 5.5 Hours
Mesh utilization for ventral hernia repair is associated with potential complications such as mesh infections, adhesions, seromas, fistula formation and signi
To evaluate the short term outcomes when the modified RMR was used to repair ventral hernias.
This was a 5-year prospective study that examined the outcome of all consecutive patients with ventral abdominal wall hernias > 5 cm in maximal diameter who underwent repair using the modified RMR technique in a single surgeon unit. Patients were reviewed in an outpatient clinic at 3, 6 and 12 mo and evaluated for hernia recurrence on clinical examination. Each patient’s abdominal wall was also assessed with using ultrasonography at 24 mo to detect recurrences. All data were examined with SPSS ver 18.0.
Over the 5-year study period, there were 52 patients treated for ventral hernias at this institution. Four patients were excluded and there were 48 in the final study sample, at a mean age of 56 years (range 28-80). The mean maximal diameter of the hernia defect was 7 cm (range 5-12 cm). There were 5 (10.4%) seromas and 1 recurrence (2.1%) at a mean of 36 mo follow-up.
The authors recommend the modified RMR as an acceptable alternative to mesh repair of ventral hernias. The seroma rate can be further reduced with routine use of drains. The modified RMR also has the benefit of eliminating all mesh-specific complications.
Core Tip: Mesh utilization for ventral hernia repair is associated with potential complications such as mesh infections, adhesions, seromas, fistula formation and significant postoperative pain. Using the modified Rectus Muscle Repair results in 10.4% seromas, which can be further reduced with routine use of drains. Using the modified Rectus Muscle Repair results in 2.1% recurrences at a mean of 36 mo follow up. The modified Rectus Muscle Repair is as an option to repair midline ventral hernias without mesh.
- Citation: Naraynsingh V, Cawich SO, Hassranah S. Alternative to mesh repair for ventral hernias: Modified rectus muscle repair. World J Surg Proced 2023; 13(3): 14-21
- URL: https://www.wjgnet.com/2219-2832/full/v13/i3/14.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v13.i3.14
In the 21st Century, most surgeons use mesh to repair midline ventral hernias in an attempt to lower recurrence rates[1]. However, mesh utilization is associated with potential complications such as mesh infections, adhesions, seromas, fistula formation and significant postoperative pain[2-7]. These have resulted in numerous lawsuits[8]. Moreover, in low and middle-income countries, both the cost of mesh and its inconstant availability are additional factors that limit its utilization.
The rectus muscle repair (RMR) was described in 1993 as an option to repair midline ventral hernias without mesh[9]. However, we noticed that this technique could not be applied to hernias > 6 cm in maximal diameter, and this prompted our development of a modified RMR, described in detail in a previous report[10].
The short-term recurrence and complication rates of the modified RMR are largely unknown, and this paper will make them clear. We carried out this study to evaluate the short-term outcomes when the modified RMR was used to repair ventral hernias.
This study was approved by the local institutional review board and performed at a tertiary referral hospital in Trinidad & Tobago, an island state in the Eastern Caribbean. This was a prospective study that spanned a period of 5 years, from January 1, 2015 to December 30, 2019. All consecutive patients who were referred to the surgical department with diagnoses of a ventral abdominal wall hernia were potential candidates for the study. We included all those who were above the age of 18 years, had hernia defects > 5 cm in maximal diameter, and consented to participate. Exclusion criteria included patients who were less than 18 years of age, did not consent to participate, had hernia defects larger than 15 cm in maximal diameter that did not allow primary closure, and those who desired mesh repairs. We collected the following data from all patients who underwent repair using the modified RMR technique in a single surgeon unit: patient demographics, complications, mortality and recurrences. Patients were reviewed in an outpatient clinic at 3, 6 and 12 mo and evaluated for hernia recurrence on clinical examination. Each patient’s abdominal wall was also assessed with using ultrasonography at 24 mo to detect recurrences. All data were examined with SPSS ver 18.0.
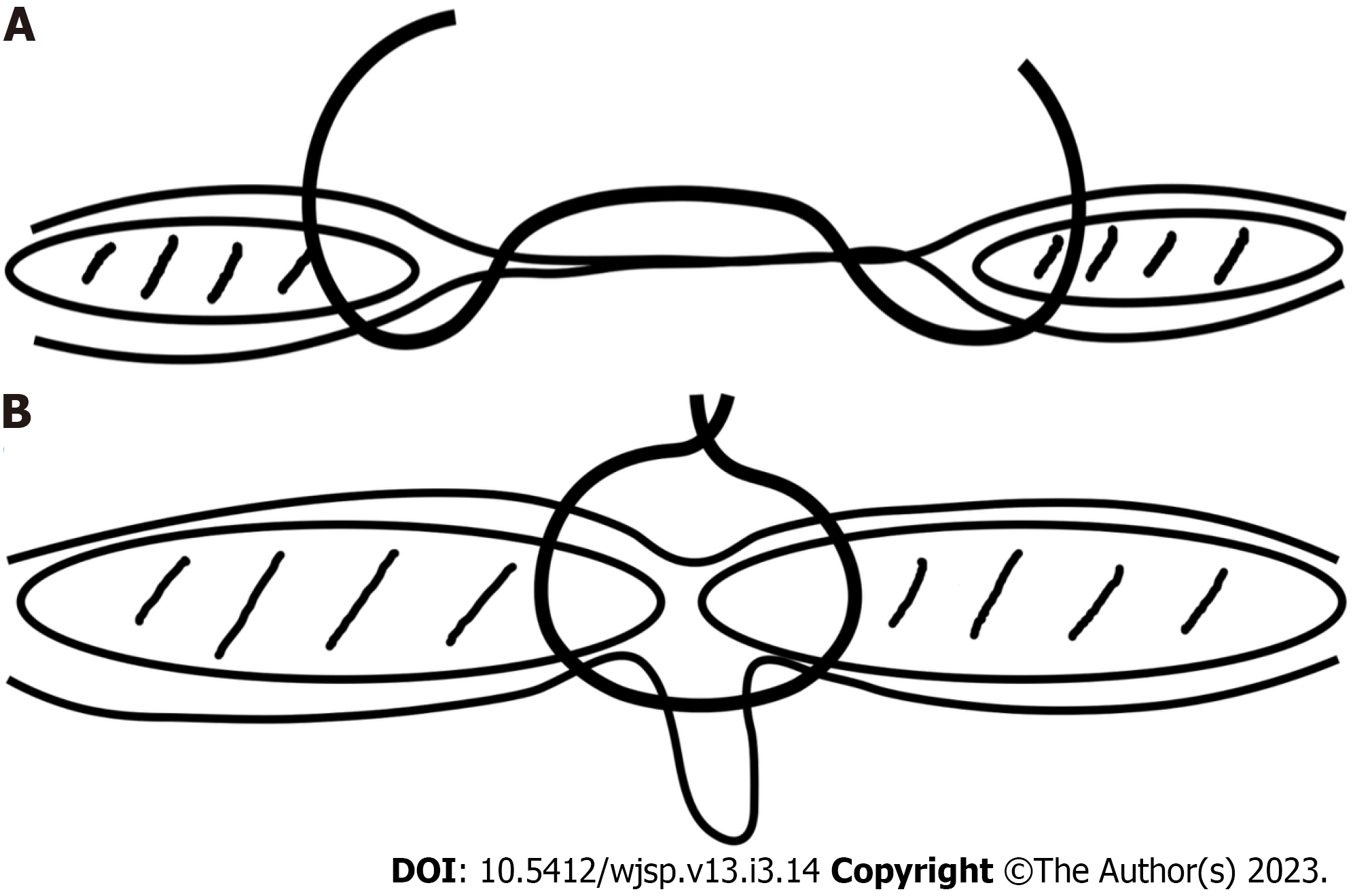
The RMR technique has already been described in detail in a previous publication[9]. The technique focused on bringing the recti together in the midline by full thickness nylon sutures through the anterior sheath, rectus muscle and posterior sheath on one side and continued through the posterior sheath, muscle and anterior sheath of the opposite side (Figure 1A). Thus, when brought together, the hernia sac and attenuated linea alba are inverted ventrally towards the peritoneal cavity (Figure 1B); the sac is not opened unless multiloculated. The inversion resembles the Keel operation but the major difference is that the suture must engage more than 1cm of rectus muscle and its sheaths whereas the Keel engages the 'fibroaponeurotic' tissue around the hernia.
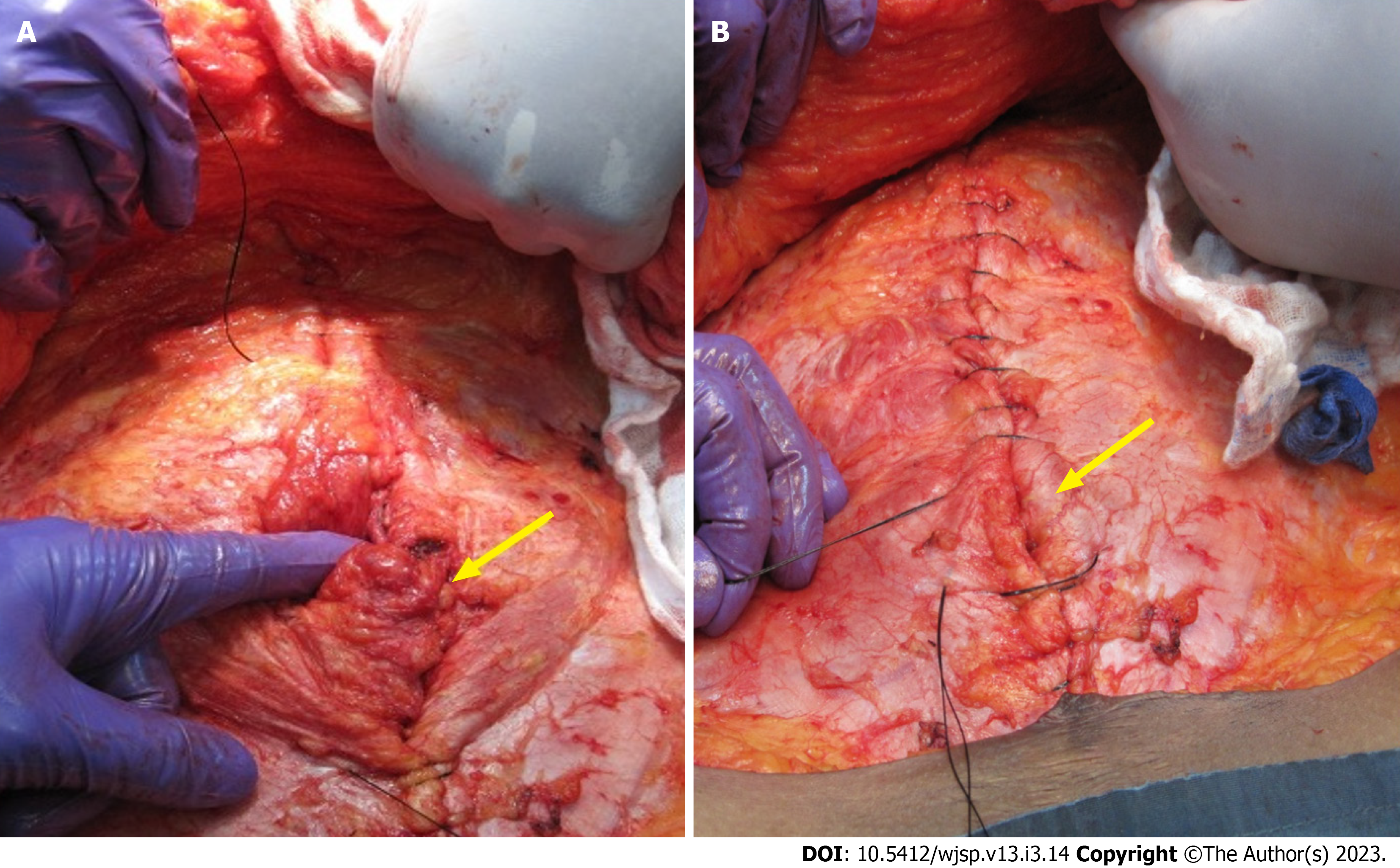
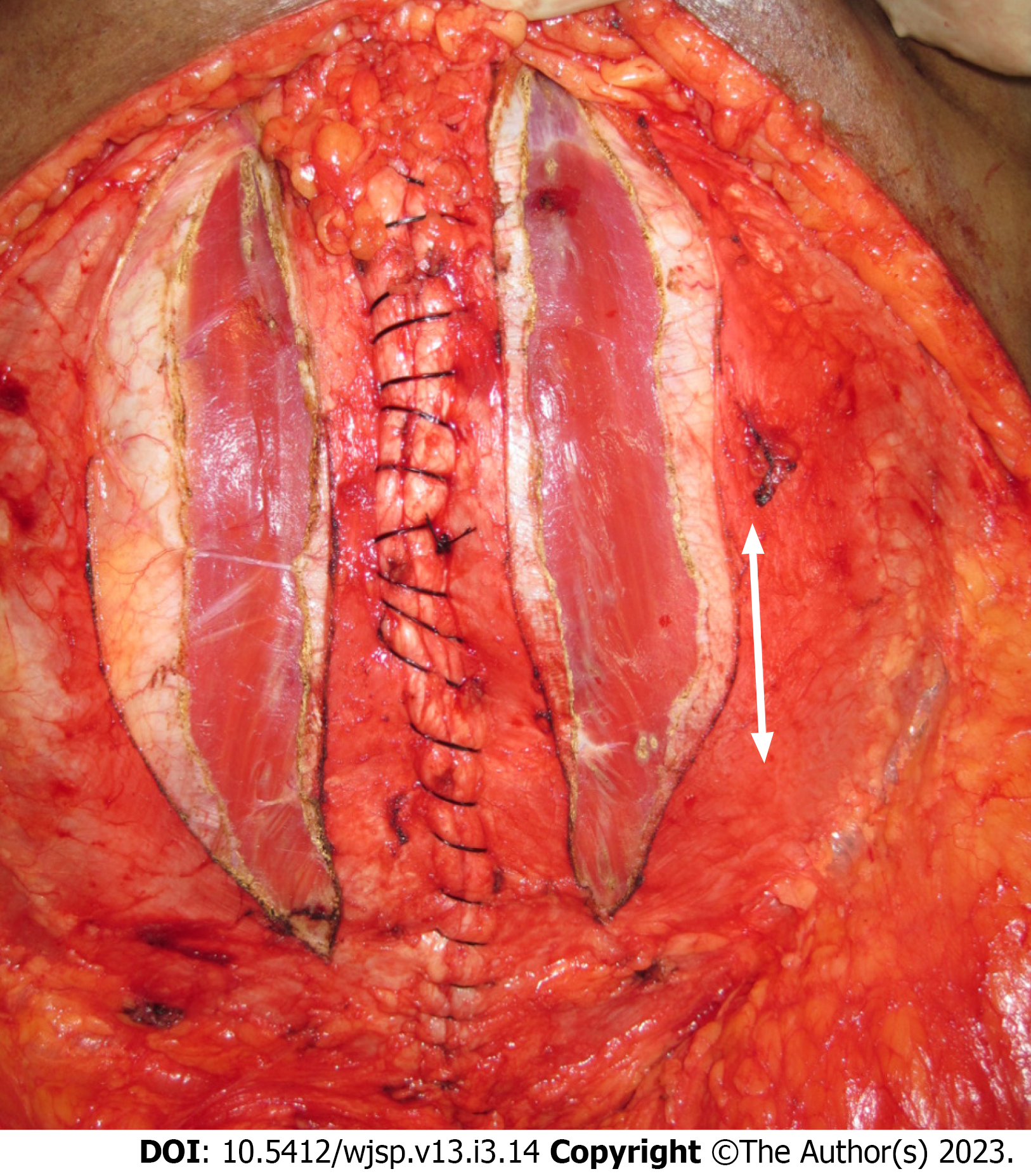
The suture bites engage 1.5-2 cm of rectus sheath and muscle on each side and successive bites are 1.5cm apart. The anterior sheath is dissected to expose 3-4 cm lateral to the medial margin of the rectus muscle; this allows enough space for suturing the muscle as well as incising the anterior sheath, not the muscle (Figure 2). In this center, we used the modified RMR technique previously described[10], where relaxing incisions were made in the anterior rectus sheath (Figure 3) in an attempt to reduce tension on the suture line. The anterior sheath relaxing incision did not extend > 1 cm below the umbilicus because the posterior rectus sheath was deficient below this point. This differs from the Ramirez procedure in that (1) the dissection is not carried far laterally to the lateral border of the rectus muscle; and (2) the relaxing incision is in the anterior rectus sheath, not the external oblique aponeurosis. Haemostasis was achieved and a subcuticular suture was placed to close skin. For large defects, a subcutaneous drain was used. This was strictly an observational study and the attending surgeon was solely responsible for clinical decisions.
Over the 5-year study period, there were 52 patients treated for ventral hernias at this institution. Four patients were excluded due to a desire to have mesh repair (2) and large hernias defects (15 cm and 17 cm) that did not allow primary suture closure (2). The final study sample, therefore, was 48 patients with ventral hernias. These included umbilical hernias (15), para-umbilical hernias (12), supra-umbilical (9) and incisional (12).
There were 48 patients in the final study sample, at a mean age of 56 years (range 28-80). Of this 46 patients had elective repairs and 2 patients with paraumbilical hernias had emergency repairs after presenting with strangulation. The mean maximal diameter of the hernia defect was 7 cm (range 5-12 cm); see distribution in Table 1.
| Hernia type | No. | Mean diameter |
| Umbilical | 15 | 6 cm |
| Paraumbilical | 12 | 7 cm |
| Supraumbilical | 9 | 9 cm |
| Incisional | 12 | 8 cm |
Abdominal drains were used in 30 patients. Eighteen patients had no drains placed, at the decision of the attending surgeon, and 5 of these patients developed clinically significant seromas, requiring aspiration between post-operative days 7-14. There were no seromas in the sub-group in which drains were used. There were no haematomas detected and no other complications were recorded in any patients.
The mean follow up time was 36 mo (range 12-60 mo). There was 1 (2.1%) recurrence diagnosed on clinical examination at the eight post-operative month in a patient who underwent incisional hernia repair. On reoperation, the nylon suture line was intact; the defect had recurred lateral to it, near the umbilicus. The suture had not engaged the muscle and its two sheaths - an error in technique.
Hernia repairs were initially done using sutures to close the defect primarily, but the problem of recurrence eluded surgeons. Theodore Billroth[11] in 1890 first postulated that a prosthesis could be used to close the defect but, at that time, mesh repair was met with high complication rates[11,12]. At that time the quality of material used, the absence of haemostatic devices and paucity of antibiotics would have contributed to the high complication rate. In 1958, Francis Usher published his research on the more inert polypropylene mesh and it was adopted as the gold standard of hernia repair compared to primary suture repair[12,13]. Mesh has become so widely accepted that Pawlak et al[1] reported that it was used in 75% of all hernias repaired in the United Kingdom in the year 2020.
While we agree that the use of mesh in ventral hernia repair generally reduces the rate of recurrence when compared to non-mesh repair [14], we also note that many of the existing non-mesh techniques focus on accurately placing non-absorbable sutures in the linea alba 1cm from the midline[15]. In our opinion, this is not ideal because the linea alba in patients with hernias is often already attenuated and quite wide. We agree with Naraynsingh et al[16] who wrote “it seems logical that a repair which eliminates the linea alba should minimise the risk of recurrence.”
The Rives-Stoppa repair is the main technique when mesh is utilized, but it is a challenging operation[17] and may not always be accurately reproduced. Additionally, there are two issues that deserve further consideration before mesh is used for ventral hernia repair: Mesh complications and mechanism of recurrence.
Mesh infection remains a concern despite aseptic technique and perioperative antibiotic prophylaxis[4,5,18,19]. Peri-operative antibiotics reduce, but do not eliminate, mesh infections. Ríos et al[18] reported that mesh infections reduced from 26.3% to 13.6% when peri-operative antibiotics were administered to patients who underwent mesh repairs of incisional hernias. Apart from the fact that many patients who develop hernias already harbour conditions that predispose to infections, such as obesity, increased age, diabetes and/or a history of smoking[4,20,21], the mere presence of a foreign body reduces the number of bacteria needed to cause an infection by 100000[22,23].
Adhesion formation with bowel involvement can lead to obstruction[24] and abdominal pain[25] in these patients.
The mesh can also lead to irritation and post-operative pain. Chronic post-operative pain, persisting for > 3 mo, occurs in 11%[7] to 17%[27] of patients after ventral hernia repairs. This results in poor function and reduced quality of life in 10%[28] to 26%[28] of patients after undergoing mesh hernia repair, and up to 13% of patients need occasional analgesics up to 4 years after the procedure[28].
The incidence of seromas was reported by Bauer et al[29] to be 5% with polytetrafluoroethylene mesh and Molloy et al[30] reported 4% incidence of seromas and 2% incidence of haematomas with Marlex® mesh. In our study, we did not encounter any haematomas. The incidence of seromas was greater than expected (10.4%), although we noted that these occurred only when drains were omitted. A reasonable further modification could be the routine use of drains as there is no risk of prosthesis infections.
Fistula formation is a relatively rare complication of mesh use, but when it occurs it is a devastating complication[5,6].
In addition to these known complications, the cost of the mesh and the price of treating these complications are yet to be addressed and quantified[2-7]. Given the number of complications associated with mesh repairs, a dedicated legal industry dedicated has developed. In 2011, C.R. Bard was made to pay USD$184 million to settle approximately 3000 cases of mesh failure[8]. This was the largest case of this type but in November 2019, there were over 7000 similar lawsuits pending against Ethicon, Atrium and Bard[31]. There is no established method to quantify the burden of stress to the patients and surgeons dealing with these legalities, but we firmly believe that the money and time spent to settle these lawsuits should be taken into account before a decision is made to use mesh in ventral hernia repairs.
We also suggest that this decision should also include the cost of care to treat mesh complications. Plymale et al[32] identified 34 patients who had ventral hernia repair and subsequent mesh removal. The median cost was approximately double for the removal than for the ventral hernia repair, and the majority of patients developed recurrences.
Midline ventral hernias recur through the linea alba, almost never through the rectus muscles with their anterior and posterior sheaths. It seems logical that the modified RMR which eliminates the linea alba should minimise the risk of recurrence. This study documented that there was a 2.1% recurrence rate after the modified RMR. Additionally, we consider the single recurrence in this series to be due to a technical failure since the recurrence occurred at an area where the sutures did not engage the anterior sheath, rectus muscle and posterior sheath en masse.
Mesh repairs, on the other hand, do not focus on elimination of the defective linea alba. It was not surprising, therefore, that the surgical literature reported greater recurrence rates after mesh repairs, ranging from 2.7%-20%[3,4,7,33,34]. In our opinion this was predictable, considering that recurrence following mesh repair does not occur through the rectus abdominis muscle nor through the mesh itself. Recurrences occur through the linea alba, above, below or beside the mesh.
Although the European Hernia Society and American Hernia Society recommend use of mesh in the umbilical and epigastric hernias more than 1 cm in size[35], many authors have demonstrated the feasibility of successful non-mesh repair in much larger hernias. Ramirez showed that component separation may allow closure of large defects (up to 35 cm) without using prostheses[36]. Using this technique as a modification, Girotto et al[37] were able to achieve a recurrence rate of 6% in 30 patients and Shestak et al[38] reported 5% recurrence rate in 22 patients with 6-14 cm defects after 52 mo follow up. Thus, in spite of the general recommendations, it is possible to achieve acceptable results without using mesh, but none of these emphasize muscular approximation with elimination of the linea alba as we are advocating.
This study has demonstrated that the modified RMR technique carries a lower morbidity risk than the surgical literature reports for mesh ventral hernia repairs[4,7,19,24,27] and avoids the financial and medico-legal ramifications associated with mesh complications[8,31]. With a low morbidity profile and 2.1% recurrence after 36 mo mean follow-up, we suggest that the modified RMR technique should be seriously considered as a viable option for ventral hernia repair.
The modified RMR is an acceptable alternative to mesh repair of ventral hernias. The technique carries a 10.4% seroma rate, but this can be further reduced with routine use of drains. The modified RMR also has the benefit of eliminating all mesh-specific complications.
This study examined the use of a novel procedure to repair ventral hernias without the use of prosthetic mesh. This is a newly described technique.
Mesh utilization for ventral hernia repair may potentially lead to mesh infections, adhesions, seromas, fistula formation and postoperative pain. If the modified Rectus Muscle Repair technique is shown to be effective and safe, then it may lead to the omission of mesh in patients with ventral hernias.
The objective of this study was to examine the short term outcomes of all consecutive patients with ventral abdominal wall hernias > 5 cm in maximal diameter who underwent repair using the modified rectus muscle repair (RMR) technique in a single surgeon unit.
A 5-year prospective study was undertaken to examine the outcome of all consecutive hernia repairs using the modified RMR technique. Patients were reviewed in an outpatient clinic at 3, 6 and 12 mo and evaluated for hernia recurrence on clinical examination. Each patient’s abdominal wall was also assessed with using ultrasonography at 24 mo to detect recurrences. All data were examined with SPSS ver 18.0.
There were 52 patients treated for ventral hernias, and 4 were excluded, leaving 48 in the final study sample, at a mean age of 56 years (range 28-80). The mean maximal diameter of the hernia defect was 7 cm (range 5-12 cm). There were 5 (10.4%) seromas and 1 recurrence (2.1%) at a mean of 36 mo follow-up.
This study proposes that the modified RMR can be used as an acceptable alternative to mesh repair of ventral hernias. The new method that this study suggests is the routine use of drains to reduce seroma rates
Further study of larger case series is warranted since this early research shows encouraging results.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Trinidad and Tobago
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dilek ON, Turkey; Sato M, Japan S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH
| 1. | Pawlak M, Tulloh B, de Beaux A. Current trends in hernia surgery in NHS England. Ann R Coll Surg Engl. 2020;102:25-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 2. | Narkhede R, Shah NM, Dalal PR, Mangukia C, Dholaria S. Postoperative Mesh Infection-Still a Concern in Laparoscopic Era. Indian J Surg. 2015;77:322-326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Luijendijk RW, Hop WC, van den Tol MP, de Lange DC, Braaksma MM, IJzermans JN, Boelhouwer RU, de Vries BC, Salu MK, Wereldsma JC, Bruijninckx CM, Jeekel J. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343:392-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1317] [Cited by in RCA: 1186] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 4. | Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS, Liang MK. Comparison of outcomes of synthetic mesh vs suture repair of elective primary ventral herniorrhaphy: a systematic review and meta-analysis. JAMA Surg. 2014;149:415-421. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in RCA: 142] [Article Influence: 12.9] [Reference Citation Analysis (2)] |
| 5. | Bostanci O, Idiz UO, Yazar M, Mihmanli M. A Rare Complication of Composite Dual Mesh: Migration and Enterocutaneous Fistula Formation. Case Rep Surg. 2015;2015:293659. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Rezende-Neto J, Marshall S, Nixon K, Vlachou P, Rotstein O. Chronic Infection and Enterocutaneous Fistula Secondary to Mesh Migration and Erosion into the Small Bowel. Surgical Infections Case Reports. 2017;2:17-19. [DOI] [Cited in This Article: ] |
| 7. | McLanahan D, King LT, Weems C, Novotney M, Gibson K. Retrorectus prosthetic mesh repair of midline abdominal hernia. Am J Surg. 1997;173:445-449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 141] [Cited by in RCA: 143] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Drugwatch. Hernia Mesh Lawsuits | Mesh Lawsuit |Settlement Amounts & Top Lawyers. Available from: http://www.drugwatch.com/hernia-mesh/Lawsuits. [Cited in This Article: ] |
| 9. | Naraynsingh V, Ariyanayagam D. Rectus repair for midline ventral abdominal wall hernia. Br J Surg. 1993;80:614-615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Naraynsingh V, Hassranah S, Maharaj S, Singh Y, Harnanan D, Islam S, Cawich SO. A Modification of the Rectus Muscle Repair for Repair Ventral Hernias: Case Report. Med Res Arch. 2023;11:1-4. [DOI] [Cited in This Article: ] |
| 11. | Billroth T. The Medical Sciences in the German Universities: A Study in the History of Civilization. New York, NY, USA: Welch, W. H., Ed.; Macmillan; 1924. [Cited in This Article: ] |
| 12. | Baylón K, Rodríguez-Camarillo P, Elías-Zúñiga A, Díaz-Elizondo JA, Gilkerson R, Lozano K. Past, Present and Future of Surgical Meshes: A Review. Membranes (Basel). 2017;7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in RCA: 162] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 13. | Elango S, Perumalsamy S, Ramachandran K, Vadodaria K. Mesh materials and hernia repair. Biomedicine (Taipei). 2017;7:16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Peralta R, Latifi R. Long-term outcomes of abdominal wall reconstruction. what are the real numbers? World J Surg. 2012;36:534-538. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Dudley H. Access to the abdomen and lower chest. 2nd ed. London: Butterworths; 1986. [Cited in This Article: ] |
| 16. | Naraynsingh V, Maharaj R, Dan D, Hariharan S. Strong linea alba: myth or reality? Med Hypotheses. 2012;78:291-292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Heartsill L, Richards ML, Arfai N, Lee A, Bingener-Casey J, Schwesinger WH, Sirinek KR. Open Rives-Stoppa ventral hernia repair made simple and successful but not for everyone. Hernia. 2005;9:162-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Ríos A, Rodríguez JM, Munitiz V, Alcaraz P, Pérez Flores D, Parrilla P. Antibiotic prophylaxis in incisional hernia repair using a prosthesis. Hernia. 2001;5:148-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Database Syst Rev. 2008;2008:CD006438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 20. | Mavros MN, Athanasiou S, Alexiou VG, Mitsikostas PK, Peppas G, Falagas ME. Risk factors for mesh-related infections after hernia repair surgery: a meta-analysis of cohort studies. World J Surg. 2011;35:2389-2398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 21. | Kao AM, Arnold MR, Augenstein VA, Heniford BT. Prevention and Treatment Strategies for Mesh Infection in Abdominal Wall Reconstruction. Plast Reconstr Surg. 2018;142:149S-155S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 22. | Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V. Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res. 2002;63:765-771. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in RCA: 123] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 23. | An YH, Friedman RJ. Concise review of mechanisms of bacterial adhesion to biomaterial surfaces. J Biomed Mater Res. 1998;43:338-348. [DOI] [Cited in This Article: ] |
| 24. | Zinther NB, Fedder J, Friis-Andersen H. Noninvasive detection and mapping of intraabdominal adhesions: a review of the current literature. Surg Endosc. 2010;24:2681-2686. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Mussack T, Fischer T, Ladurner R, Gangkofer A, Bensler S, Hallfeldt KK, Reiser M, Lienemann A. Cine magnetic resonance imaging vs high-resolution ultrasonography for detection of adhesions after laparoscopic and open incisional hernia repair: a matched pair pilot analysis. Surg Endosc. 2005;19:1538-1543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Aubé C, Pessaux P, Tuech JJ, du Plessis R, Becker P, Caron C, Arnaud JP. Detection of peritoneal adhesions using ultrasound examination for the evaluation of an innovative intraperitoneal mesh. Surg Endosc. 2004;18:131-135. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Liang MK, Clapp M, Li LT, Berger RL, Hicks SC, Awad S. Patient Satisfaction, chronic pain, and functional status following laparoscopic ventral hernia repair. World J Surg. 2013;37:530-537. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Paajanen H, Hermunen H. Long-term pain and recurrence after repair of ventral incisional hernias by open mesh: clinical and MRI study. Langenbecks Arch Surg. 2004;389:366-370. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Bauer JJ, Harris MT, Kreel I, Gelernt IM. Twelve-year experience with expanded polytetrafluoroethylene in the repair of abdominal wall defects. Mt Sinai J Med. 1999;66:20-25. [PubMed] [Cited in This Article: ] |
| 30. | Molloy RG, Moran KT, Waldron RP, Brady MP, Kirwan WO. Massive incisional hernia: abdominal wall replacement with Marlex mesh. Br J Surg. 1991;78:242-244. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Drugwatch. Available from: https://www.drugwatch.com/news/2020/10/26/status-of-bard-ethicon-atrium-hernia-mesh-lawsuits/#sources. [Cited in This Article: ] |
| 32. | Plymale MA, Davenport DL, Walsh-Blackmore S, Hess J, Griffiths WS, Plymale MC, Totten CF, Roth JS. Costs and Complications Associated with Infected Mesh for Ventral Hernia Repair. Surg Infect (Larchmt). 2020;21:344-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 33. | Piccoli M, Pecchini F, Vetrone G, Linguerri R, Sarro G, Rivolta U, Elio A, Piccirillo G, Faillace G, Masci E, Guglielminetti D, Santorelli C, Soliani G, Koleva Radica M, Trapani V, Marchi D, Chester J, Leonardi L, Neri S. Predictive factors of recurrence for laparoscopic repair of primary and incisional ventral hernias with single mesh from a multicenter study. Sci Rep. 2022;12:4215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 34. | Kadakia N, Mudgway R, Vo J, Vong V, Seto T, Bortz P, Depew A. Long-Term Outcomes of Ventral Hernia Repair: An 11-Year Follow-Up. Cureus. 2020;12:e9523. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Garcia Urena MA, Simons MP; European and Americas Hernia Societies (EHS and AHS). Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br J Surg. 2020;107:171-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in RCA: 164] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 36. | Ramirez OM, Ruas E, Dellon AL. "Components separation" method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86:519-526. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 974] [Cited by in RCA: 857] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 37. | Girotto JA, Ko MJ, Redett R, Muehlberger T, Talamini M, Chang B. Closure of chronic abdominal wall defects: a long-term evaluation of the components separation method. Ann Plast Surg. 1999;42:385-94; discussion 394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in RCA: 85] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | Shestak KC, Edington HJ, Johnson RR. The separation of anatomic components technique for the reconstruction of massive midline abdominal wall defects: anatomy, surgical technique, applications, and limitations revisited. Plast Reconstr Surg. 2000;105:731-8; quiz 739. [PubMed] [Cited in This Article: ] |