Copyright
©The Author(s) 2015.
World J Respirol. Nov 28, 2015; 5(3): 188-198
Published online Nov 28, 2015. doi: 10.5320/wjr.v5.i3.188
Published online Nov 28, 2015. doi: 10.5320/wjr.v5.i3.188
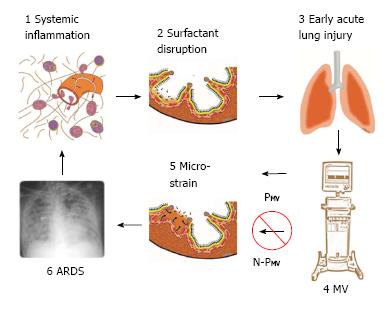
Figure 1 Pathogenesis of acute respiratory distress syndrome.
1: Systemic inflammation, also know as the systemic inflammatory response syndrome (SIRS) activates white blood cells and increases vascular permeability (red arrows); 2: Surfactant disruption occurs if increased permeability result in alveolar edema (tan color) forces surfactant molecules off of the alveolar surface into the lumen of the alveolus; 3: Early acute lung injury (EALI) pathology is associated with moderate surfactant deactivation and pulmonary edema with limited clinical symptoms; 4: Mechanical ventilation (MV) if non-protective (N-PMV) will cause a ventilator induced lung injury, which greatly exacerbates progressive acute lung damage; 5: Micro-strain on the alveolar walls occurs as alveoli with limited surfactant function collapse and reopen during each breath. N-PMV greatly accelerates and expands micro-strain injury and is one of the primary VILI mechanisms. However, if a protective mechanical breath (PMV) is applied immediately upon intubation alveolar micro-strain is avoided; 6: Acute respiratory distress syndrome (ARDS) is caused by a combination of systemic inflammation-induced pulmonary edema, deactivation of surfactant and N-PMV, resulting in alveolar micro-strain. If micro-strain is prevented by applying PMV, VILI will be avoided and ARDS incidence reduced. PMV: Protective mechanical ventilation; VILI: Ventilator induced lung injury.
- Citation: Nieman GF, Gatto LA, Habashi NM. Reducing acute respiratory distress syndrome occurrence using mechanical ventilation. World J Respirol 2015; 5(3): 188-198
- URL: https://www.wjgnet.com/2218-6255/full/v5/i3/188.htm
- DOI: https://dx.doi.org/10.5320/wjr.v5.i3.188