Published online Dec 18, 2016. doi: 10.5312/wjo.v7.i12.801
Peer-review started: July 21, 2016
First decision: September 5, 2016
Revised: September 6, 2016
Accepted: October 5, 2016
Article in press: October 7, 2016
Published online: December 18, 2016
Processing time: 141 Days and 16.3 Hours
To investigate the impact of extrinsic visual feedback and additional cognitive/physical demands on single-limb balance in individuals with ankle instability.
Sixteen subjects with ankle instability participated in the study. Ankle instability was identified using the Cumberland Ankle Instability Tool (CAIT). The subject’s unstable ankle was examined using the Athletic Single Leg Stability Test of the Biodex Balance System with 4 different protocols: (1) default setting with extrinsic visual feedback from the monitor; (2) no extrinsic visual feedback; (3) no extrinsic visual feedback with cognitive demands; and (4) no extrinsic visual feedback with physical demands. For the protocol with added cognitive demands, subjects were asked to continue subtracting 7 from a given number while performing the same test without extrinsic visual feedback. For the protocol with added physical demands, subjects were asked to pass and catch a basketball to and from the examiner while performing the same modified test.
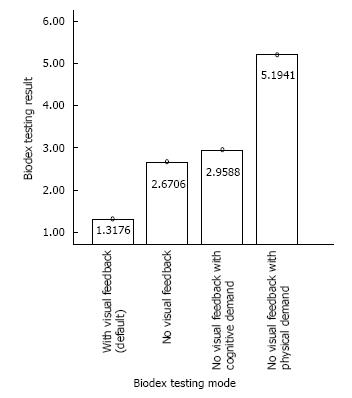
The subject’s single-limb postural control varied significantly among different testing protocols (F = 103; P = 0.000). Subjects’ postural control was the worst with added physical demands and the best with the default condition with extrinsic visual feedback. Pairwise comparison shows subjects performed significantly worse in all modified protocols (P < 0.01 in all comparisons) compared to the default protocol. Results from all 4 protocols are significantly different from each other (P < 0.01) except for the comparison between the “no extrinsic visual feedback” and “no extrinsic visual feedback with cognitive demands” protocols. Comparing conditions without extrinsic visual feedback, adding a cognitive demand did not significantly compromise single-limb balance control but adding a physical demand did. Scores from the default protocol are significantly correlated with the results from all 3 modified protocols: No extrinsic visual feedback (r = 0.782; P = 0.000); no extrinsic visual feedback with cognitive demands (r = 0.569; P = 0.022); no extrinsic visual feedback with physical demands (r = 0.683; P = 0.004). However, the CAIT score is not significantly correlated with the single-limb balance control from any of the 4 protocols: Default with extrinsic visual feedback (r = -0.210; P = 0.434); no extrinsic visual feedback (r = -0.450; P = 0.081); no extrinsic visual feedback with cognitive demands (r = -0.406; P = 0.118); no extrinsic visual feedback with physical demands (r = -0.351; P = 0.182).
Single-limb balance control is worse without extrinsic visual feedback and/or with cognitive/physical demands. The balance test may not be a valid tool to examine ankle instability.
Core tip: Single-limb balance control with the Biodex Balance System (BBS) was significantly worse without extrinsic visual feedback and with cognitive or physical demands in those with ankle instability. Clinicians should consider a patient’s activity and incorporate proper additional demands in ankle stability testing. In addition, the Athletic Single Leg Stability Test of the BBS may not be a valid tool to examine ankle instability. Further research is needed to examine the validity and reliability of the Athletic Single Leg Stability Test in testing ankle instability.
- Citation: Hung YJ, Miller J. Extrinsic visual feedback and additional cognitive/physical demands affect single-limb balance control in individuals with ankle instability. World J Orthop 2016; 7(12): 801-807
- URL: https://www.wjgnet.com/2218-5836/full/v7/i12/801.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i12.801
Ankle sprain is one of the most common musculoskeletal injuries, especially for active individuals and athletes[1-3]. An estimated 23000 ankle sprains occur daily in the United States alone[1]. Ankle sprains often occur as the result of trauma (e.g., landing on an uneven surface from a jump), compromising the physical structural and functional integrity of the tissues surrounding the joint[4]. It was reported that lateral ankle sprains comprise up to 83% of all ankle injuries[5]. They are likely the result of a fast perturbation of ankle plantar flexion and inversion, contributing to complete or partial tears of the 3 lateral ankle ligaments (anterior talo-fibular ligament, calcaneo-fibular ligament, and posterior talo-fibular ligament). Moreover, compromised mechanical restraints (e.g., injured ligaments, joint capsule), muscle strength, and/or neuromuscular control (e.g., proprioception deficits) after the initial injury may further compromise ankle stability[6-18]. As the result, 73% of the individuals who had sprained their ankles before are likely to experience recurrent injuries and ankle instability[19].
Several screening tools [e.g., The Cumberland Ankle Instability Tool (CAIT), The Ankle Instability Instrument, The Functional Ankle Instability Questionnaire] have been developed to identify individuals with ankle instability[18]. A panel of experts concluded that CAIT is based on the highest level (level I) of evidence according to guidelines described by the Centre of Evidence-Based Medicine, Oxford, United Kingdom[18]. The CAIT is a 9-item questionnaire with the score ranges from 30 (best) to 0 (worst)[19]. A subject scores lower than 28 would be considered having ankle instability. It has a test-retest intraclass correlation coefficient (ICC) of 0.96, and it also has a good sensitivity (82.9) and specificity (74.7) in differentiating participants with or without ankle instability[19].
Proper balance control is crucial to ensure safe functional activities. It is achieved with the integration of sensory inputs (e.g., visual, vestibular, and somatosensory information), muscle activations, and cognitive function in human bodies[20]. For individuals with ankle instability, compromised muscle strength and proprioception around the ankle joint may hamper balance control[21,22]. A variety of laboratory equipment (e.g., force plates) and clinical tests (e.g., Y Balance Test, Star Excursion Balance Test, Foot Lift Test) have been developed to examine balance control. One of the commonly used devices to examine both static and dynamic balance control is the Biodex Balance System (BBS; Biodex, Inc, Shirley, NY)[23]. This apparatus has a good test-retest reliability and provides quantitative measures of balance control[24,25]. In addition, the BBS uses a multi-axial testing platform which can be set at various degrees of instability/difficulty (from the static protocol of 0° surface tilt to a dynamic protocol of 20° surface tilt) to challenge the subjects with various fitness levels and injury severities[25]. Compared to other balance testing equipment, the unstable platform of the BBS can simulate unexpected external perturbations (such as landing on an uneven surface) in various activities. However, the monitor of the BBS also provides extrinsic visual feedback (information about the center of gravity location in relation to the base of support) to the subject and compromises the test’s functional significance. In real life scenarios, individuals don’t receive concurrent visual information about their performance. Therefore, balance control measured with the BBS may not truly reflect balance control in daily activities.
Individuals often sprain their ankles while engaging a sport activity (e.g., basketball), in which additional cognitive demands (e.g., whom to pass the ball to) and/or physical demands (e.g., catching or passing the ball) are often present. It was suggested that balance activities take place in association with at least one concurrent task in daily activities, and cognitive function can have an impact on balance control[26]. The impact of adding a cognitive loading on functional activities such as gait and balance control is inconclusive, depending on many factors such as the difficulty of the primary/secondary tasks and subject conditions[26-34]. Examining single-leg balance control with the BBS, Rahnama et al[30] (2010) reported adding a cognitive task decreased postural stability in subjects with ankle instability. However, they used a modified protocol with their subjects’ eyes closed during the testing. Eliminating all visual inputs does not resemble functional activities and common ankle injury mechanisms. Moreover, their protocol can further increase anxiety and unnecessary muscle activation, therefore compromising balance control. In addition, no study had examined the impact of adding a physical demand with a functional significance to individuals performing the single-leg balance lest with the BBS.
The first aim of this study was to investigate the impact of extrinsic visual feedback and additional cognitive/physical demands on single-limb balance in individuals with ankle instability. The second aim of the study was to investigate if any of the 4 single-limb balance testing protocols correlates to ankle stability measured by the CAIT. It was hypothesized that taking away the extrinsic feedback and additional cognitive/physical demands could compromise single-limb balance control. Results of the study can provide clinicians useful information regarding testing and rehabilitation regimens for individuals with ankle instability.
Sixteen subjects (12 females and 4 males, ranged from 19-30 years old) with ankle instability participated in the study. Subjects were recruited from the campus of a local university. The inclusion criteria for the subjects includes: (1) have one or more ankle sprains over the same ankle resulted in pain, swelling, and/or loss of function when it occurred; (2) have the latest ankle sprain occurred within the past year; (3) have no other prior injury that received medical attention for the injured ankle; (4) have no pain or discomfort during single leg standing over the injured ankle at participation; and (5) answer “no” to all questions on the Physical Activity Readiness Questionnaire (PAR-Q and YOU)[35]. All participants signed a consent form approved by the Institutional Review Board of the local university at the beginning of the study.
At the beginning of the testing session, subjects were asked to fill out the CAIT questionnaire (Table 1). Only subjects who scored 27 or less (an indication of ankle instability) were asked to participate in the study. The subject’s unable ankle was examined using the Athletic Single Leg Stability Test of the BBS. The single-leg test was chosen because all subjects were recreational athletes and other double foot support and/or static protocols of the BBS lack functional significance. Subjects were examined with 4 different protocols: (1) default setting with extrinsic visual feedback; (2) no extrinsic visual feedback; (3) no extrinsic visual feedback with cognitive demands; and (4) no extrinsic visual feedback with physical demands (Figure 1). Subjects were tested at dynamic level 4, which provided moderate balance control difficulty.
| Please check the one statement in each question that best describes your ankles | |||
| Left | Right | Score | |
| 1 I have pain in my ankle | |||
| Never | □ | □ | 5 |
| During sport | □ | □ | 4 |
| Running on uneven surfaces | □ | □ | 3 |
| Running on level surfaces | □ | □ | 2 |
| Walking on uneven surfaces | □ | □ | 1 |
| Walking on level surfaces | □ | □ | 0 |
| 2 My ankle feels unstable | |||
| Never | □ | □ | 4 |
| Sometimes during sport (not every time) | □ | □ | 3 |
| Frequently during sport (every time) | □ | □ | 2 |
| Sometimes during daily activity | □ | □ | 1 |
| Frequently during daily activity | □ | □ | 0 |
| 3 When I make SHARP turns, my ankle feels unstable | |||
| Never | □ | □ | 3 |
| Sometimes when running | □ | □ | 2 |
| Often when running | □ | □ | 1 |
| When walking | □ | □ | 0 |
| 4 When going down the stairs, my ankle feels unstable | |||
| Never | □ | □ | 3 |
| If I go fast | □ | □ | 2 |
| Occasionally | □ | □ | 1 |
| Always | □ | □ | 0 |
| 5 My ankle feels unstable when standing on one leg | |||
| Never | □ | □ | 2 |
| On the ball of my foot | □ | □ | 1 |
| With my foot flat | □ | □ | 0 |
| 6 My ankle feels unstable when | |||
| Never | □ | □ | 3 |
| I hop from side to side | □ | □ | 2 |
| I hop on the spot | □ | □ | 1 |
| When I jump | □ | □ | 0 |
| 7 My ankle feels unstable when | |||
| Never | □ | □ | 4 |
| I run on uneven surfaces | □ | □ | 3 |
| I jog on uneven surfaces | □ | □ | 2 |
| I walk on uneven surfaces | □ | □ | 1 |
| I walk on a flat surface | □ | □ | 0 |
| 8 Typically, when I start to roll over (or “twist”) on my ankle, I can stop it | |||
| Immediately | □ | □ | 3 |
| Often | □ | □ | 2 |
| Sometimes | □ | □ | 1 |
| Never | □ | □ | 0 |
| I have never rolled over on my ankle | □ | □ | 3 |
| 9 After a typical incident of my ankle rolling over, my ankle returns to “normal” | |||
| Almost immediately | □ | □ | 3 |
| Less than one day | □ | □ | 2 |
| 1-2 d | □ | □ | 1 |
| More than 2 d | □ | □ | 0 |
| I have never rolled over on my ankle | □ | □ | 3 |
After adopting a single-limb stance on the BSS platform without shoes, subjects performed a total of 3 trails with 20 s/trial while receiving extrinsic visual feedback (their center of gravity location in relation to the base of support) concurrently from the monitor. For the remaining 3 modified protocols, subjects were positioned on the platform facing the opposite direction while keeping the same relative foot position/alignment in relation to the platform as in the default protocol. In the modified protocols, subjects were able to use vision to assist maintaining the balance but without the direct extrinsic visual feedback from the monitor. For the protocol with cognitive demands, subjects were asked to continue subtracting 7 from 121 (trial 1), 119 (trial 2), and 116 (trial 3) to 0 without feedback from the monitor. For the protocol with physical demands, subjects were asked to pass and catch a basketball to and from an examiner standing 6 feet away. The pace was standardized at once every second (guided by a metronome). All 3 modified protocols consisted of 3 trails with 20 s/trial. Subjects were asked to sit and relax for 2 min between protocols to avoid fatigue.
Statistical analyses were conducted using IBM SPSS Statistics (Armonk, NY) Version 21.0. The overall stability index (OSI) produced by the BBS was used for analyses. One-way Analysis of Variance (ANOVA) with repeated measures was used to compare the 4 different testing protocols. Post hoc comparisons were performed with the Paired-Samples T test. Pearson Correlation was used to examine the correlations between the OSI and the CAIT scores. Significance level (P-values) was set at 0.05 for all comparisons.
The subject’s single-limb balance control varied significantly among different protocols (F = 103; P = 0.000). Subjects’ postural control was the worst with added physical demand (passing and catching a basketball) and the best with the default condition with extrinsic visual feedback (Figure 2). Pairwise comparison shows subjects performed significantly worse in all modified protocols (P < 0.01 in all comparisons) compared to the default protocol. Results from all 4 protocols are significantly different from each other (P < 0.01), except for the comparison between the “no extrinsic visual feedback” and “no extrinsic visual feedback with cognitive demands” protocols. Comparing conditions without extrinsic visual feedback, adding a cognitive demand did not significantly compromise single-limb balance control but adding a physical demand did. Scores from the default protocol are significantly correlated with the results from all 3 modified protocols: no extrinsic visual feedback (r = 0.782; P = 0.000); no extrinsic visual feedback with cognitive demands (r = 0.569; P = 0.022); no extrinsic visual feedback with physical demands (r = 0.683; P = 0.004). However, the CAIT score is not significantly correlated with the OSI from any of the 4 protocols: default with extrinsic visual feedback (r = -0.210; P = 0.434); no extrinsic visual feedback (r = -0.450; P = 0.081); no extrinsic visual feedback with cognitive demands (r = -0.406; P = 0.118); no extrinsic visual feedback with physical demands (r = -0.351; P = 0.182).
Compared to the default setting, results of the present study show single-limb balance control was significantly worse without extrinsic visual feedback with the BBS. The BBS is a common testing and training apparatus for balance control. However, the monitor of the BBS provides concurrent extrinsic visual feedback about the performance, which is not available in most activities. In other words, performance with the BBS may over-estimate the true capability of balance control in a functional setting. Although providing additional extrinsic visual feedback could be beneficial during training sessions for those with balance control deficits (e.g., patients with severe Parkinson disease), its result may not accurately reflect the performance in other conditions without additional visual feedback. Moreover, individuals who train exclusively with the BBS may grow accustomed to rely too much on extrinsic visual cues for balance control.
The results show that adding a cognitive demand did not significantly compromise single-limb balance control with the BBS. Literature is very limited about the role of cognitive function on balance control for individuals with ankle instability[30]. The impact of adding a cognitive loading on functional activities depends on many factors such as the difficulty of the primary/secondary tasks and subject conditions[26-34]. Rahnama et al[30] (2010) reported that adding a cognitive task decreased single-limb postural stability in subjects with ankle instability. However, their subjects were asked to close their eyes during the testing. Despite not having extrinsic visual feedbacks, subjects in the current study could still use their vision in a subconscious matter to adjust their body alignment in relation to surrounding objects. Therefore, an easier primary task (maintaining the balance) may explain the lack of cognitive effect in the current study. Another explanation for the difference between the two projects is the difficulty of the secondary task. Instead of performing a simple mathematic calculation task, their subjects were asked to remember the sequence of 7 digits and then repeat the digits in the exact reverse order. The more difficult secondary task could also have a greater impact on single-limb balance control in their study.
No study had examined the impact of adding physical demands on single-limb balance control in individuals with ankle instability. Considering basketball players are more vulnerable to ankle sprains (41.1% prevalence) than other athletes[3], the present study adopted a physical demand (catching and passing) that is similar to playing basketball. The results show that adding a physical demand significantly compromised single-limb balance control with the BBS. In order to catch and pass the basketball properly in a timely fashion, subjects could not solely focus on balance control. Engaging an upper extremity movement/perturbation also moved their center of gravity away from the base of support more often, therefore making it more challenging to maintain single-limb balance. Based on the results, clinicians should incorporate physical demands in ankle stability testing and rehabilitation protocols to better simulate functional activities and sports.
Results of the present study indicate a poor correlation between single-limb balance control and ankle instability severity. It was suggested that ankle instability can have a negative impact balance control[21,22]. Because after the initial ankle sprain, overstretched ligaments and joint capsule may hamper the function of mechanoreceptors (e.g., muscles spindles and Golgi Tendon Organs) and compromise the proprioception of the ankle joint[6-18]. However, other studies found no proprioception difference between unstable and healthy ankles[10,36-38]. Moreover, balance control can also rely on other motor control strategies (e.g., hip strategy), and the coordination of other joints (e.g., hip and knee) and muscles (e.g., trunk muscles). In conclusion, many factors other than ankle stability can contribute to single-limb balance control. The results of the current study suggest that OSI measured with the BBS may not be a good indicator of the severity of ankle instability.
A limitation of the present study is the small sample size. In addition, future studies may consider adding a separate group of subjects without ankle instability to examine if subjects with ankle instability respond to added demands differently from healthy subjects. Although the BBS is a commonly used apparatus in a rehabilitation setting, further research is needed to examine the validity and reliability of the Athletic Single Leg Stability Test in testing ankle instability.
Single-limb balance control is compromised without extrinsic visual feedback and/or with added cognitive/physical demands. Clinicians should consider eliminating excessive extrinsic visual feedback and incorporating physical demands in ankle stability testing and rehabilitation protocols to better simulate functional activities and sports. In addition, many factors other than ankle stability may impact single-limb balance control. Single-limb balance tests with the BBS may not be a valid tool to categorize the severity of ankle instability.
Ankle sprain is one of the most common musculoskeletal injuries. Recurrent ankle sprains can cause ankle instability, and potentially contribute to poor balance control. The purpose of the research was to examine the impact of extrinsic visual feedback and additional cognitive/physical demands on single-limb balance control, and to examine if those testing results can correlate to the severity of ankle instability.
Ankle instability is a well-studied pathology. However, it is still unclear if ankle instability would have a significant impact on single-limb balance control. In addition, some of the commonly used balance testing protocols provide too much visual feedback and lack functional significance.
In order to provide more functional significance of a commonly used protocol for single-limb balance testing, the default protocol was modified to better resemble daily activities and sport movements.
Clinicians should consider eliminating excessive extrinsic visual feedback and incorporating physical demands in ankle stability testing and rehabilitation protocols to better simulate functional activities and sports.
Extrinsic visual feedback in the current study refers to the visual information about the center of gravity location in relation to the base of support displayed by the Biodex Balance System monitor. Proprioception includes both position sense and movement sense of a joint.
Authors aimed to investigate the impact of extrinsic visual feedback and additional cognitive/physical demands on single-limb balance in individuals with ankle instability. Sixteen subjects with ankle instability participated in the study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Jiao C, Zheng N S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305-312. [PubMed] [Cited in This Article: 2] |
| 2. | Farrer C, Franck N, Paillard J, Jeannerod M. The role of proprioception in action recognition. Conscious Cogn. 2003;12:609-619. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279-2284. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 590] [Cited by in RCA: 634] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 4. | Sueki D, Jacklyn B. Orthopedic Rehabilitation Clinical Advisor. 1st ed. USA: Mosby Elsevier 2010; 624-625. [Cited in This Article: 1] |
| 5. | Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73-94. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 183] [Cited by in RCA: 172] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006;43:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Arnold BL, De La Motte S, Linens S, Ross SE. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41:1048-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 177] [Cited by in RCA: 174] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 8. | Fu AS, Hui-Chan CW. Ankle joint proprioception and postural control in basketball players with bilateral ankle sprains. Am J Sports Med. 2005;33:1174-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678-685. [PubMed] [Cited in This Article: 2] |
| 10. | de Noronha M, Refshauge KM, Kilbreath SL, Crosbie J. Loss of proprioception or motor control is not related to functional ankle instability: an observational study. Aust J Physiother. 2007;53:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | McKeon JM, McKeon PO. Evaluation of joint position recognition measurement variables associated with chronic ankle instability: a meta-analysis. J Athl Train. 2012;47:444-456. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 260] [Cited by in RCA: 276] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 13. | de Noronha M, Refshauge KM, Herbert RD, Kilbreath SL, Hertel J. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain? Br J Sports Med. 2006;40:824-828; discussion 828. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 101] [Cited by in RCA: 92] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 14. | Payne KA, Berg K, Latin RW. Ankle injuries and ankle strength, flexibility, and proprioception in college basketball players. J Athl Train. 1997;32:221-225. [PubMed] [Cited in This Article: 2] |
| 15. | Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and Muscle Strength in Subjects With a History of Ankle Sprains and Chronic Instability. J Athl Train. 2002;37:487-493. [PubMed] [Cited in This Article: 2] |
| 16. | Witchalls J, Waddington G, Blanch P, Adams R. Ankle instability effects on joint position sense when stepping across the active movement extent discrimination apparatus. J Athl Train. 2012;47:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Refshauge KM, Kilbreath SL, Raymond J. Deficits in detection of inversion and eversion movements among subjects with recurrent ankle sprains. J Orthop Sports Phys Ther. 2003;33:166-173; discussion 173-176. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Martin RL, Davenport TE, Paulseth S, Wukich DK, Godges JJ. Ankle stability and movement coordination impairments: ankle ligament sprains. J Orthop Sports Phys Ther. 2013;43:A1-40. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 4] [Cited by in Crossref: 109] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 19. | Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland ankle instability tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87:1235-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 371] [Cited by in RCA: 446] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 20. | Emery CA. Is there a clinical standing balance measurement appropriate for use in sports medicine? A review of the literature. J Sci Med Sport. 2003;6:492-504. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833-839. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 186] [Cited by in RCA: 157] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Riemann BL. Is There a Link Between Chronic Ankle Instability and Postural Instability? J Athl Train. 2002;37:386-393. [PubMed] [Cited in This Article: 2] |
| 23. | Cug M, Wikstrom EA. Learning effects associated with the least stable level of the biodex® stability system during dual and single limb stance. J Sports Sci Med. 2014;13:387-392. [PubMed] [Cited in This Article: 1] |
| 24. | Arifin N, Abu Osman NA, Wan Abas WA. Intrarater test-retest reliability of static and dynamic stability indexes measurement using the Biodex Stability System during unilateral stance. J Appl Biomech. 2014;30:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 25. | Jose A Parraca, Pedro R Olivares, Ana Carbonell-Baeza, Virginia A Aparicio, Jose C Adsuar, Narcis Gusi. Test-Retest reliability of Biodex Balance SD on physically active old people. J Human Sports Exercise. 2011;6:444-450. [RCA] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Huxhold O, Li SC, Schmiedek F, Lindenberger U. Dual-tasking postural control: aging and the effects of cognitive demand in conjunction with focus of attention. Brain Res Bull. 2006;69:294-305. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 3] [Cited by in Crossref: 376] [Cited by in RCA: 401] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 27. | O’Shea S, Morris ME, Iansek R. Dual task interference during gait in people with Parkinson disease: effects of motor versus cognitive secondary tasks. Phys Ther. 2002;82:888-897. [PubMed] [Cited in This Article: 2] |
| 28. | Brauer SG, Morris ME. Can people with Parkinson’s disease improve dual tasking when walking? Gait Posture. 2010;31:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 92] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 29. | Broglio SP, Tomporowski PD, Ferrara MS. Balance performance with a cognitive task: a dual-task testing paradigm. Med Sci Sports Exerc. 2005;37:689-695. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Rahnama L, Salavati M, Akhbari B, Mazaheri M. Attentional demands and postural control in athletes with and without functional ankle instability. J Orthop Sports Phys Ther. 2010;40:180-187. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 5] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Lamoth CJ, Stins JF, Pont M, Kerckhoff F, Beek PJ. Effects of attention on the control of locomotion in individuals with chronic low back pain. J Neuroeng Rehabil. 2008;5:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: 2] [Cited by in Crossref: 82] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Laufer Y, Rotem-Lehrer N, Ronen Z, Khayutin G, Rozenberg I. Effect of attention focus on acquisition and retention of postural control following ankle sprain. Arch Phys Med Rehabil. 2007;88:105-108. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Riley MA, Baker AA, Schmit JM. Inverse relation between postural variability and difficulty of a concurrent short-term memory task. Brain Res Bull. 2003;62:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 105] [Cited by in RCA: 104] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 34. | Salavati M, Mazaheri M, Negahban H, Ebrahimi I, Jafari AH, Kazemnejad A, Parnianpour M. Effect of dual-tasking on postural control in subjects with nonspecific low back pain. Spine (Phila Pa 1976). 2009;34:1415-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 2] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 35. | Pescatello LS, American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription Ninth Edition: RC684.E9 A37 2014. Philadelphia PA: Wolters Kluwer/Lippincott Williams & Wilkins Health 2014; 23-24. [Cited in This Article: 1] |
| 36. | Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 175] [Cited by in RCA: 188] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 37. | Gross MT. Effects of recurrent lateral ankle sprains on active and passive judgements of joint position. Phys Ther. 1987;67:1505-1509. [PubMed] [Cited in This Article: 1] |
| 38. | Hiller CE, Nightingale EJ, Lin CW, Coughlan GF, Caulfield B, Delahunt E. Characteristics of people with recurrent ankle sprains: a systematic review with meta-analysis. Br J Sports Med. 2011;45:660-672. [RCA] [PubMed] [DOI] [Full Text] [Cited in This Article: 1] [Cited by in Crossref: 122] [Cited by in RCA: 127] [Article Influence: 9.1] [Reference Citation Analysis (0)] |