Revised: August 22, 2013
Accepted: November 15, 2013
Published online: January 18, 2014
Processing time: 222 Days and 12.6 Hours
Ankle arthrodesis is a common procedure that resolves many conditions of the foot and ankle; however, complications following this procedure are often reported and vary depending on the fixation technique. Various techniques have been described in the attempt to achieve ankle arthrodesis and there is much debate as to the efficiency of each one. This study aims to evaluate the efficiency of anterior plating in ankle arthrodesis using customised and Synthes TomoFix plates. We present the outcomes of 28 ankle arthrodeses between 2005 and 2012, specifically examining rate of union, patient-reported outcomes scores, and complications. All 28 patients achieved radiographic union at an average of 36 wk; the majority of patients (92.86%) at or before 16 wk, the exceptions being two patients with Charcot joints who were noted to have bony union at a three year review. Patient-reported outcomes scores significantly increased (P < 0.05). Complications included two delayed unions as previously mentioned, infection, and extended postoperative pain. With multiple points for fixation and coaxial screw entry points, the contoured customised plate offers added compression and provides a rigid fixation for arthrodesis stabilization.
Core tip: Ankle arthrodesis is a common procedure that resolves many conditions of the foot and ankle; however, complications are common. Complications vary with the technique described and there is not much agreement on the most advantageous method. This study evaluates the efficiency of anterior plating in ankle arthrodesis using customised and Synthes TomoFix plates. We present the outcomes of 28 ankle arthrodeses performed by a single orthopedic surgeon between 2005 and 2012, specifically examining rate of union, patient-reported outcomes scores, and complications. Contoured customised plates offer added compression and provide a rigid fixation for arthrodesis stabilization with few complications.
- Citation: Slater GL, Sayres SC, O’Malley MJ. Anterior ankle arthrodesis. World J Orthop 2014; 5(1): 1-5
- URL: https://www.wjgnet.com/2218-5836/full/v5/i1/1.htm
- DOI: https://dx.doi.org/10.5312/wjo.v5.i1.1
Ankle arthrodesis is commonly used to resolve conditions including end stage arthritis, failure of total ankle arthroplasty, fracture, osteonecrosis, infection, and Charcot joint[1]. Difficulties arise when presented with challenges such as poor bone quality, poor perfusion, gross deformity of the joint, and compromised wound healing. The use of techniques such as intramedullary rodding or external fixation can also be fraught with complications. With an increase in gross deformities of the ankle joint due to diabetes, rheumatoid arthritis, and failed total ankle replacements, surgeons are faced with the need to decrease variables in primary ankle arthrodesis and salvage arthrodesis. This study aims to evaluate the efficiency of customised and Synthes TomoFix plates in 28 ankle fusion patients including time taken to achieve arthrodesis, patient satisfaction, and complications.
Various techniques have been used in the attempt to achieve ankle arthrodesis; however, complications are common. Nonunions are most commonly reported but complications also include tibial stress fractures, malunion, hindfoot arthritis, neurovascular injury, compromised wound healing, and infection[1-4]. The operative techniques often studied can involve difficult and complex procedures in order to achieve acceptable fixation of the arthrodesis. These techniques can be technically demanding for the surgeon and involve lengthy operative time.
With the increase of gross deformity and Charcot joint due to diabetes, challenges arise in salvage arthrodesis. In the failure of total ankle replacement, considerable loss of bone stock is common, as well as the presence of necrotic or non-viable bone. When patients present with poor bone quality, for example after a failed ankle arthroplasty, intramedullary nailing may not be possible due to loss of bone stock in the talus[5]. A study by Moore et al[4] that reviewed intramedullary rodding as a salvage procedure reported a 73.7% fusion rate with 81% of patients being ambulatory. One patient developed a deep infection and another sustained a broken rod. In the current study, two total ankle replacements were revised using an anterior plate; one for aseptic loosening, the second for delayed haematogenous sepsis.
There are many options for ankle arthrodesis, depending on the patient, diagnosis, and surgeon experience. Techniques of internal and external fixation have been reported with varying degrees of success[5-20].
The outcomes of intramedullary rodding, a common alternative to pantalar arthrodesis with plating, have often been reported in the literature. Mendicino et al[15] examined one group of 20 patients who underwent tibiotalocalcaneal arthrodesis with retrograde intramedullary rodding and reported a 95% union rate; however, five diabetic patients sustained major complications following the operation and 11 patients had minor complications. Only one of the patients in the current study is diabetic and this patient did not present with any complications following the operation with anterior plating. Another study done by O’Neill et al[16] which compared locking plates to intramedullary nailing in six fresh frozen cadavers demonstrated that the locking plate provided a significantly higher final stiffness (P = 0.01) and thus offered superior rigidity. Chiodo et al[6] compared intramedullary rodding with the use of a blade-plate and screw in ten matched pairs of fresh frozen cadavers. On one ankle, the intramedullary rod fixed the tibia, talus, and calcaneus. A five-hole plate with a blade was inserted into the contralateral ankle with two or three screws securing the plate to the tibia. The authors found that the blade-plate and screw construct provided more stiffness than the intramedullary rod.
Currently, techniques using plates and screws are known to further increase compression and consequently increase arthrodesis success rates[5,9,14,19]. Plaass et al[5] studied a series of 29 patients in which an anterior double plating system was used to achieve tibiotalar arthrodesis. This method improves compression and fixation and the authors reported that all patients fused at an average of 13.2 wk. Internal compression is known to improve arthrodesis rates and decrease fusion periods. Mears et al[14] studied 17 patients whereby an anterior tension plate was found to realign the ankle and transform the otherwise deforming force of the Achilles tendon into a compressing force. The authors of this study achieved an 82% arthrodesis rate. Rowan et al[19] examined the outcomes of the use of an anterior AO tibial T plate in a retrospective study of 33 patients. In this study, 31 patients (94%) fused and two patients developed tibial stress fractures. The authors of the current study report a 100% union rate.
Arthroscopic ankle arthrodesis is often performed by surgeons as well. An arthroscopic technique allows for the procedure to be minimally invasive, have a shorter recovery period, and have a lower rate of complications[8]. In this procedure, the screws are crossed transversely or medially from the tibia into the talus[8,20]. Fusion rates have been reported to be high, and a short length of time to fusion has often been reported; Ferkel et al[10] reported a union rate of 97% at an average of 12 wk. Removal of screws is common in this procedure and has been reported to range from 9% to 31%[8,10,11]. The surgeon that performed the procedures in the current study has found the anterior plate to be more rigid and that it provides more consistent results; however, ankle arthrodeses are done arthroscopically if the patient has poor skin.
Twenty-eight patients (24 males and 4 females) underwent a unilateral ankle arthrodesis by a single surgeon between 2005 and 2012. Patients ranged in age from 32 to 84 years with a mean age of 61 years. Five of these patients received an anterior customised plate and 23 patients received a modified Synthes proximal-medial tibial plate, based on surgeon preference. Twenty patients were diagnosed preoperatively as having osteoarthritis, three patients had Charcot ankle joints, two had traumatic fractures (one leading to osteoarthritis), one had avascular necrosis leading to ankle collapse, and two patients had a previous ankle replacement (one with aseptic loosening, and one with delayed haematogenous sepsis). Anterior plating was also used in one patient who had a pantalar arthrodesis; the talar screws were continued across into the calcaneus and the subtalar joint was decorticated through a separate lateral incision.
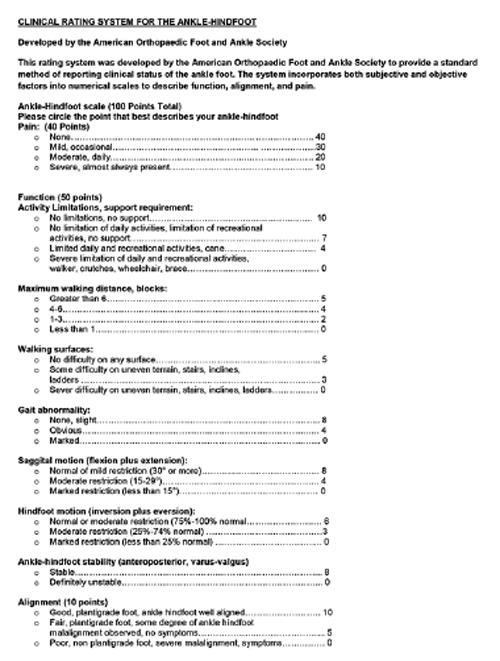
At the initial consultation, prior to any operative measures, patients were given an ankle-hindfoot questionnaire before seeing the surgeon (Figure 1). This questionnaire has been developed by the American Orthopaedic Foot and Ankle Society (AOFAS) as a standardised method of assessing the clinical status of the ankle-hindfoot[21]. The scale incorporates both subjective factors from the patient questionnaire, (e.g., pain and activity limitations), and objective factors from the surgeon questionnaire, (e.g., gait abnormality and alignment). This questionnaire was repeated at the eight week stage and at the patient’s most recent stage in recovery to evaluate hindfoot function.
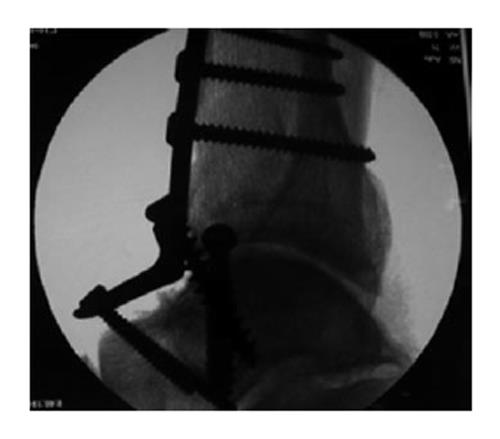
Surgery was carried out under general anaesthesia with the additional use of a knee block, administered by the anaesthetist under ultrasound guidance prior to induction. Prophylactic antibiotic therapy was commenced during the procedure and continued for three doses in all patients. An anterior plate was used in all cases; five cases used a customised plate and 23 cases used a modified Synthes proximal-medial tibial plate. An incision was made longitudinally anterior to the ankle joint. Dissection was then made down to the talotibial joint, using a Hintermann distractor to obtain an optimal level of exposure at the joint surface. Hintermann wires were inserted into the talus and the distal tibia. The distractor was then attached and the joint was distracted. The instrument remained in place during decortication of the joint surface. A 4-mm rose bud burr, curette, bone nibblers, and 1-mm Kirschner wires were used to decorticate the joint surface. A customised plate or Synthes plate was then selected (Figure 2).
Modification of the Synthes plate was achieved by applying pressure to the distal end of the plate using a bending press (65°/180°). The joint was then stabilized using 2-mm Kirschner wires and the positioning of these wires was checked using fluoroscopy before proceeding with plate attachment. The anterior plate was screwed into position beginning with the insertion of the 6.5-mm cancellous home run screw of appropriate length through the distal tibia to the talus or, in the cases of pantalar fusion, to the calcaneus. Through the distal end of the plate, two self-tapping screws were inserted into the talus, continuing plantarly into the distal portion of the calcaneus. At the proximal end of the plate, three self-tapping screws were inserted into the tibia. The use of a home run screw allowed for added compression through the entire joint and further accommodated successful arthrodesis. It is important to note that the usage and placement of screws can vary greatly depending on the condition of the ankle; screening is advised throughout fusion for joint replacement as the target zone may present with narrow bone stock. The wound was then closed using a subcuticular, continuous absorbable suture. A size ten French vacuum drain was also inserted. A compression dressing was applied over the wound and a Plaster of Paris splint, not extending over the wound, was then applied. In the case of the patient who had previously had a total ankle replacement with asepsis, the patient initially had two debridements followed by a gentamicin impregnated cement spacer for eight weeks. To fill the cavity created in the talus by the implant, the distal fibula was harvested through a separate incision and was used as a structured autograft. This technique was also used in the patient with avascular necrosis to maintain hindfoot height.
At two weeks post-operatively, the Plaster of Paris splint and the dressings were removed. X-rays were taken, the wound was checked and redressed, and a fiberglass cast was then applied. In patients who smoke and in patients who have diabetes, rheumatoid arthritis, or a suppressed immune system, a six week course of antibiotic therapy was prescribed. A magnetic implanted bone growth stimulator was used in revision cases and in the Charcot joint cases, as delayed fusion was anticipated. At six weeks postoperatively, patients were seen again for an X-ray. At this time, patients were instructed to partially bear weight in a ski boot orthotic. Patients then returned at 12 wk for X-rays and at 16 wk for X-rays and a computed tomography (CT) scan. Follow-up care after this point depended on fusion and clinical resolution of symptoms. Following this time, X-rays were reviewed at standard intervals ranging from six months consultation to 4.35 years (mean 1.36 years) to ensure that fusion was achieved. CT scans were also performed for all patients at the 12 mo mark to ensure that fusion had occurred.
All patients achieved bony fusion at an average of 36 wk (range 6 wk to 3 years). With the exception of three Charcot joints, all patients fused between 12 and 16 wk (Figure 3A). CT examinations were performed for all patients one year postoperatively. CT scans were also performed at four months postoperatively if the arthrodesis appeared to be healing slowly or if the patient was experiencing pain. On occasion, it was found that the ankle looked fused on X-ray, but clinical symptoms differed and a CT scan confirmed that the fusion was not complete. The three Charcot joints initially developed a fibrous fusion, defined as an asymptomatic stable position for one year; at a three year followup, these ankles were determined to have bony fusion. Partial weight bearing was allowed in all patients at six weeks in a controlled ankle motion walker boot.
Vast improvement was found upon comparison of pre-operative and post-operative ankle-hindfoot scale assessments. The mean ankle-hindfoot AOFAS score increased significantly (P < 0.05) from 28.89 preoperatively (range 3 to 59) to 82.04 at the last review appointment (range 30 to 96). Time frames for the final review appointment varied greatly and depended on individual patient demands (mean 1.36 years, range 14 wk to 4.35 years).
Complications encountered included infection, delayed union, and extended post-operative pain. Four patients developed superficial infections which resolved with a one week treatment of 500 mg oral Keflex four times daily. One patient developed a wound breakdown which resolved quickly after treatment with standard protocol involving debridement, antiseptic lavage, and primary suture in an operative environment. This patient was then treated using intravenous antibiotic therapy and was discharged with a program of six weeks oral antibiotic therapy. One patient’s “Charcot joint” screws began to back out and were reinserted percutaneously at six months postoperatively. Four patients, two of which had Charcot joints, displayed delayed union at 14 wk postoperatively; these patients were given the recommendation to use a magnetic implanted bone growth stimulator. All other patients developed fusion by 36 wk (Figure 3B). Four patients with Synthes plates were recommended for removal of the plate and screws due to residual pain and prominence.
Current studies support the suggestion that internal fixation with plates and screws is superior to intramedullary nailing. Anterior plating provides enhanced compression and rigidity compared to other forms of arthrodesis. The anterior plate is strong enough to secure the ankle even in the case of a delayed union. As patients are always eager to begin weight-bearing, the ability to cease non-weight-bearing at six weeks routinely was beneficial to the current study’s patients.
We found anterior plating to be successful even in the cases of failed total ankle replacements and pantalar arthrodeses. Two total ankle replacements were able to be revised using an anterior plate in this study and one patient underwent a pantalar arthrodesis.
The use of an anterior plate has the added benefit of allowing the calcaneus to be incorporated into the arthrodesis in order to increase rigidity and compression and it also provides a variety of screw entry points. Anterior plating is successful in achieving a high rate of fusion with few complications.
P- Reviewers: Regauer M, SooHoo NF, Trieb K S- Editor: Gou SX L- Editor: A E- Editor: Liu SQ
| 1. | Abidi NA, Gruen GS, Conti SF. Ankle arthrodesis: indications and techniques. J Am Acad Orthop Surg. 2000;8:200-209. [PubMed] [Cited in This Article: ] |
| 2. | Cheng YM, Chen SK, Chen JC, Wu WL, Huang PJ, Chiang HC, Lin CY. Revision of ankle arthrodesis. Foot Ankle Int. 2003;24:321-325. [PubMed] [Cited in This Article: ] |
| 3. | Cooper PS. Complications of ankle and tibiotalocalcaneal arthrodesis. Clin Orthop Relat Res. 2001;33-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Moore TJ, Prince R, Pochatko D, Smith JW, Fleming S. Retrograde intramedullary nailing for ankle arthrodesis. Foot Ankle Int. 1995;16:433-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 115] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Plaass C, Knupp M, Barg A, Hintermann B. Anterior double plating for rigid fixation of isolated tibiotalar arthrodesis. Foot Ankle Int. 2009;30:631-639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Chiodo CP, Acevedo JI, Sammarco VJ, Parks BG, Boucher HR, Myerson MS, Schon LC. Intramedullary rod fixation compared with blade-plate-and-screw fixation for tibiotalocalcaneal arthrodesis: a biomechanical investigation. J Bone Joint Surg Am. 2003;85-A:2425-2428. [PubMed] [Cited in This Article: ] |
| 7. | Christodoulou NA, Mavrogenis AF, Sdenias C, Mitsiokapa EA, Tsaknis R, Salagiannis G, Papagelopoulos PJ. Ankle Arthrodesis Using a Tibio-calcaneal External Fixator. Eur J Orthop Surg Traumatol. 2006;16:146-149. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Cottino U, Collo G, Morino L, Cosentino A, Gallina V, Deregibus M, Tellini A. Arthroscopic ankle arthrodesis: a review. Curr Rev Musculoskelet Med. 2012;5:151-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Easley ME, Montijo HE, Wilson JB, Fitch RD, Nunley JA. Revision tibiotalar arthrodesis. J Bone Joint Surg Am. 2008;90:1212-1223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26:275-280. [PubMed] [Cited in This Article: ] |
| 11. | Gougoulias NE, Agathangelidis FG, Parsons SW. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007;28:695-706. [PubMed] [Cited in This Article: ] |
| 12. | Grass R, Rammelt S, Biewener A, Zwipp H. Arthrodesis of the ankle joint. Clin Podiatr Med Surg. 2004;21:161-178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Kennedy JG, Harty JA, Casey K, Jan W, Quinlan WB. Outcome after single technique ankle arthrodesis in patients with rheumatoid arthritis. Clin Orthop Relat Res. 2003;131-138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Mears DC, Gordon RG, Kann SE, Kann JN. Ankle arthrodesis with an anterior tension plate. Clin Orthop Relat Res. 1991;70-77. [PubMed] [Cited in This Article: ] |
| 15. | Mendicino RW, Catanzariti AR, Saltrick KR, Dombek MF, Tullis BL, Statler TK, Johnson BM. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing. J Foot Ankle Surg. 2004;43:82-86. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 106] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | O’Neill PJ, Logel KJ, Parks BG, Schon LC. Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2008;29:581-586. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Pfahler M, Krodel A, Tritschler A, Zenta S. Role of internal and external fixation in ankle fusion. Arch Orthop Trauma Surg. 1996;115:146-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Rochman R, Jackson Hutson J, Alade O. Tibiocalcaneal arthrodesis using the Ilizarov technique in the presence of bone loss and infection of the talus. Foot Ankle Int. 2008;29:1001-1008. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Rowan R, Davey KJ. Ankle arthrodesis using an anterior AO T plate. J Bone Joint Surg Br. 1999;81:113-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Winson IG, Robinson DE, Allen PE. Arthroscopic ankle arthrodesis. J Bone Joint Surg Br. 2005;87:343-347. [PubMed] [Cited in This Article: ] |
| 21. | Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349-353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3199] [Cited by in F6Publishing: 3040] [Article Influence: 101.3] [Reference Citation Analysis (0)] |