INTRODUCTION
Parathyroid cancer is an uncommon and indolent endocrine malignancy. Clinically, it is characterized by markedly raised serum calcium levels and correlated symptoms (e.g., lethargy, fatigue, mental depression or psychosis, weight loss and muscle weakness), high release of parathyroid hormone (PTH) accompanied by osteolytic bone changes and renal impairment[1-3]. The American Joint Committee on Cancer (AJCC) has neither staged nor planned to stage parathyroid carcinoma in the 7th edition of the AJCC Staging Manual, because of the rarity of the condition[4]. The incidence of parathyroid carcinoma is quite low and is seen with greater frequency in patients with hyperparathyroidism-jaw tumour (HPT-JT) syndrome.
The aetiology of parathyroid carcinoma is unknown and mutations in the HRPT2 gene, a single locus associated with HPT-JT, seem to play a crucial role in its pathogenesis. Inactivation of the tumour suppressor gene, HRPT2, can be identified in a large number of parathyroid carcinomas and therefore, germ-line HRPT2 gene mutations may help in the screening of asymptomatic patients[5]. The most effective treatment for parathyroid carcinoma is complete resection of the primary lesion and any subsequent recurrence of disease[6,7]. Parathyroid cancer tends to recur locally at the operative site and spreads via both lymphatic and haematogenous routes.
Neck ultrasound and 99mTc-sestamibi scintigraphy are the most common imaging studies used to detect benign parathyroid adenoma but are also of value in malignant cases[8]. Ultrasound provides general information about the location of the lesion and its structure[9]; whereas, 99mTc-sestamibi scanning can reveal abnormal and ectopic parathyroid tissue in the neck and elsewhere[10,11]. In cases where malignancy is suspected, higher-resolution anatomical studies are of considerable value[12]. Computed tomography (CT) with medium contrast can provide excellent details on the location of the lesion and its relation to other structures, and may also reveal invasion of surrounding structures and enlarged lymph nodes. On the other hand, magnetic resonance imaging (MRI) with gadolinium and fat suppression can provide the best detail of soft tissues of the neck, and can supplement further information, specifically in the setting of preoperative assessment. MRI is considered superior to CT in assessing recurrent disease, where surgical clips in the field can cause significant artefacts on CT images[13]. Interest in the fusion of single photon emission CT (SPECT) and CT has increased recently, although the use of SPECT/CT has not been reported in parathyroid carcinoma to date. 18F-fluorodeoxyglucose positron emission tomography (FDG PET) has mainly been used in adenoma cases, and very few reports exist on its use in parathyroid carcinoma[14-17]. The aim of this short report is to describe the impact of PET/CT in parathyroid cancer at different phases of the disease.
PET/CT and image analysis
All patients involved in the study underwent whole-body 18F-FDG PET/CT. A dedicated PET/CT scanner (Biograph 16 HR, by Siemens Medical Solutions, Illinois, United States) was used. The PET component is a high-resolution scanner with a spatial resolution of 4.7 mm and has no septa, thus allowing 3-dimensional-only acquisitions. The CT portion of the scanner is the Somatom Sensation 16-slices. Together with the PET system, the CT scanner is used both for attenuation correction of PET data and for localization of 18F-FDG uptake in PET images. All patients were advised to fast for at least 6 h before the integrated PET/CT examination. Each patient’s blood glucose level was obtained prior to tracer injection. The threshold of blood glucose level for FDG injection was below 180 mg/dL. After injection of about 3 MBq of 18F-FDG per kilogram of body weight, the patients rested for a period of about 60 min in a comfortable chair. Emission images ranging from the proximal femur to the base of the skull were acquired for 2-3 min per bed position. Acquired images were reconstructed using the attenuation weighted - ordered subset expectation maximization (OSEM) iterative reconstruction, with 2 iterations and 8 subsets. The Gaussian filter was applied to the image after reconstruction along the axial and transaxial directions. The data were reconstructed over a 128 × 128 matrix with 5.25-mm pixel size and 2-mm slice thickness. Processed images were displayed in coronal, transverse, and sagittal planes. PET/CT images were also assessed quantitatively using the maximum standardized uptake value (SUVmax). All PET/CT scans were performed in our Institutions and two nuclear medicine specialists read all images. At visual analysis, increased FDG uptake on the basis of either highly suspicious or definite CT morphologic changes and not corresponding to physiological uptake patterns was recorded as positive for recurrence/metastases. In contrast, the absence of uptake, out of normal physiological sites, was used to define a negative PET/CT scan. The support of lesions was given by a SUVmax greater than 2.5 in some doubtful lesions.
CASE REPORT
Staging
Patient one: A 55-year-old man presented with back pain and recurrent kidney stones. Laboratory tests showed raised serum calcium and parathyroid hormone (PTH) levels to 3.14 mmol/L (normal, 2.10-2.55 mmol/L)
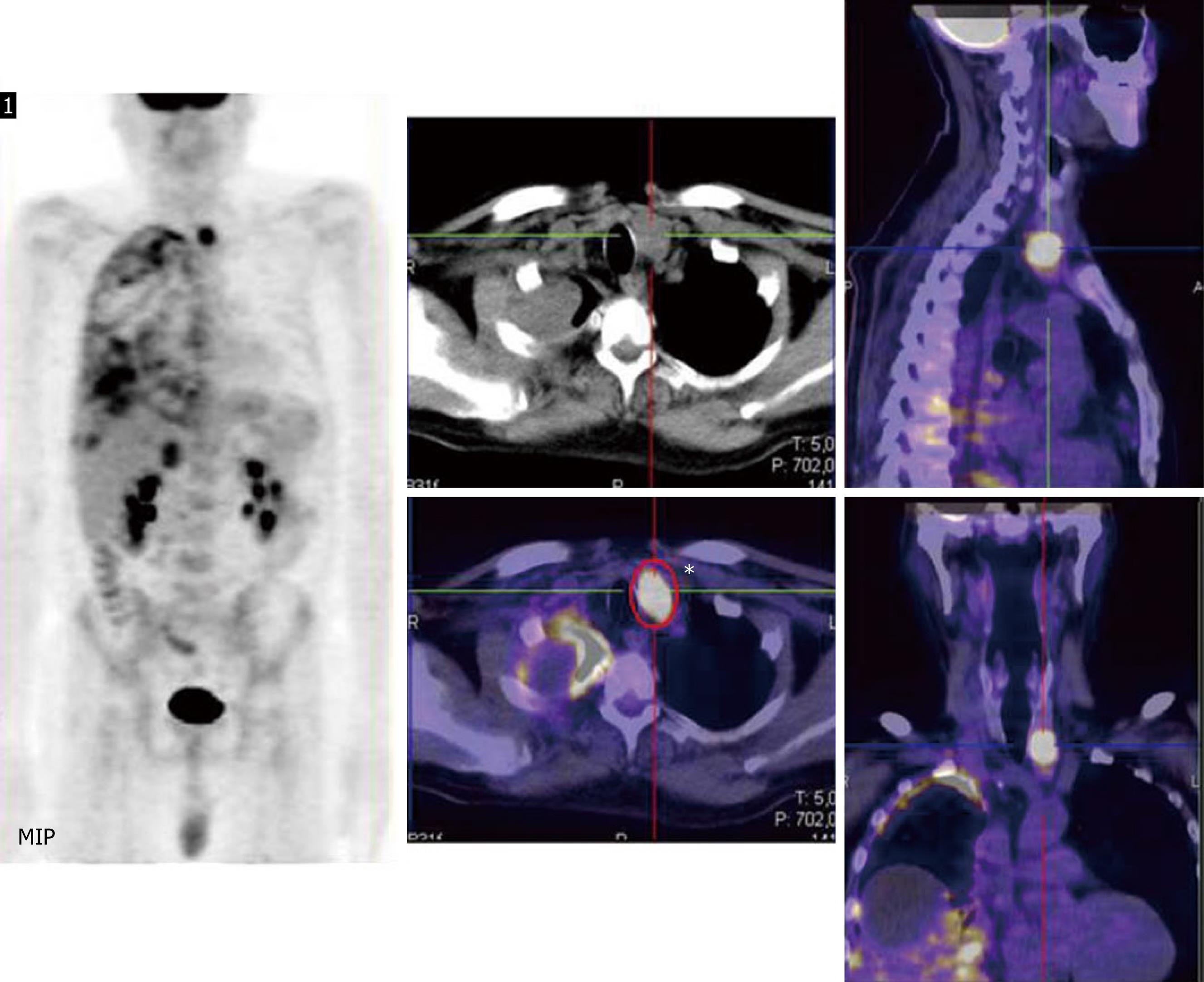
and 730 μg/L (normal, 8-74 μg/L), respectively. Neck ultrasound demonstrated the presence of an abnormal and larger left inferior parathyroid gland. A double-phase SPECT study of the neck and chest, obtained after 15 min and 2 h following intravenous injection of 99mTc-sestamibi, demonstrated no evidence to suggest a parathyroid adenoma. CT scan of the neck, thorax and abdomen demonstrated a lesion in the left inferior parathyroid gland and multiple nodules in the right lung. A confirmatory combined PET/CT scan was performed 60 min after the intravenous injection of 205 MegaBequerel (MBq) FDG. This showed a lesion in the left parathyroid, corresponding to the enhancing nodule seen on the previous CT scan, and right plural metastasis. SUVmax at the main lesion was 10.78 and ranged from 5.00 to 8.74 for the pleural lesions. No other FDG-avid lesions were seen in the rest of the body (Figure 1). The patient underwent left inferior parathyroidectomy with ipsilateral thyroid lobectomy and central compartment lymph node sampling. Histological biopsy of the parathyroid lesion revealed a parathyroid carcinoma (oxyphil cell carcinoma). The genetic analysis for HRPT2 mutation was negative.
Figure 1 Staging.
Right: At Maximum intensity projection the parathyroid and pleural involvements are visible; Central and left: High 18F-Fluorodeoxyglucose-uptake is clearly displayed corresponding to the left parathyroid gland and right pleura in coronal, transverse and sagittal planes.
Restaging
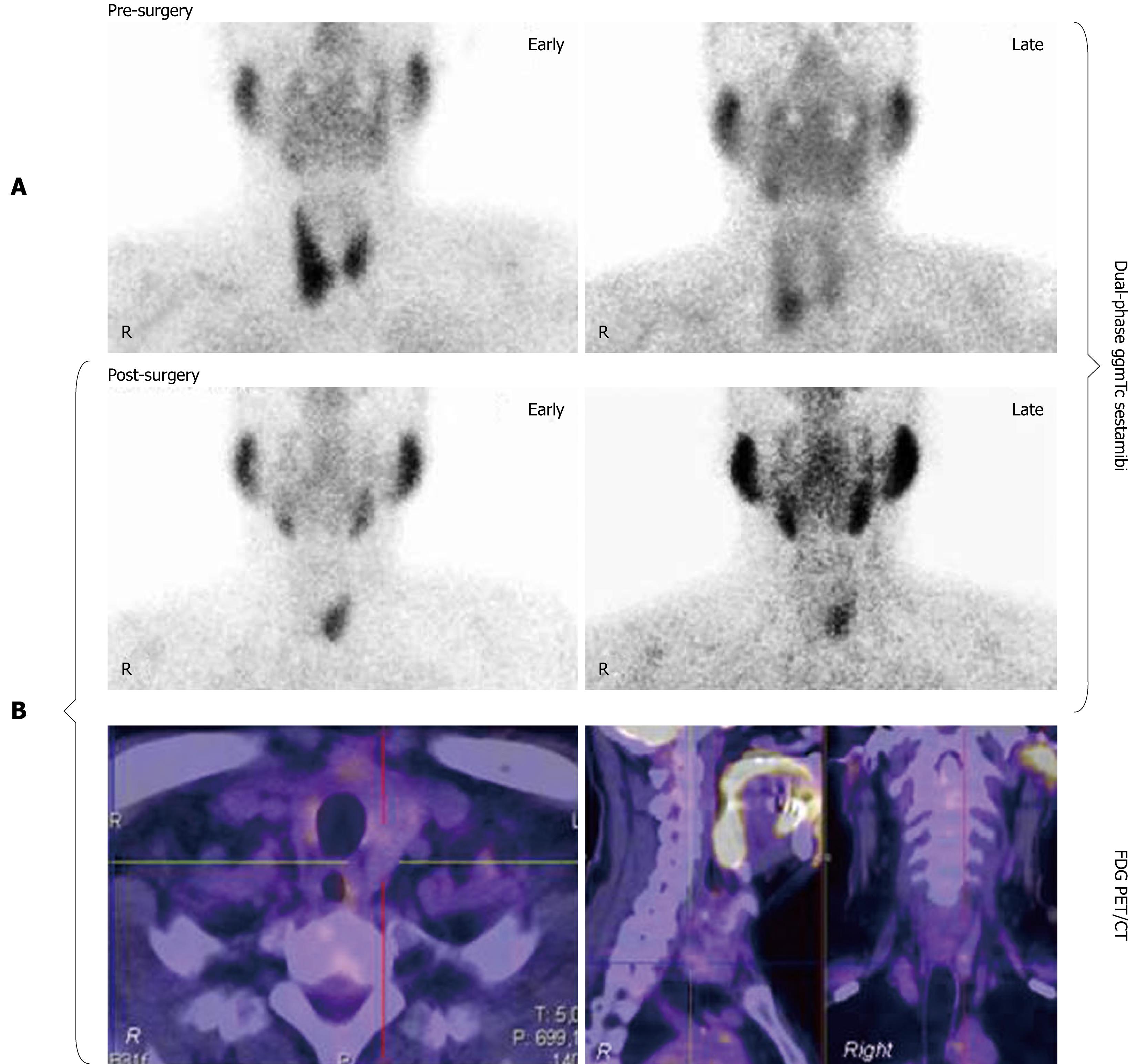
Patient two: A 61-year-old man presented with repeated renal colic and a history of acute pancreatitis. Laboratory tests showed raised serum calcium and PTH levels (3.15 mmol/L and 899 μg/L, respectively). A 99mTc-sestamibi parathyroid scan reported a positive increase in tracer in the right inferior parathyroid glands between early and delayed images (Figure 2A). He underwent right thyroid lobectomy associated with right parathyroidectomy due to intraoperative evidence of a large lesion (mean diameter 4 cm) that infiltrated adjacent structures. The histological analysis revealed a right parathyroid carcinoma that infiltrated the nearest organs (thyroid gland and omolateral recurrent nerve). Three months after surgery, laboratory tests showed a reduction in calcium (2.08 mmol/L) and PTH levels, although higher than the normal value (94 μg/L). A second 99mTc-sestamibi scan was performed demonstrating moderate tracer uptake in the left contralateral parathyroid gland both in early and late scans; for the exclusion of persistent contralateral parathyroid disease, a combined PET/CT scan was performed using 204 MBq of FDG revealing no uptake in the neck region (Figure 2B).
Figure 2 Restaging.
A: Pre-surgical 99mTc99 sestamibi early (15 min) and delayed (2 h) images showed the presence of high uptake in the right inferior parathyroid gland; B: Post-surgical scintigraphy scan demonstrated high tracer uptake in the left inferior parathyroid gland at early and late images, whereas no 18F-Fluorodeoxyglucose-uptake in the same gland during the positron emission tomography/computed tomography scan was reported.
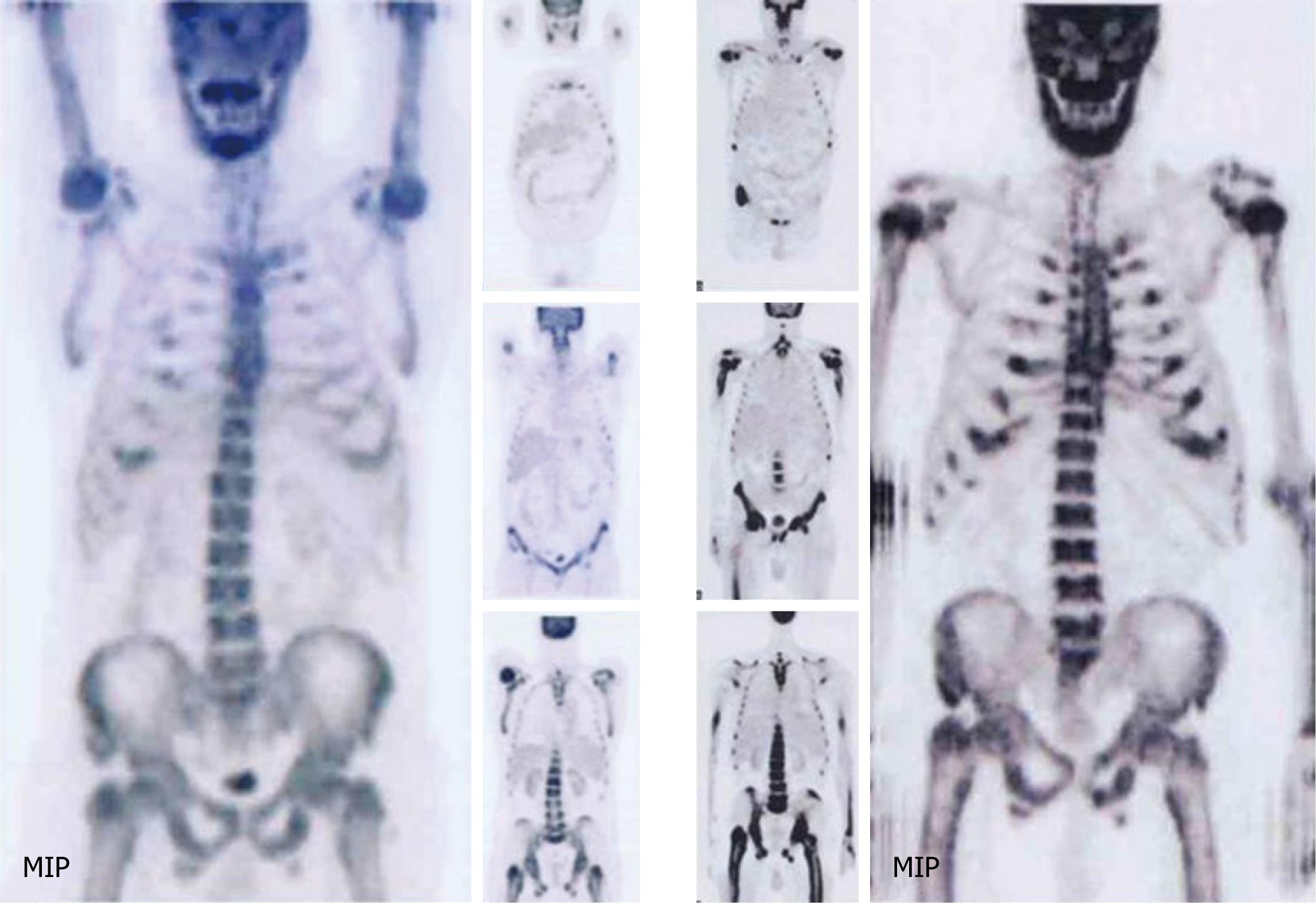
Patient three: A 54-year-old man with history of parathyroid carcinoma which was treated with surgery, radiotherapy and chemotherapy. Pre-surgery laboratory tests showed a PTH level of 1410 μg/L. Inactivation of the tumour suppressor gene HRPT2 was demonstrated. Three years after initial diagnosis, the patient developed disease relapse at the left lung and adjacent ribs (PTH levels and serum calcium were 1268 μg /L and 3.05 mmol/L, respectively) for which he underwent left inferior lung lobectomy and rib resections. The histological analysis showed parathyroid cancer metastasis in the lung and brown tumours in the ribs. During the follow-up period, two FDG PET/CT scans were performed to evaluate the extension and status of disease. These scans demonstrated widespread bone marrow-based lesions with high FDG uptake that had increased further at a follow up scan (Figure 3).
Figure 3 Progression of disease.
Right: First positron emission tomography/computed tomography (PET/CT) exam demonstrated moderate and diffuse skeletal involvement, particularly in medullar bone; Left: Second PET/CT scan, performed 5 mo after earlier PET exam, showed progression of skeletal disease.
Post-surgery evaluation
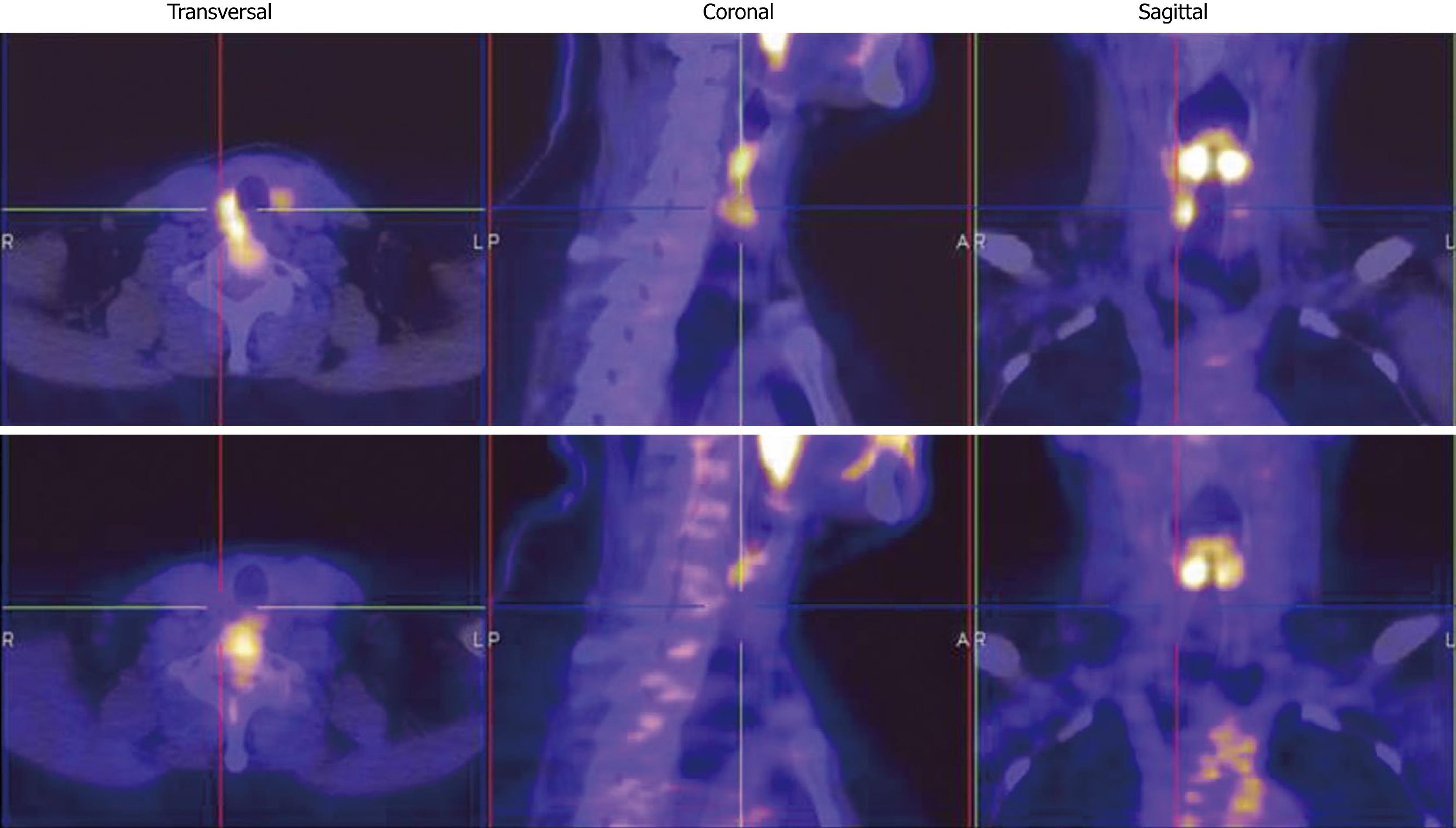
Patients four and five: Two patients (a female aged 48 years and a male aged 64 years) complained of anxiety and agitation. Serum calcium and PTH levels were raised (2.87 mmol/L and 500 μg/L for the first patient, 2.19 mmol/L and 360 μg/L for the second patient). The first patient underwent total thyroidectomy with right parathyroidectomy, the second had left thyroid lobectomy to excise a large infiltrative parathyroid lesion. A parathyroid cancer was demonstrated at histological analysis in both cases associated with a micro-papillary thyroid cancer in the second patient. To evaluate the absence of residual disease, a whole-body 18F-FDG PET/CT was performed approximately 50 d after surgery. The scan demonstrated mild FDG-uptake in the parathyroid lodge corresponding to the surgical site, doubtful for persistence of disease. Both patients underwent 99mTc-sestamibi scintigraphy within 1 wk which was negative for parathyroid tissue. Finally, to resolve any doubt, new PET/CT exams were performed after 3 mo which showed no uptake in the locations previously described (Figure 4).
Figure 4 Post-surgical evaluation.
Up: First positron emission tomography/computed tomography (PET/CT) scan performed at least 50 d after curative surgery, demonstrated mild 18F-Fluorodeoxyglucose (FDG) uptake corresponding to the right lateral wall of the larynx; Down: Second PET/CT exam, performed 4 mo after curative surgery, demonstrated the disappearance of FDG-uptake at the same site.
DISCUSSION
Parathyroid carcinoma is a very rare cause of PTH-dependent hypercalcaemia, accounting for less than 1% of all cases of hyperparathyroidism[18]. The diagnosis of parathyroid carcinoma is often made during surgery or histopathology examination. The tumour often invades surrounding structures, spreads to regional lymph nodes and disseminates haematogenously to lungs, liver and bones. The prognosis is affected by the completeness of tumour resection. Mortality rates for parathyroid carcinomas, particularly for those patients with recurrence within the first 2 years postoperatively, are high and are reported to be between 46% and 65%[12-21].
Staging
18F-FDG PET is recognized as a powerful tool to detect tumours, especially malignant cancers (i.e. lymphoma, breast cancer, lung cancer, etc.) due to an increased glucose metabolism that is correlated with a larger number of glucose transporter proteins[22].
The hybrid PET/CT technique offers many advantages over conventional imaging modalities in the evaluation of disease extension due to dual anatomical and functional information allowing small tumour deposits in liver, lungs, bone, adrenal glands, soft tissues, thyroid or skin to be detected and localized in a single examination. Micrometastases, however, cannot be detected and small lung metastases (less than 6 mm) can be missed by PET when performed as a separate imaging test. Moreover, qualitative evaluation of glucose metabolism can also be quantified using SUV which is a semi-quantitative parameter of malignancy. Certain factors such as tumour aggressiveness or metabolic activity are important prognostic indicators of malignant tumours besides the stage at initial diagnosis, and could play an additional role in risk stratification and assessment of prognosis. A variety of studies have linked the intensity of 18F-FDG, and therefore glucose metabolism of primary tumours, to progression-free and overall survival[23].
We present the first report on the value of PET/CT in parathyroid malignancy at different phases of the disease. Neumann et al[24] reported a clinical case of parathyroid cancer that was not detected by double-phase 99mTc-sestamibi scintigraphy and MRI, but localized by FDG-PET. They concluded that FDG-PET provided additional information related to the location and extent of parathyroid carcinoma, compared to CT, MRI and 99mTc-sestamibi. In our experience (1st patient), the impact of PET/CT in staging was mainly addressed to evaluate the loco-regional and distant spread of disease, adding data on lesion metabolism. According to our results, parathyroid carcinoma and its metastatic sites showed significant avidity for FDG, with a SUVmax value of 10.78 in the primary lesion. It is difficult to postulate a statistical correlation between the histologic grade of the tumour and the level of FDG uptake, due to the limited number of parathyroid carcinoma cases studied with FDG PET reported in literature [25], thus neither sensitivity nor specificity of the technique can be calculated. From our experience, the elevated SUV value highlights the aggressiveness of the tumour and therefore its poor prognosis.
Restaging
Early detection of recurrent disease in parathyroid cancer, as in other tumours, is mandatory for the effectiveness and early initiation of appropriate therapy. Ultrasound, CT and MRI scans are employed as routine imaging procedures, but they have marked limitations in the pre- and post-operative detection of tumour spread and early detection of recurrent disease[26]. Some previously published reports have suggested the superiority of nuclear medicine scans to cross-sectional imaging methods (CT and MRI) in the detection of recurrent parathyroid carcinoma, defining the inclusion of FDG PET in the diagnostic algorithm. Al-Sobhi et al[27] described a patient with an established diagnosis of parathyroid cancer for which he had undergone surgery. 99mTc-sestamibi, performed more than 3 years after surgery due to an increase in PTH localized the recurrence of disease and identified a local metastasis. Arslan et al[16] described a 43-year-old man who had undergone left parathyroidectomy and hemithyroidectomy for parathyroid carcinoma; 2 years after surgery the patient had a recurrence of disease and underwent complete thyroidectomy and left neck dissection. One year later, the patient showed an increase in serum PTH and calcium levels. Neither CT nor MRI was helpful in revealing recurrence or residual malignancy. FDG-PET showed a solitary focus of moderately increased FDG-uptake (SUVmax: 2.1) in the anterior mediastinum at the level of the sternal notch, compatible with parathyroid carcinoma recurrence. Gardner et al[17] described a 47-year-old man with parathyroid carcinoma treated surgically who had raised calcium and PTH 18 years later. Thoracic CT demonstrated a small nodule in the right lung of unknown significance, not amenable to percutaneous biopsy. FDG PET/CT was performed which demonstrated a focus of activity in the lung nodule with a SUVmax of 3.2.
Histological exam can demonstrate metastatic parathyroid carcinoma. According to our results, PET/CT was able to recognize skeletal lesions with bone-marrow involvement (3rd patient), thus demonstrating better diagnostic accuracy compared to conventional imaging. This conforms to the clear evidence in the literature that PET/CT is able to identify bone marrow disease early in the initial phases compared with conventional imaging such as CT[28].
Furthermore, PET/CT was able to exclude the recurrence of disease (2nd patient); it identified normal function of the parathyroid gland rather than hyperparathyroidism status/suspicious for recurrence otherwise shown on 99mTc-sestamibi scan. This finding shows that a PET exam can demonstrate the absence of relapse or hyperfunction of the contralateral parathyroid (or secondary hyperparathyroidism) in patients with a history of parathyroid cancer.
Post-surgery evaluation
Tissues with increased glucose metabolism, such as malignant lesions, appear as areas of increased activity on PET scans due to trapped FDG within the cells. However, one of the limitations of FDG PET is the false positive results which arise due to inflammation[29,30]. Acute or chronic inflammation, abscesses, inflammatory lymphadenopathy and non-specific reactions following radiotherapy may mimic tumour tissue on PET scans[31]. After surgery or radiation, post-treatment inflammation or infection can also show up on PET scan and make it difficult to differentiate residual cancer, especially if close to the original treated tumour. Because of this concern, it is generally recommended that PET should be performed at least 3-6 mo after treatment, thus reducing the rate of false positive results; therefore, any areas that appear suspicious on PET should be confirmed as recurrence or residual cancer with other imaging modalities and/or biopsy before planning any interventions. In our experience in parathyroid cancer (4th and 5th patients), a delay of at least three or four mo from surgery to PET/CT, allowed for differentiation between residual cancer and inflammatory processes, whereas a period of only 1 mo does not seem to be enough and may increase the post-surgical false positive rate at FDG PET/CT.
In conclusion, PET/CT scan can be considered a very sensitive tool in all phases of parathyroid cancer. As in other tumours, the main roles of metabolic imaging are: (1) extension of disease at initial staging; (2) identification of suspected tumour recurrence; and (3) evaluation of residual disease after primary treatment. PET/CT could be considered a complementary technique, in addition to conventional imaging, although the loss of sensitivity and specificity in some conditions (i.e. small lesions), makes its use in early staging rather difficult.