Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastrointest Pathophysiol. May 15, 2014; 5(2): 82-90
Published online May 15, 2014. doi: 10.4291/wjgp.v5.i2.82
Published online May 15, 2014. doi: 10.4291/wjgp.v5.i2.82
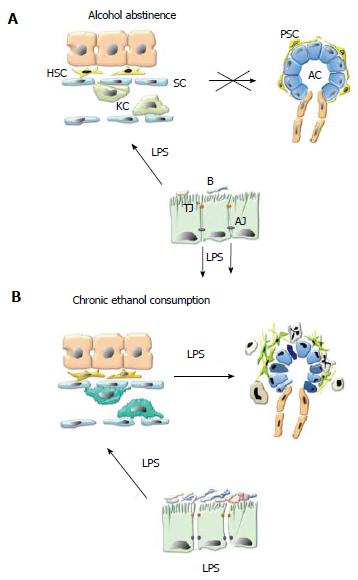
Figure 1 Alcohol and lipopolysaccharide promote pancreatic necroinflammation and fibrosis via pancreatic stellate cell activation.
A: Alcohol abstinence. In healthy, non-alcoholic subjects small amounts of lipopolysaccharide (LPS) derived from the membrane of commensal gram negative bacteria (B) cross the gut epithelial barrier at the level of interendothelial junctions. LPS reaches the liver via the portal circulation where it is entirely cleared by Kupffer cells (KC) in the liver sinusoids (S), preventing it from entering the systemic circulation and reaching systemic organs such as the pancreas; B: Chronic ethanol consumption. Chronic alcohol consumption promotes bacterial proliferation in the proximal small bowel, dissociation of interendothelial junctions (by direct toxicity of alcohol and its metabolites) and leads to increased translocation of LPS into the portal circulation. In the liver, alcohol decreases the phagocytic capacity of Kupffer cells. As a result, LPS enters the systemic circulation and exerts its harmful effects on the pancreas. Alcohol and LPS promote pancreatic necroinflammation and fibrosis via PSC activation. TJ: Tight junctions; AJ: Adherens junctions; AC: Acinar cell; PSC: Pancreatic stellate cell.
- Citation: Vonlaufen A, Spahr L, Apte MV, Frossard JL. Alcoholic pancreatitis: A tale of spirits and bacteria. World J Gastrointest Pathophysiol 2014; 5(2): 82-90
- URL: https://www.wjgnet.com/2150-5330/full/v5/i2/82.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v5.i2.82