Copyright
©2013 Baishideng Publishing Group Co.
World J Gastrointest Pathophysiol. Feb 15, 2013; 4(1): 1-11
Published online Feb 15, 2013. doi: 10.4291/wjgp.v4.i1.1
Published online Feb 15, 2013. doi: 10.4291/wjgp.v4.i1.1
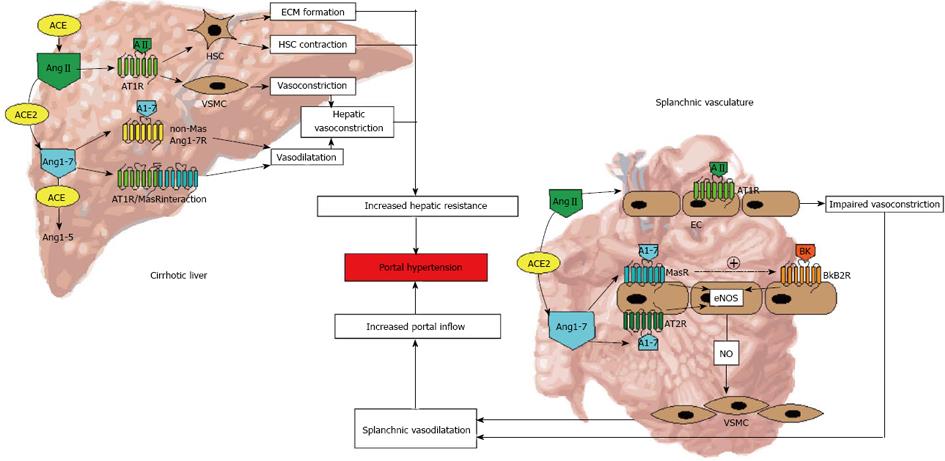
Figure 4 Overview of the renin angiotensin system-mediated pathophysiological changes in portal hypertension.
In cirrhosis, the effects of classical axis of the renin angiotensin system (RAS), mediated by its potent vasoconstrictor peptide angiotensin II (Ang II), are predominant within the hepatic vasculature, resulting in increased hepatic resistance to portal inflow. In this, apart from fixed barrier due to increased deposition of extracellular matrix (ECM) proteins, vascular tone is exacerbated by Ang II action on myofibroblastic cells (activated hepatic stellate cells-HSCs) and vascular smooth muscle cells (VSMCs). In contrast, the effects of the alternate axis of the RAS, mediated by its vasodilator peptide angiotensin-(1-7) (Ang1-7), are predominant within the splanchnic vasculature, resulting in increased nitric oxide (NO) production by vascular endothelial cells (ECs). This consequently exacerbates portal hypertension as a result of increased inflow to the portal circulation. Ang1-5: Angiotensin-(1-5); ACE: Angiotensin converting enzyme; ACE2: Angiotensin converting enzyme 2; eNOS: Endothelial nitric oxide synthase; Bk: Bradykinin; BkB2R: Bradykinin B2 receptor; AT1R: Angiotensin II type 1 receptor; AT2R: Angiotensin II type 2 receptor; MasR: Mas receptor.
- Citation: Herath CB, Grace JA, Angus PW. Therapeutic potential of targeting the renin angiotensin system in portal hypertension. World J Gastrointest Pathophysiol 2013; 4(1): 1-11
- URL: https://www.wjgnet.com/2150-5330/full/v4/i1/1.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v4.i1.1