Published online Jun 24, 2024. doi: 10.4291/wjgp.v15.i3.93408
Revised: May 13, 2024
Accepted: June 3, 2024
Published online: June 24, 2024
Processing time: 113 Days and 16.6 Hours
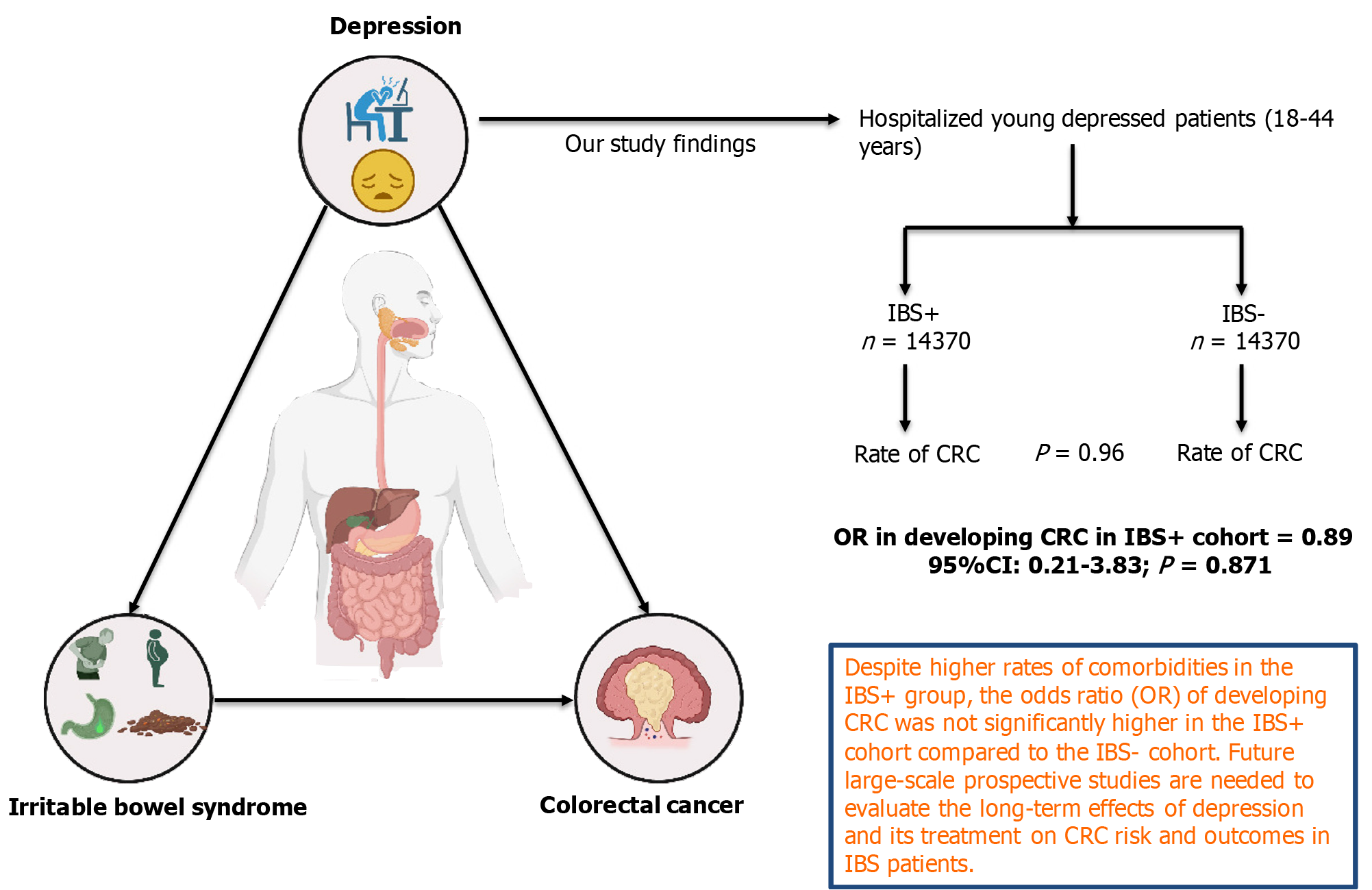
There exists a link between irritable bowel syndrome (IBS) and depression. Similarly, chronic depression is known to increase the risk of cancer in general. In this population-based analysis, we investigated the prevalence and the odds of colorectal cancer (CRC) in young-depressed patients with IBS.
To investigate the relationship between IBS and CRC in young, depressed patients using a nationally representative United States inpatient sample.
The 2019 National Inpatient Sample was used to identify young (18-44 years) patients admitted with comorbid depression in the presence vs absence of IBS using relevant International Classification of Diseases, Tenth Revision, Clinical Modification codes. Primary endpoint was the prevalence and odds of CRC in age matched (1:1) young-depressed cohort hospitalized with IBS (IBS+) vs without IBS (IBS-). Multivariable regression analysis was performed adjusting for potential confounders.
Age-matched (1:1) young-depressed IBS+ (83.9% females, median age 36 years) and IBS- (65.8% females, median age 36 years) cohorts consisted of 14370 patients in each group. IBS+ cohort had higher rates of hypertension, uncomplicated diabetes, hyperlipidemia, obesity, peripheral vascular disease, chronic obstructive pulmonary disease, hypothyroidism, prior stroke, prior venous thromboembolism, anxiety, bipolar disorder, and borderline personality disorder (P < 0.005) vs the IBS- cohort. However, prior myocardial infarction, acquired immunodeficiency syndrome, dementia, smoking, alcohol abuse, and drug abuse (P < 0.005) are high in IBS- cohort. The rate of CRC was comparable in both cohorts [IBS+ n = 25 (0.17%) vs IBS- n = 35 (0.24%)]. Compared to the IBS- cohort, the odds ratio (OR) of developing CRC was not significantly higher [OR 0.71, 95% confidence interval (CI) 0.23-2.25)] in IBS+ cohort. Also, adjusting for baseline sociodemographic and hospital characteristics and relevant comor
This nationwide propensity-matched analysis revealed comparable prevalence and risk of CRC in young-depressed patients with vs without IBS. Future large-scale prospective studies are needed to evaluate the long-term effects of depression and its treatment on CRC risk and outcomes in IBS patients.
Core Tip: Young adults with depression and irritable bowel syndrome (IBS) do not have a significantly higher risk of colorectal cancer (CRC) compared to those without IBS. Further prospective studies are required to understand the long-term effects of depression and its treatment on CRC risk in IBS patients.
- Citation: Mellacheruvu SP, Lekkala SP, Chauhan S, Mohammed AS, Mundla SR, Shenoy A, Mohammed BK, Bawa J, Nallapothula S, Gurram P, Jain A, Desai R, Nayeem MM. Link between irritable bowel syndrome, depression, and colorectal cancer risk in young patients: Age-matched nationwide population-based study. World J Gastrointest Pathophysiol 2024; 15(3): 93408
- URL: https://www.wjgnet.com/2150-5330/full/v15/i3/93408.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v15.i3.93408
Irritable bowel syndrome (IBS) is a common disorder of gut-brain interaction characterized by abdominal pain, discomfort, and changes in bowel habits in the absence of known structural or biochemical abnormalities affecting 5%-10% of the population worldwide[1]. IBS affects people of all ages, but for unknown reasons, there appears to be a modest decline in occurrence as people get older[2]. Psychological distress and gastroenteritis are two well-known risk factors for IBS[2]. Fewer than half of the individuals with IBS seek treatment mainly because of the associated psychiatric disorders including major depression, anxiety, panic disorder post-traumatic stress disorder, etc[3]. On the other hand, a meta-analysis conducted by Jia et al[4] in 2017, concludes that there is a positive association between depression and the overall risk of cancer. Elevated concentrations of plasma proinflammatory cytokines associated with depression may mediate the neuroendocrinal, neural, and immune pathways that account for the increased risk of cancer in depressed patients. Chronic depression is also associated with decreased survival in cancer patients[5]
Colorectal cancer (CRC) is the third leading cause of cancer worldwide, recording 1.85 million cases per day[6]. The multifactorial nature of colorectal carcinogenesis and possible interactions between interactions have been studied earlier. One of the major concerns of IBS is the risk of developing CRC[2]. In a large United Kingdom database, IBS patients had a 1% possibility of being later diagnosed with CRC[7]. There have been extensive studies regarding the association between IBS and CRC. However, there is limited research on the specific relationship between depression, IBS, and CRC risk in young adults. Some studies have shown that individuals with IBS are at an increased risk for CRC due to the presence of chronic inflammation in the colon[5]. Depression is also associated with a higher risk of developing CRC, but the exact mechanism is not well understood[5]. In this study, we proposed to look for the association between IBS, depression, and CRC using the largest inpatient database publicly accessible in the United States (Figure 1).
The study sample was acquired from the 2019 National Inpatient Sample (NIS) database. This is a large administrative database funded by the Agency for Healthcare Research and Quality[8]. The prevalence and risk of CRC in hospitalized young, depressed adults with or without IBS were analyzed using this sample. The NIS database is the largest all-payer publicly available inpatient healthcare database in the United States. The NIS database includes more than 35 million weighted inpatient discharges and approximately 7 million unweighted inpatient discharges annually, which represents a 20% sample from 1000 hospitals in at least 40 states across the United States[9]. In our study, we used weighted nationwide data which provides national estimates divided into cohorts and analyzed for primary or secondary outcomes. We used the discharge weight provided by the database to generate national estimates, employing complex sample modules for accurate representation. All statistical analyses were conducted using IBM SPSS Statistics 25.0 software (IBM Corp, Armonk, New York).
Hospitalized young patients ages 18 to 44 with depression as primary or secondary diagnosis were extracted from the 2019 NIS database using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes including F32.0, F32.1, F32.3, F32.8, and F32.9. We used ICD-10-CM codes, including K58.x, to identify the history of IBS as one of the secondary diagnoses among young adults with depression. The ICD-10-CM codes utilized in our study have been verified and validated from previous studies[10,11]. Software codes provided by the Healthcare Cost and Utilization were used to recognize the other comorbidities and risk factors.
We compared baseline demographics and hospital characteristics between 2 age-matched (1:1) cohorts (without vs with a history of IBS) in hospitalized young patients with depression using the pearson χ2 test and Mann Whitney U test for categorical and continuous variables, respectively. Propensity matching was performed using nearest neighbor matching and a caliper width of 0.01. Absolute standardized difference between matched variables was obtained below 10% after matching. The percentages and means (SD) for the categorical and continuous variables, respectively, were quantified. Univariate analysis was used to determine the prevalence and risk of CRC in hospitalized young, depressed adults with a history of IBS.
Multivariate logistic regression was used to incorporate clinically important demographic and hospital factors such as age, sex, race, the median household income in the zip code, elective vs nonelective admissions, the primary expected payer, hospital bed size, a region of the hospital, control/ownership of the hospital, and location/teaching status of the hospital. Other patient risk factors such as diabetes mellitus, obesity, history of smoking, history of alcohol consumption, prior MI, drug abuse, anxiety, and related disorders were also adjusted to determine the risk of CRC-related inpatient encounters. The odds ratio (OR), 95% confidence interval (CI), and P value were used to express the results of the logistic regression. Since the NIS database does not contain patient identification data, we did not require approval from an institutional review board to carry out this investigation.
Our results comprised 28740 young adults with depression who were hospitalized in the United States. Of these, age-matched IBS+ group (n = 14370) and IBS- (n = 14370) were obtained. Patients from each cohort are age-matched (median age 36), primarily female (83.9% vs 65.8%, P < 0.001), and Caucasian (80.8% vs 67.9%, P < 0.001). The IBS+ cohort often consisted of patients from higher-income quartile households (21.1% vs 17.9%; P < 0.001). The IBS+ group had a higher prevalence of non-elective admissions (78.8% vs 77.1%, P < 0.001), Medicaid enrollees (40.1% vs 31.2%, P < 0.001), and admission in the South region (37% vs 36.5%, P < 0.001) (Table 1).
| Variables | Total young admissions with depression, n (%) | P value | |
| IBS- (n = 14370) | IBS+ (n = 14370) | ||
| Age (years) at admission | 36 (29-41) | 36 (29-41) | 1 |
| Median (IQR) | |||
| Sex | |||
| Male | 34.20 | 16.10 | < 0.001 |
| Female | 65.80 | 83.90 | |
| Race | |||
| White | 67.00 | 80.80 | < 0.001 |
| Black | 16.10 | 11.00 | |
| Hispanic | 11.40 | 5.60 | |
| Asian or Pacific Islander | 1.40 | 0.60 | |
| Native American | 1.00 | 0.40 | |
| Others | 3.20 | 1.70 | |
| Median household income national quartile for patient ZIP Code | |||
| 0-25th | 32.00 | 25.90 | < 0.001 |
| 26-50th | 26.10 | 25.70 | |
| 51-75th | 24.00 | 27.30 | |
| 76-100th | 17.90 | 21.10 | |
| Primary expected payer | |||
| Medicare | 13.90 | 15.00 | < 0.001 |
| Medicaid | 40.10 | 31.20 | |
| Private including HMO | 34.60 | 45.40 | |
| Location/teaching status of hospital | |||
| Rural | 7.70 | 7.40 | 0.029 |
| Urban non-teaching | 14.90 | 16.00 | |
| Urban teaching | 77.50 | 76.60 | |
| Comorbidities | |||
| Acquired immune deficiency syndrome | 1.00 | 0.40 | < 0.001 |
| Arthropathies | 3.90 | 6.20 | < 0.001 |
| Dementia | 0.30 | 0.10 | 0.001 |
| Hypertension, complicated | 7.90 | 6.40 | < 0.001 |
| Hypertension, uncomplicated | 21.30 | 23.00 | 0.001 |
| Diabetes with chronic complications | 9.70 | 9.70 | 1 |
| Diabetes without chronic complications | 6.50 | 6.90 | 0.193 |
| Hyperlipidemia | 12.00 | 14.60 | < 0.001 |
| Obesity | 23.60 | 27.70 | < 0.001 |
| Peripheral vascular disease | 1.30 | 1.60 | 0.014 |
| Prior MI | 1.70 | 0.70 | < 0.001 |
| Chronic pulmonary disease | 16.30 | 26.10 | < 0.001 |
| Hypothyroidism | 7.80 | 11.20 | < 0.001 |
| Other thyroid disorders | 1.10 | 2.00 | < 0.001 |
| Prior TIA/Stroke without Neurologic deficit | 2.10 | 2.50 | 0.017 |
| Prior VTE | 5.00 | 5.80 | 0.002 |
| Cancer | 2.20 | 2.00 | 0.409 |
| Anxiety and fear related disorders | 54.60 | 68.60 | < 0.001 |
| Psychoses | 4.20 | 4.50 | 0.312 |
| Bipolar disorder | 0.70 | 1.50 | < 0.001 |
| Borderline personality disorder | 1.90 | 2.90 | < 0.001 |
| Alcohol abuse | 12.00 | 6.30 | < 0.001 |
| Tobacco use disorder | 32.80 | 26.10 | < 0.001 |
| Drug abuse | 17.80 | 11.20 | < 0.001 |
Young adults with IBS are more likely to have anxiety and fear-related disorder, bipolar disorder, and borderline personality disorder (68.6% vs 54.6%, P < 0.001; 1.5% vs 0.7%, P < 0.001; 2.9% vs 1.9%, P < 0.01). However, the IBS- the group has considerably higher rates of drug misuse, alcohol abuse, and tobacco use disorder than the IBS+ cohort (17.8% vs 11.2%, P < 0.001; 12.0% vs 6.3%, P < 0.001; 32.8% vs 26.1%, P < 0.001). Among the Cardiovascular comorbidities, peripheral vascular disorders were significantly higher in the IBS+ cohort (1.6% vs 1.3%, P < 0.001); while prior MI rates were higher in the IBS- cohort (1.7% vs 0.7%, P < 0.001%). Other comorbidities such as endocrine complications, hypertension, obesity, hematological issues, and musculoskeletal and pulmonary complications are shown in Table 1.
In both cohorts, the rate of CRC was similar [IBS+ n = 25 (0.17%) vs IBS- n = 35 (0.24%), P = 0.196]. The odds of developing CRC in the IBS cohort were not statistically different from the IBS-cohort (OR 0.71, 95%CI 0.23-2.25, P = 0.565). The OR was also shown to be non-significant after controlling for baseline sociodemographic and hospital variables as well as pertinent cardiovascular, pulmonary, endocrine, psychiatric, neurological, and infectious comorbidities (OR 0.89, 95%CI 0.21-3.83, P = 0.871) (Table 2).
| IBS- (n = 14370) | IBS+ (n = 14370) | P value | |
| Rate of CRC | 0.2% | 0.2% | 0.196 |
| Logistic regression models | Odds ratio | 95%CI (LL-UL) | Adjusted P value |
| Model 1-Univariate | 0.71 | 0.23-2.25 | 0.565 |
| Model 2-Adjusted for baseline sociodemographic characteristics + hospital characteristics | 0.73 | 0.22-2.41 | 0.610 |
| Model 31-Model 2 + relevant preexisting comorbidities | 0.89 | 0.21-3.83 | 0.871 |
To our knowledge, this is the first United States study utilizing nationwide data and analyzing the association of CRC in young adults with depression and IBS. Our findings show that having both IBS and depression does not significantly raise the risk of getting CRC.
Depression has been linked to an increased risk of cancer, likely due to innate immune activation and inflammation, which are involved in the pathophysiology of both these conditions[5]. In particular, a 20% increased risk of CRC [hazard ratio (HR) = 1.21, 95%CI = 1.09-1.48] has been observed in patients with severe depressive symptoms[12]. Patients with IBS often report anxiety and depression[13], but the link between IBS and CRC risk remains understudied[14].
Patients with IBS often report anxiety and depression[13], but the link between IBS and CRC risk remains understudied[14]. Studies have shown that IBS does not raise the likelihood of getting cancer in general. A major cohort study that included 449595 individuals from England, Wales, and Scotland found that IBS did not increase the overall risk of cancer. The adjusted HR (aHR) for overall cancer was 0.97 (95%CI = 0.93-1.00, P = 0.062) for those with IBS compared to those without IBS. Furthermore, the risk of CRC was even lower in IBS patients (aHR = 0.73, 95%CI = 0.62-0.86)[15]. Similarly, a Danish nationwide cohort study that included 57, 851 patients with IBS showed no evidence of increased risk of CRC 1-10 years after the diagnosis of IBS. However, the risk was higher in the initial 3 months, with colon cancer standardized ratio at 8.42 (95%CI = 6.48-10.75) and rectal cancer at 4.81 (95%CI = 2.85-7.60). The authors attributed this finding to diagnostic confusion secondary to overlapping symptoms between IBS and CRC[16]. Several other studies have also shown that IBS is not associated with an increased risk of long-term development of CRC[14,17,18]. However, it is important to note that a Taiwanese study with 39384 participants conducted in a community-based CRC screening program revealed that, after adjusting for factors such as age, gender, and family history of CRC, patients with IBS had a higher risk of developing only colorectal adenomas (21%, aHR = 1.21, 95%CI = 1.02-1.42) and not invasive CRC (aHR = 1.20; 95%CI = 0.94-1.53) as compared to IBS- cohort[19].
Our study had the limitation of only being conducted among young adults ages 18 to 44, while the median age of CRC diagnosis is 70 for men and 72 for women[20]. As a result, our study might have only evaluated the potential link between IBS and early-onset CRC, but not the long-term impact of IBS on colon cancer. Moreover, medication data was not available. The administrative nature of the dataset may include some eros due to over-coding or under coding instances.
In summary, our findings suggest that IBS is not associated with an increased risk of CRC in young adults who also have depression. However, more prospective studies are needed to confirm these results and to better understand the relationship between long-term depression in young individuals and CRC in the presence of IBS.
| 1. | Black CJ. Review article: Diagnosis and investigation of irritable bowel syndrome. Aliment Pharmacol Ther. 2021;54 Suppl 1:S33-S43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Rey E, Talley NJ. Irritable bowel syndrome: novel views on the epidemiology and potential risk factors. Dig Liver Dis. 2009;41:772-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Lydiard RB. Irritable bowel syndrome, anxiety, and depression: what are the links? J Clin Psychiatry. 2001;62 Suppl 8:38-45; discussion 46. [PubMed] |
| 4. | Jia Y, Li F, Liu YF, Zhao JP, Leng MM, Chen L. Depression and cancer risk: a systematic review and meta-analysis. Public Health. 2017;149:138-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 5. | Currier MB, Nemeroff CB. Depression as a risk factor for cancer: from pathophysiological advances to treatment implications. Annu Rev Med. 2014;65:203-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Mattiuzzi C, Sanchis-Gomar F, Lippi G. Concise update on colorectal cancer epidemiology. Ann Transl Med. 2019;7:609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 201] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 7. | García Rodríguez LA, Ruigómez A, Wallander MA, Johansson S, Olbe L. Detection of colorectal tumor and inflammatory bowel disease during follow-up of patients with initial diagnosis of irritable bowel syndrome. Scand J Gastroenterol. 2000;35:306-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 94] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Khera R, Krumholz HM. With Great Power Comes Great Responsibility: Big Data Research From the National Inpatient Sample. Circ Cardiovasc Qual Outcomes. 2017;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 223] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 9. | Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP). Feb 18, 2023. Available from: https://www.ahrq.gov/data/hcup/index.html. |
| 10. | Kessing LV. Severity of depressive episodes according to ICD-10: prediction of risk of relapse and suicide. Br J Psychiatry. 2004;184:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Häuser W, Marschall U, Layer P, Grobe T. The Prevalence, Comorbidity, Management and Costs of Irritable Bowel Syndrome. Dtsch Arztebl Int. 2019;116:463-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Kiridly-Calderbank JF, Sturgeon SR, Kroenke CH, Reeves KW. Antidepressant Use and Risk of Colorectal Cancer in the Women's Health Initiative. Cancer Epidemiol Biomarkers Prev. 2018;27:892-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Banerjee A, Sarkhel S, Sarkar R, Dhali GK. Anxiety and Depression in Irritable Bowel Syndrome. Indian J Psychol Med. 2017;39:741-745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Wu X, Wang J, Ye Z, Wang J, Liao X, Liv M, Svn Z. Risk of Colorectal Cancer in Patients With Irritable Bowel Syndrome: A Meta-Analysis of Population-Based Observational Studies. Front Med (Lausanne). 2022;9:819122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Wu S, Yuan C, Liu S, Zhang Q, Yang Z, Sun F, Zhan S, Zhu S, Zhang S. Irritable Bowel Syndrome and Long-Term Risk of Cancer: A Prospective Cohort Study Among 0.5 Million Adults in UK Biobank. Am J Gastroenterol. 2022;117:785-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Nørgaard M, Farkas DK, Pedersen L, Erichsen R, de la Cour ZD, Gregersen H, Sørensen HT. Irritable bowel syndrome and risk of colorectal cancer: a Danish nationwide cohort study. Br J Cancer. 2011;104:1202-1206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Hsiao CW, Huang WY, Ke TW, Muo CH, Chen WT, Sung FC, Kao CH. Association between irritable bowel syndrome and colorectal cancer: a nationwide population-based study. Eur J Intern Med. 2014;25:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Canavan C, Card T, West J. The incidence of other gastroenterological disease following diagnosis of irritable bowel syndrome in the UK: a cohort study. PLoS One. 2014;9:e106478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Chang HC, Yen AM, Fann JC, Chiu SY, Liao CS, Chen HH, Yang KC, Chen LS, Lin YM. Irritable bowel syndrome and the incidence of colorectal neoplasia: a prospective cohort study with community-based screened population in Taiwan. Br J Cancer. 2015;112:171-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Glover M, Mansoor E, Panhwar M, Parasa S, Cooper GS. Epidemiology of Colorectal Cancer in Average Risk Adults 20-39 Years of Age: A Population-Based National Study. Dig Dis Sci. 2019;64:3602-3609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |