Copyright
©The Author(s) 2021.
World J Gastrointest Pathophysiol. Jul 22, 2021; 12(4): 59-83
Published online Jul 22, 2021. doi: 10.4291/wjgp.v12.i4.59
Published online Jul 22, 2021. doi: 10.4291/wjgp.v12.i4.59
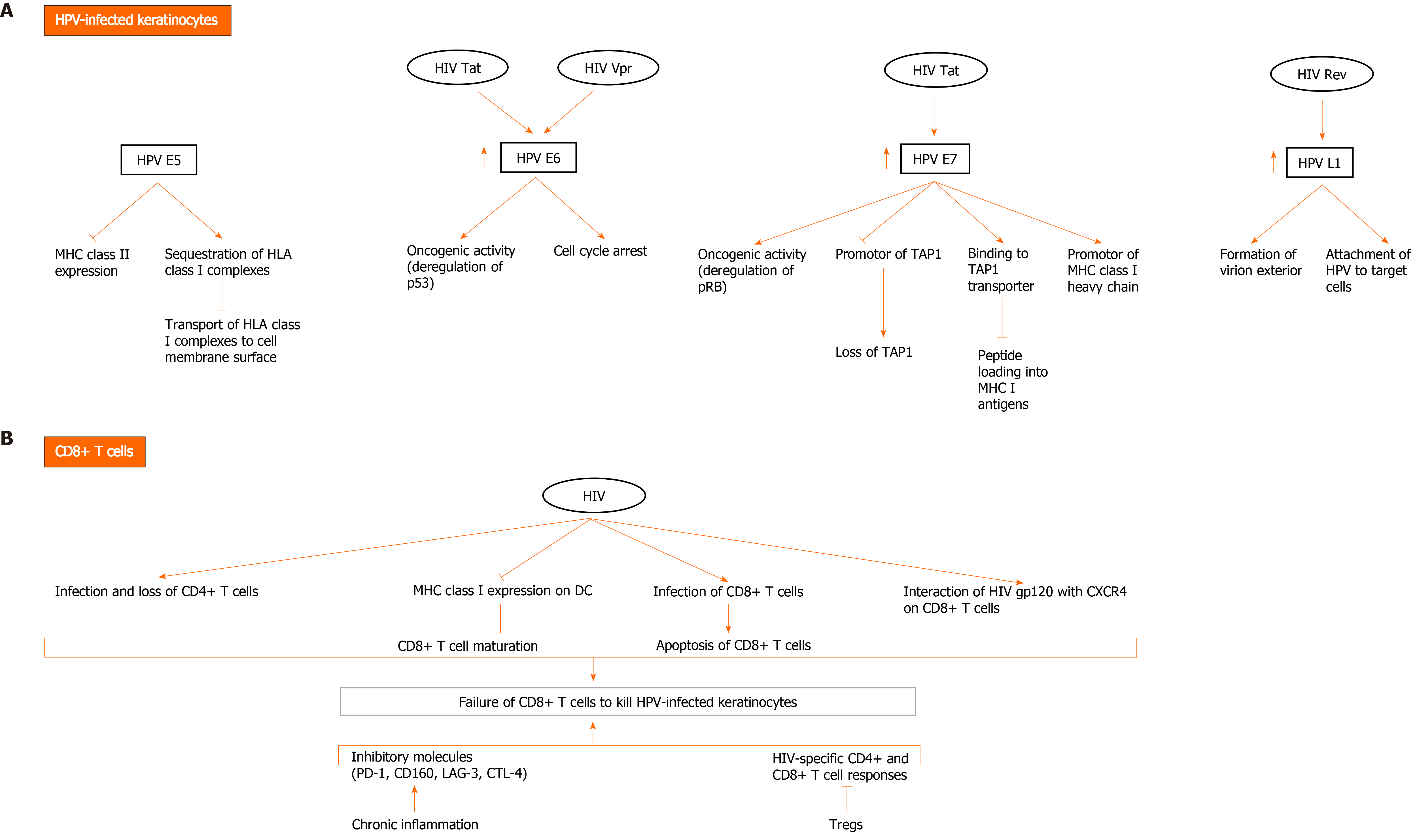
Figure 2 Possible mechanisms of direct and indirect interactions between human papillomavirus and human immunodeficiency virus to evade the immune system and mediate human papillomavirus carcinogenesis.
A: Human immunodeficiency virus (HIV) and human papillomavirus (HPV) contribute to HPV-related carcinogenesis and evasion of immune cells through several mechanisms involving direct interaction between HIV and HPV proteins in HPV-infected keratinocytes. HPV E5 oncoprotein downregulates major histocompatibility complex (MHC) II expression and sequesters human leukocyte antigen (HLA) class I complexes in keratinocytes, thereby blocking transport of HLA class I complexes to cell membrane surface. HPV E6 exerts oncogenic effects, mainly through deregulation of p53 and induction of cell cycle arrest. HPV E7 exerts oncogenic activity through deregulating pRB. It promotes downregulation of MHC class I expression through downregulating peptide transporter 1 associated with antigen processing (TAP1) and binding to TAP transporter, and thus inhibiting peptide loading into MHC I antigens. It also downregulates promotor of MHC I heavy chain. Importantly, HIV Tat upregulates the expression of HPV16 E6 and E7, enhancing their oncogenic effects. It also increases the expression of HPV L1. HIV Rev indirectly upregulates HPV L1 expression. HIV Vpr interacts with HPV E6 protein to induce cell cycle arrest and oncogenesis; B: HIV infection diminishes immune response to HPV infection, resulting in HPV persistence and pathogenesis. Failure of CD8+ T cells to kill HPV-infected keratinocytes is a major event in HIV and HPV co-infection and occurs through multiple mechanisms. In addition to loss of CD4+ T cells due to infection with HIV, downregulation of MHC I expression on dendritic cells (DC) by HIV inhibits CD8+ T cell maturation. A small fraction of CD8+ T cells become infected with HIV and are susceptible to the direct cytotoxic effects of the virus. Moreover, HIV gp120 interacts with CXCR4 on CD8+ T cells and affects their function. Other factors also contribute to inhibition of HIV-specific CD4+ and CD8+ T cell responses and include activation of Tregs and the expression of inhibitory molecules (programmed death-1 [PD-1], CD160, lymphocyte activation gene 3, cytotoxic T lymphocyte antigen-4 [CTLA-4]) by CD8+ T cells during chronic inflammation induced by HIV.
- Citation: Al Bitar S, Ballouz T, Doughan S, Gali-Muhtasib H, Rizk N. Potential role of micro ribonucleic acids in screening for anal cancer in human papilloma virus and human immunodeficiency virus related malignancies. World J Gastrointest Pathophysiol 2021; 12(4): 59-83
- URL: https://www.wjgnet.com/2150-5330/full/v12/i4/59.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v12.i4.59