Published online Mar 28, 2012. doi: 10.4329/wjr.v4.i3.121
Revised: February 20, 2012
Accepted: February 27, 2012
Published online: March 28, 2012
Gastric varices are usually associated with a gastro-renal (G-R) shunt. However, the gastric varices described in this case report were not associated with a G-R shunt. The inflow vessel was the posterior gastric vein and the outflow vessels were the narrow inferior phrenic vein and the dilated cardio-phrenic vein. First, percutaneous transhepatic obliteration of the posterior gastric vein was performed, but the gastric varices remained patent. Then, micro-balloon catheterization of the subphrenic vein was carried out via the jugular vein, pericardial vein and cardio-phrenic vein, however, micro-balloon-occluded inferior phrenic venography followed by micro-coil embolization of the cardio-phrenic vein revealed no delineation of gastric varices resulting in no further treatment. Thereafter, as a gastro-subphrenic-intercostal vein shunt developed, a micro-balloon catheter was advanced to the gastric varices via the intercostal vein and balloon-occluded retrograde transvenous obliteration (BRTO) was performed resulting in the eradication of gastric varices. BRTO for gastric varices via the intercostal vein has not previously been documented.
-
Citation: Minamiguchi H, Kawai N, Sato M, Ikoma A, Sawa M, Sonomura T, Sahara S, Nakata K, Takasaka I, Nakai M. Balloon-occluded retrograde transvenous obliteration for gastric varices
via the intercostal vein. World J Radiol 2012; 4(3): 121-125 - URL: https://www.wjgnet.com/1949-8470/full/v4/i3/121.htm
- DOI: https://dx.doi.org/10.4329/wjr.v4.i3.121
Once gastric varices rupture, bleeding is extremely dangerous and sometimes fatal because the volume of hemorrhage is often large. Treatment procedures for gastric varices such as surgical portosystemic shunt, percutaneous transhepatic obliteration (PTO) and transjugular intrahepatic portosystemic shunt may be effective[1]. However, balloon-occluded retrograde transvenous obliteration (BRTO), which was first reported by Kanagawa et al[2], is becoming a well-established treatment for gastric varices, whether hemorrhagic or prophylactic, as BRTO is less invasive than the other procedures and offers good control even if hepatic function is poor. During BRTO, the sclerosant is infused into the gastric varices under occlusion of the draining vessel by balloon inflation. Gastric varices most commonly have a spontaneous gastro-renal (G-R) shunt with the left adrenal vein targeted as the main draining vessel by balloon inflation. However, gastric varices which are not associated with a G-R shunt have been observed[3,4]. The outflow vessels of gastric varices without a G-R shunt such as the inferior phrenic vein, cardio-phrenic vein, pericardial vein, retroperitoneal vein and intercostal vein are anatomically listed[5]. We present a patient who underwent BRTO performed by catheterization via the intercostal vein for gastric varices with a gastro-subphrenic-intercostal shunt.
The institutional review board at our hospital did not require approval for this retrospective case.
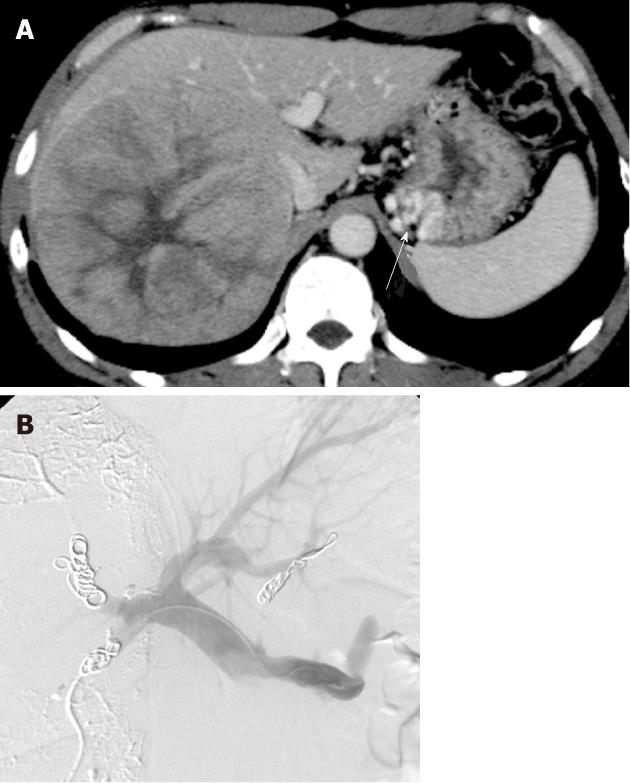
A 55-year-old man with chronic liver disorder due to hepatitis B virus infection was introduced to our hospital because the family doctor had diagnosed a liver tumor. Laboratory data revealed Child-Pugh A liver dysfunction (Child-Pugh score 5) and high α-fetoprotein (AFP) and protein induced vitamin K absence or antagonist II (PIVKA-II) values of 230 ng/mL and 273780 mAU/mL, respectively. Dynamic computed tomography (CT) demonstrated gastric varices with no G-R shunt and a large hepatocellular carcinoma (HCC) of 13 cm in diameter in the right lobe (Figure 1A).
In the multidisciplinary conference which included surgeons, interventional radiologists and hepatologists, the patient was scheduled to receive PTO for gastric varices, percutaneous transhepatic portal vein embolization (PTPE) and thereafter, right hepatectomyas the volume of the medial and lateral segment was too small to tolerate right lobe hepatectomy, and PTPE was anticipated to deteriorate gastric varices due to secondary portal hypertention[6-8]. Under ultrasound guidance, the posterior inferior subsegment of the portal vein branch was punctured using an 18 gauge needle and a 4 Fr sheath was inserted. Percutaneous transhepaticsplenography using a 4 Fr pigtail catheter revealed that the inflow vessel of the gastric varices was the posterior gastric vein and the outflow vessel was the dilated cardio-phrenic vein and narrow inferior phrenic vein. Then, PTO of the posterior gastric vein for gastric varices was attempted. A micro-balloon catheter was advanced through the sheath to the posterior gastric vein and under micro-balloon inflation, 50% glucose, 5% ethanolamine oleate-iopamidol (EOI) and microcoils were used for occlusion of the posterior gastric vein. PTPE of the anterior and posterior segments using lipiodol, gelatin sponge particles and microcoils was conducted via the same transhepatic access route (Figure 1B). However, enhanced CT one month later demonstrated that patent gastric varices remained, and the medial and lateral segments did not enlarge as expected. Laboratory tests also revealed no improvement in the indocyanine green retention ratio of 15 min (ICG-R15) (9% to 8%). Therefore, instead of surgical hepatectomy, the patient underwent single photon emission computed tomography-based three-dimensional conformal radiotherapy (SPECT-B-3D-CRT) targeting the large HCC to a total dose of 45 Gy/18 fractions with transcatheter arterial chemoembolization (TACE) resulting in tumor shrinkage with marked decreases in AFP and PIVKA-II values (18.7 ng/mL and 120 mAU/mL, respectively).
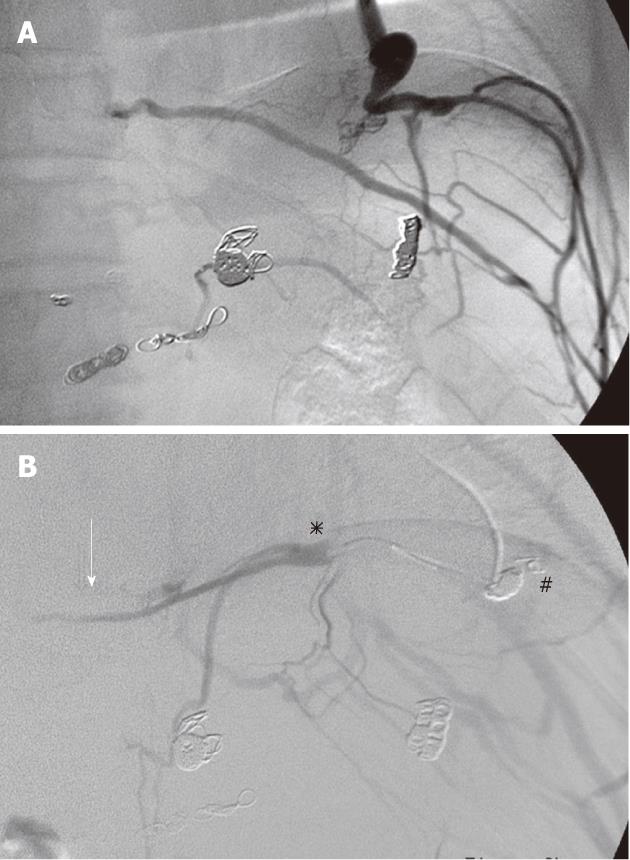
Follow-up gastrointestinal endoscopy demonstrated the presence of gastric varices and a new small gastric cancer. Endoscopic ultrasoundscopy revealed that the gastric cancer was limited to the submucosal layer, however, gastric varices were observed beneath the gastric cancer. The surgeon asked for the gastric varices to be eradicated in order to undertake endoscopic submucosal dissection (ESD) to remove the early gastric cancer. Dynamic CT demonstrated gastric varices with no G-R shunt, however, the presence of the narrow left inferior phrenic vein and dilated cardio-phrenic vein were noted. Catheterization of the inferior phrenic vein was attempted but was difficult due to the narrowness of the vein. We inserted a micro-balloon catheter into the pericardial vein via the left jugular vein and left innominate vein. Micro-balloon-occluded pericardial venography (Figure 2A) revealed the narrow subphrenic vein, dilatation of the cardio-phrenic vein and the subphrenicbranch veins but did not delineate the gastric varices. We then inserted a balloon catheter into the left subphrenic vein followed by coil embolization of the cardio-phrenic vein to reduce the collateral pathways. However, micro-balloon-occluded subphrenic venography (Figure 2B) revealed still no delineation of gastric varices. Further catheterization using the micro-balloon catheter toward the gastric vein was difficult. As growth of the early gastric cancer was slow, we waited one month anticipating development of the inferior phrenic vein and hoped that simultaneous micro-balloon inflations of the subphrenic vein and pericardial vein might lead to delineation of the gastric varices.
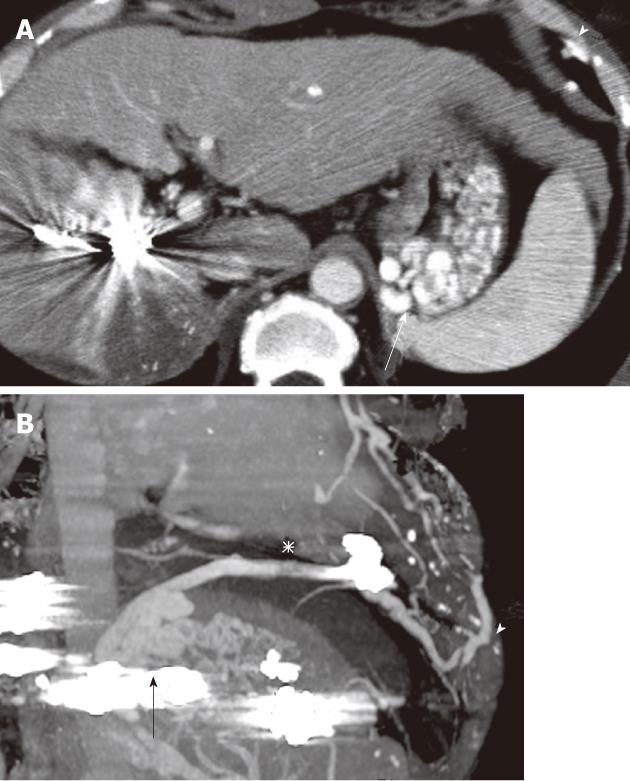
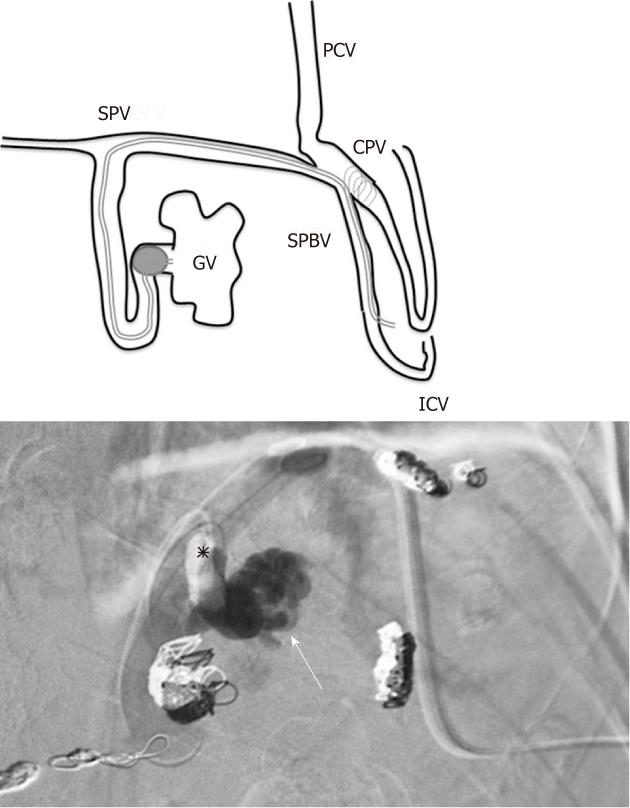
Beyond our expectation, axial and sagittal oblique images of multi-planar reconstruction enhanced CT medium one month later (Figure 3), revealed the gastric varices draining to the development gastrosubphrenic-intercostal shunt. BRTO for gastric varices via the intercostal vein was then carried out. Under ultrasound guidance, the 7th inter-costal vein was punctured using an 18-gauge needle, and a 6 French guiding catheter (ELWAY C2 type, Terumo Clinical Supply, Gifu, Japan) was inserted followed by advancement of a 0.035 inch guidewire (Surf, Piolax, Yokohama, Japan). The patient complained of slight pain during catheterization because the catheter contacted with the rib and friction arose during respiration. Drip infusion of the analgesic (pentazocine hydrochloride) was effective in relieving pain. A micro-balloon catheter (Iiguman, 7 mm diameter, Fuji System, Fukushima, Japan) was coaxially inserted through the guiding catheter and advanced using a microwire (HI-LEX, Hyogo, Japan) to the retroperitoneal vein which directly drained the gastric varices via the subphrenic vein. Micro-balloon inflation was not enough to interrupt the blood flow because the diameter of the draining vein was too large. Thus, a micro-balloon was inserted into the neck of the gastric varices and then inflated, resulting in the stagnation of blood flow. BRTO was conducted using 5% EOI mixed with 10% ethanolamine oleate (Oldamine, Fuji Chemical, Toyama, Japan) and the same dose of contrast medium (Iopamidol, 300 mg iodine) (Figure 4). Intravenous drip infusion of 4000 units of human hepatoglobin (Benesis, Kyoto, Japan) was administered for approximately 30 min before BRTO. To reduce the dose of the sclerosing agent to a minimum, 10 mL of 50% glucose was infused initially and a total of 7.5 mL of 5% EOI was infused into the gastric varices via the microcatheter under balloon inflation. However, we realized that stagnation of EOI was temporary due to the presence of other small outflow channels. Ethanol 99% mixed with lipiodol (4:1) was also injected to occlude the channels. After confirmation of the disappearance of the channels, another 7.5 mL of 5% EOI was infused resulting in satisfactory stagnation. Micro-balloon inflation was maintained overnight in the ward, and the thrombosed gastric varices were confirmed the following day by contrast-enhanced CT. Thereafter, the puncture route of the intercostal vein was occluded completely using microcoils (COOK Europe, Bjaeverskov, Denmark) of 2 to 6 mm in diameter. Enhanced CT the following day revealed no delineation of gastric varices (Figure 5), which allowed the patient to receive ESD.
Gastric varices draining into a G-R shunt occur with a high incidence of 84 to 97%[3,5]. When a G-R shunt, as the main draining vein from gastric varices is present, collateral outflows such as the left subphrenic vein, pericardio-phrenic vein, gonadal vein and retroperitoneal veins are often observed. These collateral outflows are anticipated to develop in cases of gastric varices without a G-R shunt. Kameda et al[3] demonstrated that as the draining vessel from gastric varices without a G-R shunt, the subphrenic vein is the most important followed by the pericardial vein and paraesophageal vein. In the present study involving a patient with gastric varices without a GR shunt, the inflow vessel was the posterior gastric vein and the outflow vessels were the dilated cardio-phrenic vein and the narrow subphrenic vein. The narrow subphrenic vein and coil embolization of the cardio-phrenic vein developed the draining route of the gastrosubphrenic-intercostal shunt.
Chikamori et al[9] attempted to treat gastric varices with a gastropericardiac shunt using PTO of the posterior gastric vein which resulted in the successful shrinkage of gastric varices. Despite PTO of the posterior gastric vein, the occlusion of gastric varices was not satisfactory in the present case. In order to perform ESD for early gastric cancer safely, the eradication of gastric varices was requested. Subphrenic venography under inflation of the micro-balloon catheter followed by coil embolization of the cardio-phrenic vein did not lead to delineation of gastric varices. One month later, following the development of a gastrosubphrenic-intercostal shunt, BRTO via the intercostal vein was performed resulting in complete thrombosis of gastric varices. To the best of our knowledge, BRTO for gastric varices via the intercostal vein route has not been documented.
The insertion of a catheter into an intact intercostal vein is generally difficult because of its narrow diameter. In this case, a dilated intercostal vein developed and under ultrasound guidance, puncture and catheter insertion were performed without difficulty. The friction of the catheter on the rib during respiration caused slight pain which resolved with the administration of analgesics. Pressure hemostasis by hand at the intercostal vein puncture site after withdrawal of the catheter was difficult. Microcoil embolization was then carried out adjacent to the puncture site resulting in no recurrent bleeding.
This patient suffered from a giant HCC of 13 cm in diameter. Shiraiet al[10] reported that the combination of SPECT-B-3D-CRT and TACE achieved a median survival of 13.5 mo in HCC patients with portal vein tumor thrombus which was comparable to that (13.6 mo) reported in a surgical hepatectomy series. The patient survived more than 2 years following SPECT-B-3D-CRT and TACE.
We conclude that in this case, the draining route of the gastrosubphrenic-intercostal shunt was developed by the narrow subphrenicvein and coil embolization of the cardio-phrenic vein, and BRTO for gastric varices via the intercostal vein resulted in eradication of gastric varices.
Peer reviewer: Hadi Rokni Yazdi, MD, Associate Professor, Department of Radiology, Central Radiology, Imam Khomeini Hospital, Tehran University of Medical Sciences, Keshavarz Blvd, Tehran 1419733141, Iran
S- Editor Cheng JX L- Editor Webster JR E- Editor Xiong L
| 1. | Rössle M, Deibert P, Haag K, Ochs A, Olschewski M, Siegerstetter V, Hauenstein KH, Geiger R, Stiepak C, Keller W. Randomised trial of transjugular-intrahepatic-portosystemic shunt versus endoscopy plus propranolol for prevention of variceal rebleeding. Lancet. 1997;349:1043-1049. [PubMed] [Cited in This Article: ] |
| 2. | Kanagawa H, Mima S, Kouyama H, Gotoh K, Uchida T, Okuda K. Treatment of gastric fundal varices by balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 1996;11:51-58. [PubMed] [Cited in This Article: ] |
| 3. | Kameda N, Higuchi K, Shiba M, Kadouchi K, Machida H, Okazaki H, Tanigawa T, Watanabe T, Tominaga K, Fujiwara Y. Management of gastric fundal varices without gastro-renal shunt in 15 patients. World J Gastroenterol. 2008;14:448-453. [PubMed] [Cited in This Article: ] |
| 4. | Kiyosue H, Mori H, Matsumoto S, Yamada Y, Hori Y, Okino Y. Transcatheter obliteration of gastric varices. Part 1. Anatomic classification. Radiographics. 2003;23:911-920. [PubMed] [Cited in This Article: ] |
| 5. | Maeda H, Hirota S, Yamamoto S, Kobayashi K, Arai K, Miyamoto Y, Fukuda T, Sugimoto K, Nakao N. Radiologic variations in gastrorenal shunts and collateral veins from gastric varices in images obtained before balloon-occluded retrograde transvenous obliteration. Cardiovasc Intervent Radiol. 2007;30:410-414. [PubMed] [Cited in This Article: ] |
| 6. | Abulkhir A, Limongelli P, Healey AJ, Damrah O, Tait P, Jackson J, Habib N, Jiao LR. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247:49-57. [PubMed] [Cited in This Article: ] |
| 7. | Tanaka H, Hirohashi K, Kubo S, Shuto T, Higaki I, Kinoshita H. Preoperative portal vein embolization improves prognosis after right hepatectomy for hepatocellular carcinoma in patients with impaired hepatic function. Br J Surg. 2000;87:879-882. [PubMed] [Cited in This Article: ] |
| 8. | Arai H, Abe T, Takagi H, Mori M. Efficacy of balloon-occluded retrograde transvenous obliteration, percutaneous transhepatic obliteration and combined techniques for the management of gastric fundal varices. World J Gastroenterol. 2006;12:3866-3873. [PubMed] [Cited in This Article: ] |
| 9. | Chikamori F, Kuniyoshi N, Kawashima T, Shibuya S, Takase Y. Percutaneous transhepatic obliteration for isolated gastric varices with gastropericardiac shunt: case report. Abdom Imaging. 2006;31:249-252. [PubMed] [Cited in This Article: ] |
| 10. | Shirai S, Sato M, Suwa K, Kishi K, Shimono C, Sonomura T, Kawai N, Tanihata H, Minamiguchi H, Nakai M. Feasibility and efficacy of single photon emission computed tomography-based three-dimensional conformal radiotherapy for hepatocellular carcinoma 8 cm or more with portal vein tumor thrombus in combination with transcatheter arterial chemoembolization. Int J Radiat Oncol Biol Phys. 2010;76:1037-1044. [PubMed] [Cited in This Article: ] |