Copyright
©The Author(s) 2024.
World J Radiol. Aug 28, 2024; 16(8): 337-347
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.337
Published online Aug 28, 2024. doi: 10.4329/wjr.v16.i8.337
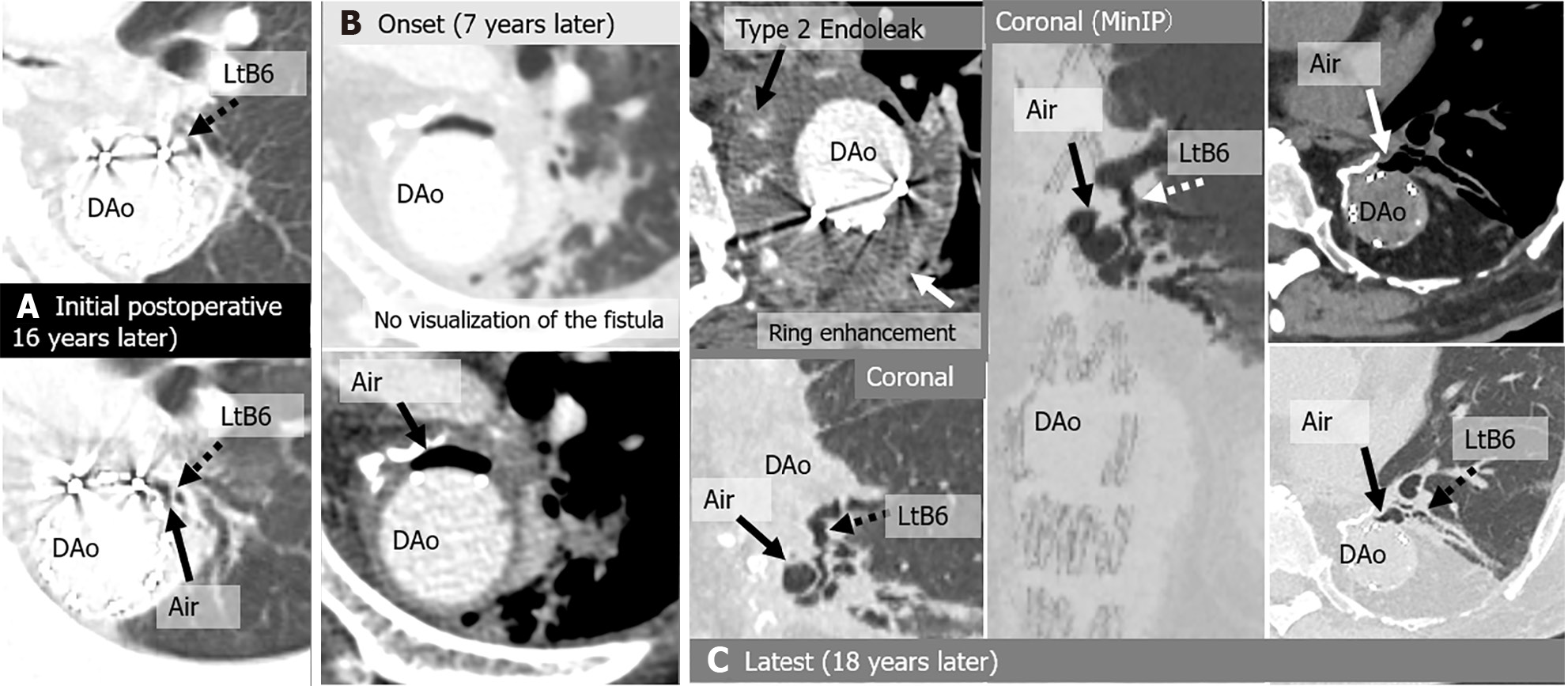
Figure 6 Aortobronchial fistula in a 57-year-old asymptomatic man, a history of bronchioles 3 years earlier for a pseudoaneurysm after thoracoabdominal aorta replacement 16 years earlier for an aneurysm.
Seven years after the first detection of peri-graft air, he developed fever and hemoptysis due to graft infection and a type 2 endoleak, and underwent aortic-arch-to-descending-aorta replacement, bronchopulmonary artery fistula closure, and intrathoracic omental repair. Ten years after the reoperation, the patient developed a pseudoaneurysm and underwent thoracic endovascular aortic repair (TEVAR). A: Initial computed tomography (CT) images show air shadow in the intra-aortic peri-graft space (arrow) and dilated peripheral bronchus (left B6) communicating with peri-graft air (arrow); B: Onset CT, 7 years after the initial CT images show increased peri-graft air (arrow), but there is no direct connection between bronchioles and peri-graft air. Axial enhanced CT demonstrates a Type 2 endoleak and ring enhancement; C: Latest CT, 18-year follow-up after initial CT images show residual peri-graft air and dilated peripheral bronchus (left B6) communicating with peri-graft air (arrow). No complications occurred during the follow-up period of 1.5 years after TEVAR for a pseudoaneurysm. DAo: Descending aorta; Lt: Left; MinIP: Minimum intensity projection.
- Citation: Tsuchiya N, Inafuku H, Yogi S, Iraha Y, Iida G, Ando M, Nagano T, Higa S, Maeda T, Kise Y, Furukawa K, Yonemoto K, Nishie A. Direct visualization of postoperative aortobronchial fistula on computed tomography. World J Radiol 2024; 16(8): 337-347
- URL: https://www.wjgnet.com/1949-8470/full/v16/i8/337.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i8.337